Миома матки (ММ) – одно из самых часто встречающихся заболеваний в практике акушера-гинеколога. В настоящее время доказано, что ММ – это моноклональная опухоль, результат патологического деления одной первичной клетки-предшественницы [1–3]. Распространенность указанной нозологии среди женщин в возрасте до 50 лет достигает 70–80% [4]. В то же время среди пациенток до 18 лет ее частота – менее 1% [5]. В отечественной и зарубежной литературе встречаются лишь единичные публикации, посвященные ММ у девочек [5–9]. Следует подчеркнуть, что большинство работ описывают клинические случаи диагностики и лечения ММ больших и гигантских размеров.
Так, в работе 2012 г. суммирован 15-летний опыт отечественных авторов наблюдения более 12 000 девочек с гинекологической патологией, из них только у 3 больных была выявлена ММ (0,025%). Возраст пациенток составил от 15 до 17 лет, размеры узлов колебались от 2 до 4,5 см. До поступления в стационар девочки наблюдались по месту жительства в среднем около 2 лет. Все девочки жаловались на дисменорею. Одна девочка поступила экстренно с рождающимся миоматозным узлом, ей было произведено его удаление. Две другие – поступили планово, в связи с отмеченным ростом узлов. Им выполнена миомэктомия. Одной девочке – из мини-лапаротомного доступа, другой – с использованием методики Single Iscition Laparoscopic Surgery. У обеих прооперированных пациенток ММ сочеталась с аденомиозом. При патоморфологическом исследовании узлов у 3 указанных пациенток подтверждена лейомиома матки [8].
Кроме того, в 2015 г. Moroni et al. выполнили систематический обзор [5]. Исследователи проанализировали 19 случаев ММ у девочек-подростков, опубликованных в период 1969–2014 гг. Возраст девочек варьировал от 14 до 17 лет. У большинства пациенток ММ (87,5%) были симптомными. Из них в 10 (10/18) случаях ММ сопровождали аномальные маточные кровотечения, в 6 (6/18) случаях девочки жаловались на тазовую боль, в 8 – на увеличение живота в объеме. У 3 пациенток отмечались симптомы, связанные с железодефицитной анемией, в 2 случаях потребовалось переливание компонентов крови. Размер образований варьировал от 3 до 30 см (в среднем 12.28 см). Не представлено данных о методе лечения в 2/19 случаях. У 1 пациентки (1/19) избрана выжидательная тактика. Миомэктомия выполнена в 16/19 случаев. В том числе 2 (2/16) пациенткам произведена гистерорезектоскопия, в остальных случаях оперативное лечение – из лапаротомного доступа (14/16). Кроме того, у одной пациентки выполнена роботизированная миомэктомия по поводу рецидива ММ через 7 месяцев. В одном случае выполнена гистерэктомия с придатками с обеих сторон. Ни в одном случае в данном систематическом обзоре не применяли медикаментозное лечение, эмболизацию маточных артерий, высокоинтенсивную фокусированную ультразвуковую абляцию, как и возможность выполнения оперативного лечения лапароскопическим доступом. Позднее в литературе в последние 5 лет появились в печати клинические случаи оперативного лечения ММ у девочек-подростков путем миомэктомии из лапароскопического доступа [6, 7].
 Описание
Описание
В кабинет гинеколога детей и подростков научно-поликлинического отделения ФГБУ НМИЦ АГП им. В.И. Кулакова (далее Центр) в ноябре 2020 г. с жалобами на обильные болезненные менструации, общую слабость и увеличение живота в объеме (рис. 1) совместно с родителями обратилась пациентка в возрасте 16 лет. По месту жительства (Кострома) по данным ультразвукового исследования (УЗИ) органов малого таза (ОМТ) выявлена киста правого яичника больших размеров. Для уточнения диагноза пациентка направлена на магнитно-резонансную томографию (МРТ) ОМТ. При дообследовании по данным МРТ ОМТ от октября 2020 г. (рис. 2) подозрение на клеточную миому матки (матка в обычном положении размерами 107×148×118 мм, из левого ребра матки на уровне тела исходит узловое образование 123×74×121 мм на всю толщу миометрия, доходит до эндометрия, но не пролабирует в полость). Описано образование гетерогенной структуры с немногочисленными мелкими участками кистозной дегенерации, по сигналам близкое к миометрию. Полость матки существенно деформирована, но при этом отчетливо прослеживается. В остальном миометрий обычный. Правый и левый яичники без структурной патологии. Учитывая вышеописанное, пациентку направили на госпитализацию в Центр для проведения оперативного лечения.

По данным анамнеза жизни: девочка – ребенок от первых родов, первая из двойни. Из перенесенных заболеваний отмечает острые респираторные вирусные инфекции. Перенесенные операции отрицает. Аллергические реакции отрицает. Гемотрансфузионный анамнез не отягощен. Вредные привычки отрицает. По данным гинекологического анамнеза: менархе в 13 лет, менструации установились сразу, регулярные по 7 дней через 28 дней, обильные, болезненные (по поводу чего принимает ибупрофен, со слов, «до 3 таблеток в сутки»).
При поступлении в стационар состояние пациентки удовлетворительное. Сознание ясное, контактна. Девочку беспокоят общая слабость и увеличение живота в объеме. Кожные покровы и видимые слизистые чистые, бледно-розовой окраски, физиологической влажности, тургор сохранен. Температура тела 36,6°С. Рост 157 см. Вес 49 кг. Индекс массы тела 20 кг/м2. Физическое и половое развитие соответствует возрасту. Регионарные лимфоузлы при пальпации не увеличены, безболезненные. Молочные железы мягкие, соски чистые, не втянуты, выделений из сосков нет. Дыхание ровное, везикулярное, хрипов нет. Частота дыхательных движений 15 в минуту. Сердечные тоны ясные, ритмичные. Частота сердечных сокращений 79 в минуту, пульс удовлетворительной наполненности. Артериальное давление 110/70 мм рт. ст. Язык не обложен.
Живот мягкий, округлен и увеличен в объеме за счет плотного образования матки (размер соответствует 20 неделям беременности), безболезненный при пальпации. Симптомов раздражения брюшины нет. Мочеиспускание свободное, безболезненное. Симптом поколачивания отрицательный с обеих сторон. Стул регулярный, оформленный.
При гинекологическом осмотре: наружные половые органы сформированы по женскому типу. Клитор не увеличен, наружное отверстие уретры расположено типично. Гимен бахромчатый. Ректально: матка значительно увеличена в размерах, до 20 недель беременности, безболезненна при пальпации. Придатки четко не определяются.
Пациентке выполнено УЗИ ОМТ на 10-й день менструального цикла. Обнаружено: тело матки отклонено вправо. Размеры матки: длина 7 см, толщина 5,7 см, ширина с узлом 15,7 см. По задней стенке слева определяется субсерозно-интерстициальный миоматозный узел размерами 11,5×10,5×13,0 см. В режиме цветного доплеровского картирования определяются единичные зоны васкуляризации на периферии узла. Полость матки не расширена. М-эхо 6 мм, обычной эхо-структуры. Шейка матки обычной эхоструктуры. Правый яичник 4,1×1,7×2,3 см. Фолликулярный аппарат выражен. Объем яичника 8,4 см3. Левый яичник 4,5×2,1×2,1 см. Фолликулярный аппарат выражен. Объем яичника 10,4 см3. Эхографический диагноз: миома матки гигантских размеров.
По данным УЗИ почек и мочевыводящих путей: почки расположены типично, контуры четкие. Правая почка: 104×34 мм, не увеличена. Паренхима дифференцирована, толщина паренхимы 11–16 мм. Чашечно-лоханочная система: не расширена, стенки не изменены. Левая почка: 119×49 мм, не увеличена. Паренхима дифференцирована, толщина паренхимы 11 мм, на полюсах до 20–24 мм. Лоханка расширена до 37 мм, чашечки верхней трети 18 мм, средней трети 9–14 мм, нижней трети 11–13 мм, стенки не изменены. Мочеточник расширен в верхней трети до 15 мм, в средней трети до 11 мм. Надпочечники: не изменены. Мочевой пузырь выполнен, стенка 6 мм слоистая, в просвете мелкодисперсная взвесь. Мочеточники в нижней трети не расширены. Выставлен эхографический диагноз: Уретерогидронефроз слева. Косвенные признаки цистита.
В Центре выполнен пересмотр дисков МРТ ОМТ. Установлено: матка размерами 13,1×12,6×8,1 см, полость расширена до 0,7 см с геморрагическим содержимым. По задней стенке и слева образование размерами 12,1×7,5×11,6 см, верхний контур на уровне пупка. Образование имеет неоднородную структуру с участками кистозной дегенерации. Мочевой пузырь расправлен не полностью, видимая стенка не изменена, содержимое однородно, левый мочеточник до 0,8 см в проксимальных отделах, правый без особенностей. Уретра не изменена. Заключение: МР-картина миомы матки больших размеров с выраженной деформацией полости матки и компрессией мочевого пузыря.
Исследованы основные лабораторные показатели. Данные клинического и биохимического анализов крови, коагулограммы в пределах нормативных значений. Лейкоциты – 4,21×109/л; эритроциты –4,48×1012/л; гемоглобин – 119 г/л; гематокрит – 35,6%; тромбоциты – 264×109/л.
По данным биохимического анализа крови: общий белок – 77 г/л; глюкоза – 4,9 ммоль/л; мочевина – 3,1 ммоль/л; креатинин – 66,9 мкмоль/л; билирубин общий – 5,5 мкмоль/л; билирубин прямой – 2,4 мкмрль/л; ЛДГ – 368,7 Ед/л; С-реактивный белок – 1,66 мг/л; железо – 14,4 мкмоль/л, ферритин – 30,8 мкг/л.
В коагулограмме: фибриноген по Клауссу – 2,73 г/л; протромбиновое время – 12,5 с; МНО – 1,1; АЧТВ – 33,1 с; тромбиновое время – 23,5 с.
При исследовании онкомаркеров отмечалось повышение уровня СА 125 – 48,51 (0–35) Ед/мл. Остальные онкомаркеры в пределах нормы. НЕ4 – 51,5 (0–60) пмоль/л; СА 19-9 – 10,6 (0–37) Ед/мл; РЭА – 0,69 (0–5) нг/мл; СА 72-4 – 0,94 (0–7) Ед/мл; СА 15-3 – 26,8 (0–30) Ед/мл; АФП – 0,51 (0–10) МЕ/мл; ХГЧ <0,5 (0–10) Ме/мл.
По результатам данных анамнеза, клинического, лабораторного и инструментальных исследований установлен диагноз: Миома матки больших размеров (13 см). Гидронефроз левой почки (компрессионного характера). Пациентке показано оперативное лечение в объеме: лапароскопия с возможной конверсией на лапаротомию, миомэктомия со срочным гистологическим исследованием, реинфузия аутоэритроцитов. Девочке и ее родителям разъяснены диагноз и выбранная тактика. От законного представителя получено информированное письменное согласие.
Хирургическое вмешательство проводилось под комбинированной эндотрахеальной анестезией. Первоначально осуществлялся лапароскопический доступ. Пункция брюшной полости и разрез для введения тубуса лапароскопа выполнены на 2 см выше и влево от пупка. При лапароскопии визуализировано тело матки, увеличенное до 20 недель беременности. Матка отклонена влево и резко деформирована узлом миомы матки, исходящим из передней стенки матки на широком основании, переходящим на дно матки, размерами 16×12 см. Широкая маточная связка, круглая маточная связка слева, яичник левый и маточная труба, маточные сосуды были распластаны на миоматозном узле. Яичник справа без видимой патологии, нормальных размеров, фолликулярный аппарат сохранен, маточная труба справа без видимой патологии, ампулярный отдел свободен, фимбрии выражены. Печень, желчный пузырь, аппендикс без патологии.
Однако, учитывая размеры миоматозного узла, его расположение, риск интраоперационной кровопотери, консилиумом все же было решено перейти на лапаротомию.
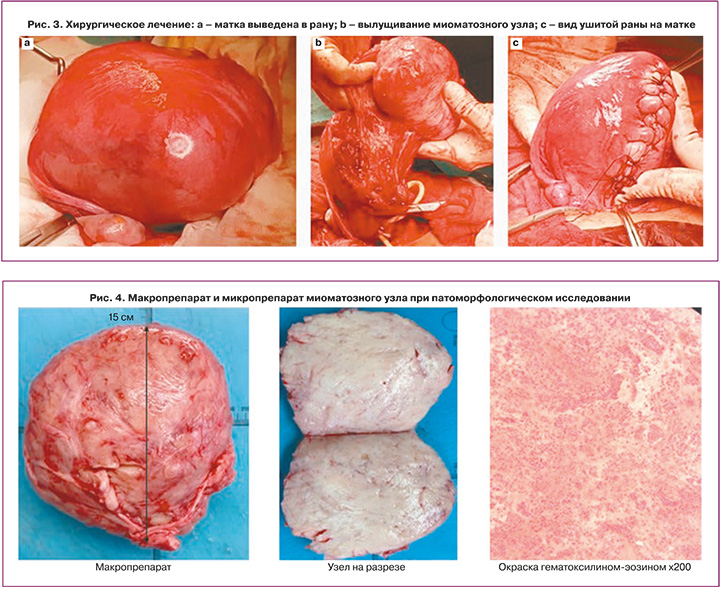
Произведена поперечная надлобковая лапаротомия, передняя брюшная стенка вскрыта послойно. Матка выведена в рану (рис. 3a). По передней стенке матки произведен продольный разрез, миоматозный узел вылущен (рис. 3b) тупым и частично острым путем без вскрытия полости матки, отправлен на срочное гистологическое исследование. Заключение: лейомиома матки. Передняя стенка матки восстановлена послойно мышечно-мышечными и мышечно-серозными отдельными викриловыми швами (рис. 3c). Произведен контроль гемостаза. Брюшная полость промыта и осушена. Передняя брюшная стенка зашита послойно наглухо. На кожу наложен косметический шов. Асептическая наклейка. Интраоперационно выполнена реинфузия аутоэритроцитов 250 мл с гематокритом 50%. Общая кровопотеря составила 200 мл. Операция продолжалась 1час 35 минут.
В послеоперационном периоде пациентка получала комплексную антибактериальную, инфузионную, противовоспалительную и обезболивающую терапию. Проведена профилактика тромбоэмболических осложнений. Послеоперационный период протекал без осложнений, заживление первичным натяжением. Пациентка выписана в удовлетворительном состоянии.
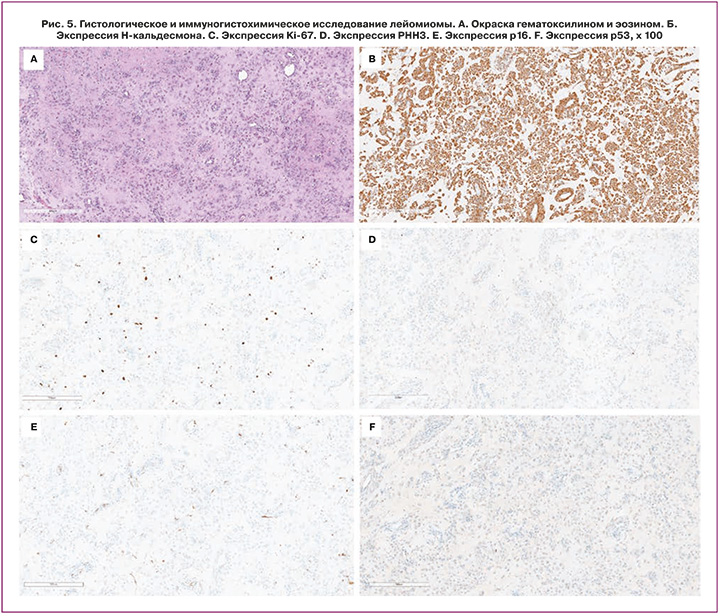
По результатам патологоанатомического исследования: присланные узлы представляли собой участки гладкомышечной ткани из разнонаправленных волокон с гиалинозом. Заключительный патоморфологический диагноз: множественная лейомиома тела матки (рис. 4). Выполнено иммуногистохимическое исследование (рис. 5). Подтверждена гистологически доброкачественная опухоль из гладких мышц матки (лейомиома) с отеком и гиалинозом. Положительная экспрессия H-кальдесмона подтверждает гладкомышечную природу опухоли. Экспрессия фосфогистона H3 (PHH3) показывает только 1–2 положительные клетки в 10 HF. Этот маркер помогает визуализировать митотические фигуры, а его низкая экспрессия свидетельствует о низкой митотической активности опухоли. Экспрессия Ki-67 демонстрирует индекс пролиферации (5–7%). Ki-67 может быть положительным для клеток в нескольких фазах клеточного цикла, поэтому он менее селективен, чем PHH3, для делящихся клеток. В продемонстрированной миоме индекс пролиферации низкий в соответствии с экспрессией PHH3 или Ki-67. Таким образом, представленный случай не является пролиферативной или митотически активной опухолью. При этом в опухоли выявлена отрицательная экспрессия р53 и низкая экспрессия р16. Анализ экспрессии данных маркеров используется для дифференциальной диагностики обычной лейомиомы от других гладкомышечных опухолей (гладкомышечная опухоль с неопределенным злокачественным потенциалом и атипичная лейомиома).
Через 2 месяца после операции девочка пришла на контрольный визит. По данным осмотра и УЗИ ОМТ патологии половых органов не обнаружено. Менструации после оперативного лечения стали регулярными, через 28 дней по 6 дней, умеренными, незначительно болезненными в первые дни.
Обсуждение
Среди женщин репродуктивного возраста ММ выявляется у 70–80%, в то же время среди девочек до 18 лет – встречаемость заболевания менее 1% [1–5]. ММ относят к гормонально-зависимым заболеваниям. В пользу чего также свидетельствует факт того, что все описанные в литературе случаи ММ у пациенток до 18 лет встречались только после менархе.
Среди взрослых пациенток ММ протекает бессимптомно до 70% случаев. Симптомные миомы, в зависимости от их размера и локализации, могут проявляться аномальными маточными кровотечениями, симптомами дисменореи и сдавления смежных органов (запоры, увеличение частоты мочеиспускания, тазовой болью), увеличением живота в объеме, сексуальной дисфункцией или бесплодием [10].
К факторам риска развития миомы матки у взрослых пациенток относят ранее менархе, отсутствие родов в анамнезе и высокий паритет, ожирение, курение, прием КОК, а также поздний репродуктивный возраст [1–4, 10].
В Центре в период с 2015 г. по 2020 г. выявлена миома матки у 9 пациенток до 18 лет (таблица). Возраст пациенток на момент установления диагноза составил от 14 до 17 лет (16,11±1,05). Во всех случаях миомы были симптомными (100%). На нерегулярные менструации жаловались 3 (33,3%), на боли внизу живота 2 (22,2%), на болезненные менструации 3 (33,3%), на кровянистые выделения 2 (22,2%), на общую слабость 2 (22,2%), на увеличение живота в объеме 1 (11,1%).

К факторам риска развития миомы матки относят ранний возраст наступления менархе. Среди наших пациенток средний возраст менархе составил 12,55±0,88 лет (от 11 до 14 лет). Раннее менархе (11 лет) отмечено у одной пациентки. Кроме того, в развитии ММ отмечают наследственную предрасположенность. Так, при активном расспросе, только одна (11,1%) девочка указала на наличие в анамнезе у ее мамы и/или бабушки ММ.
Следует отметить, что к моменту обращения к врачу по поводу вышеуказанных жалоб, у 8 девочек из 9 образование достигало больших размеров. Из анамнеза одной пациентки – до момента обращения в Центр ее наблюдали в течение двух лет по поводу ММ по месту жительства. Поводом для направления в Центр стал отмеченный рост узла и его большие размеры. Размер узла на момент первоначального установления диагноза девочка и ее родители указать не смогли.Только в 1 (11,1%) случае из 9 заболевание выявили во время профилактического осмотра в образовательном учреждении. Остальные 8 случаев диагностированы при целенаправленном обращении к врачу по поводу жалоб.
На момент обращения в Центр размер образования у девочек варьировал от 7 см до 13 см (9,89±2,31). Принимая во внимание жалобы пациенток и размер образований, всем девочкам было показано оперативное лечение.
В настоящее время не существует клинических рекомендаций по ведению и лечению пациенток с ММ до 18 лет. Учитывая молодой возраст и нереализованную репродуктивную функцию, всем пациенткам выполнено органосохраняющее лечение. Причем предпочтение отдавалось лапароскопическому (ЛС) доступу. Однако в 2 случаях из 9 (22,2%) принято решение выполнить конверсию на лапаротомический (ЛТ) доступ. Всем пациенткам выполнена миомэктомия. Интраоперационно у 1 девочки выявлен сопутствующий наружный генитальный эндометриоз (НГЭ) крестцово-маточных связок и брюшины дугласова пространства. Данной пациентке выполнены коагуляция и иссечение очагов НГЭ.
Следует отметить, что выполнение лапароскопической миомэктомии у подростков требует особо высокого профессионализма оперирующего хирурга. Вмешательство у подростков сопряжено с рядом особенностей. Так, к моменту установления диагноза часто размеры миомы достигают уже больших размеров, а размеры операционного пространства могут быть более ограничены, чем у взрослых, что приводит к росту риска интраоперационных осложнений, таких как повреждение внутренних органов и увеличенная кровопотеря [6].
При патоморфологическом исследовании узловых образований матки у всех пациенток установлен диагноз «лейомиома». Наши данные согласуются с результатами зарубежных и отечественных исследований, подтверждающих во всех опубликованных случаях гистологический диагноз лейомиомы матки у пациенток в подростковом возрасте.
При этом Diesen D.L. et al. в работе 2008 г. обсуждают особенности гистологической картины леоймиом матки у подростков в виде повышения клеточности, увеличения митотической активности и клеточной атипии [11]. Указанные морфологические черты в сочетании с быстрым ростом узлов и большими размерами самих образований создают повышенный риск их малигнизации. Авторы приводят собственный случай лечения опухоли матки диаметром 15 см у девочки 14 лет. На начальных этапах исследователи подозревали злокачественное перерождение ввиду наличия повышенной клеточности, высокой васкуляризации и очагов некроза. Однако окончательное гистологическое заключение звучало как «лейомиома».
Кроме того, Wiscot описывает случай лечения образования матки (диаметр 12 см), изначально подозрительного как саркома. При патоморфологическом исследовании удаленную опухоль описывают как лейомиому матки с кистозным перерождением [12]. Позднее Morad опубликовал клинический пример лечения симптомного образования матки диаметром 7 см у девочки 15 лет. Гистологическое исследование выявило опухоль с высокой клеточностью и сосудистыми интрузиями, вследствие чего проведена дифференциальная диагностика между саркомой и лейомиомой в пользу последнего [13]. De Rooy также привел подобный описанным выше случай. Автор отметил повышенную митотическую активность и обширный рост образования. Окончательный гистологический диагноз звучал аналогично – «доброкачественная лейомиома матки» [14].
Заключение
Несмотря на редкую частоту ММ в детском возрасте, подобные клинические наблюдения встречаются в практике врача акушера-гинеколога. Однако учитывая, что в большинстве случаев ММ протекает бессимптомно, часто к моменту установления диагноза образование достигает больших размеров. В указанных ситуациях особое значение приобретает возможность выполнения органосохраняющего лечения. В целях ранней диагностики патологии органов малого таза и выполнения своевременного органосохраняющего лечения всем девочкам-подросткам показано проведение плановых профилактических осмотров, в том числе с ультразвуковым исследованием. Необходимы разработка и внедрение в клиническую практику клинических рекомендаций по ведению пациенток с миомой матки до 18 лет.