Clinical characteristics and embryological parameters in IVF programs for women with unexplained infertility
Objective: Analysis of clinical characteristics and embryological parameters in IVF programs for women with infertility of unclear genesis versus the patients with tuboperitoneal infertility.Kirakosyan E.V., Nazarenko T.A., Bachurin A.V., Pavlovich S.V.
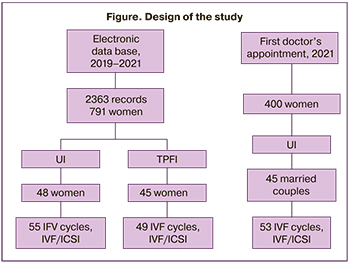
Materials and methods: The clinical characteristics of women with infertility of unclear genesis versus the patients with tuboperitoneal infertility were analyzed retrospectively and prospectively. The study group comprised 93 women, and the control group consisted of 45 patients. Embryological parameters in fertility treatment programs were compared between 108 women with infertility of unclear genesis and 49 women with tuboperitoneal infertility. The ovarian stimulation protocols were comparable between the groups of patients. Severe deviations in spermogram parameters and possible infertility factors in the partners were excluded.
Results: Significant differences were found between the groups in anamnestic, clinical, laboratory, and instrumental characteristics including women's age, mean age of their partners, women's body weight and body mass index, hereditary anamnesis, chronic diseases, previous pelvic and cervical surgery, and the infection in the pelvic organs. Statistically significant differences were found between the age at menarche, duration of menstruation and painful periods, and the data of reproductive history: the duration of unprotected sexual activity, time of establishing the diagnosis, duration of treatment before admission to IVF clinic, the use of other infertility treatment options before IVF treatment, the number of intrauterine inseminations and IVF attempts in anamnesis.
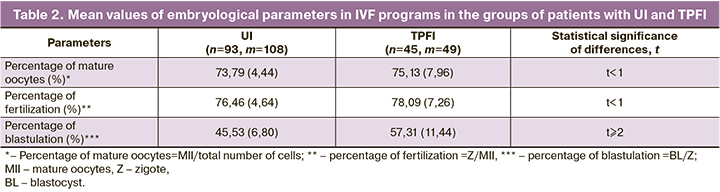
The blastulation rate was considered to be the endpoint in IVF treatmen, and it was significantly lower in the group of women with infertility of unclear genesis.
Conclusion: Clinical characteristics and embryological parameters of IVF treatment programs for women with infertility of unclear genesis were determined. A "clinical portrait" of women with infertility of unclear genesis was described and specific features of infertility were identified versus the women with tuboperitoneal infertility. The low blastulation rate was noted in IVF programs for women with infertility of unclear genesis. This may be an indirect sign of impaired embryonic development at early stages, and, therefore, can be an indication for earlier IVF treatment in order to achieve pregnancy.
Keywords
The diagnosis of unexplained infertility (UI) is established in couples whose infertility cannot be defined in the process of standard medical examination: regular, ovulatory menstrual cycle; absence of pathological changes in endometrium; normal semen parameters, patent fallopian tubes, absence of pathology by the results of laparoscopy and hysteroscopy. All these signs make it possible to categorized UI as a diagnosis of exclusion [1–3]. According to some researches, additional examination of couples with UI does not increase the incidence rate of the onset of pregnancy [4, 5]. It is recommended to take into account the age, duration of infertility, individual characteristics of patients when drawing up a plan for the diagnosis and treatment of UI [6, 7].
The introduction of the term “unclear infertility” was discussed more the 10 years ago. Its clinical validity as a stand-alone diagnosis was brought into challenge and was argued by the “dependence on the list of performed and unperformed diagnostic tests and their quality, association with endometriosis, tubal infertility, especially distal and peritubal variations, premature ovarian failure and immunological infertility.” The opposite point of view supports the idea that “despite insufficient scientific validity, the diagnosis of UI is essential from the clinical and practical point of view” [7, 8]. According to the published data, the comparison between the couples and/or women with the diagnosis of UI and women with other types of infertility or fertile women showed differences in their clinical (age, body mass index (BMI), smoking), laboratory (the level of follicle-stimulating hormone (FSH)), instrumental (number of antral follicles at the initiation of ovarian stimulation, endometrial thickness at the time of ovarian drilling), genetic (endometrial gene expression at the time of embryo implantation) characteristics [9].
Currently, there are no convincing data on the differences in live birth rates in expectant management and in the use of assisted reproductive technologies (ART) – in vitro fertilization (IVF) without or with intracytoplasmic sperm injection (ICSI) into the egg [10]; as well as no markers suggesting the advantages of the use of one or another methods of ART for the patient [11].
UI continues to remain an enigma for the doctors and researchers dictating both necessity for further research of the reproductive system of those patients, who have no obvious causes of infertility, and the improvement of clinical tactics aimed at the effective realization of reproductive function.
The purpose of the study was to analyze the clinical characteristics and embryological parameters in IVF programs for women with unexplained infertility versus the women with tubal and peritoneal factor infertility.
The study description
Research method was continuum, goal-oriented and focused on patients seeking healthcare in the Scientific and Clinical Department of ART, the National Medical Research Center for Obstetrics, Gynecology and Perinatology named after Academician V.I. Kulakov of the Ministry of Health of the Russian Federation; the period for prospective study of UI was from January 01, 2021 to December 13, 2021, retrospective study of UI from – January 1, 2019 to August 11, 2021, tubal and peritoneal factor infertility (TPFI) from January 1, 2019 to October 22, 2021).
The type of the study was observational, analytical, cohort, mixed (retrospective-prospective).
At the preparatory stage of the study the issues of diagnostics, treatment of patients with UI were defined and publications on the relevant problem were reviewed [12]. The aim and the goal of research were formulated and the working hypothesis was developed – the assumption that the patients with UI have certain clinical characteristics and embryological parameters in IVF treatment programs.
The stage I was scheduling the program and statistical analysis plan.
The program included:
1) determination of the observation unit (see Materials and methods. Inclusion criteria) and scheduling the program of material collection (sequential reporting of considered characteristics-questions, and necessity to get answers to the questionnaire);
2) scheduling the program of material development (drawing up the layouts of statistical tables based on the considered characteristics-questions and the answers received to questions: registry of UI, registry of TPFI (the control group), embryology of UI, embryology of TPFI (the control group);
3) scheduling the program for the analysis of the collected material (the list of statistical methods, which were necessary to identify the patterns of the phenomenon under the study (see Materials and methods. Statistical data processing).
Research plan:
1) the subject of research: 93 women in unexplained infertility in IVF programs;
2) statistical sample size: 45 women prospectively, 48 women with UI retrospectively and 45 women with TPFI. The samples are qualitatively and quantitatively represent the general populations, respectively, and are comparable by the number of participants.
3) The type of the study: observational, analytical, cohort, mixed (retrospective-prospective); material collection method and the terms of the study: goal-oriented (according to criteria established for this study), continuous (taking into account all cases), current (registration of detected cases); focused on patients seeking healthcare in Scientific and Clinical Department of ART, the National Medical Research Center for Obstetrics, Gynecology and Perinatology named after Academician V.I. Kulakov of the Ministry of Health of the Russian Federation; the period under study: UI prospectively from January 01,2021 to December 13, 2021, UI retrospectively from – January 1, 2019 to August 11, 2021, and TPFI from January 1, 2019 to October 22, 2021).
4) description of researchers, equipment and resources.
At stage II, material was collected according to the scheduled program and research plan. At stage III, the obtained data were processed (verification of complete collection of research material, grouping, encryption, summary of data for statistical tables, calculation of statistical parameters and statistical material processing).
At stage IV, the obtained results were analyzed, the conclusions and suggestions were made.
Materials and methods
The information about women with UI, including somatic and reproductive anamnesis of their partners, the parameters and previous IVF attempts and outcomes, embryological parameters in IVF programs was collected and analyzed retrospectively and prospectively. The group under study included 93 women with UI, the control group comprised of 45 patients with TPFI. Comparative analysis of clinical characteristic and major parameters in IVF programs was performed in 108 programs for women with UI and 49 programs in patients with TPFI, who underwent fertility treatment in IVF Departments of the National Medical Research Center for Obstetrics, Gynecology and Perinatology named after Academician V.I. Kulakov of the Ministry of Health of the Russian Federation in the period from 2019 по 2021. The ovarian stimulation protocols were comparable between the groups of patients. Severe deviations in spermogram parameters and possible infertility factors in the partners were excluded (Fig).
TPFI was diagnosed by hysterosalpingography and/or laparoscopy.
UI as diagnosis of exclusion was established in:
1) occurrence of ovulation confirmed by regular menstrual cycle length of 23–35 days, ovulation test, measurement of progesterone level in the blood during luteal phase of the menstrual cycle; visualization of the corpus luteum by ultrasound monitoring and/or laparoscopy in the luteal phase of the menstrual cycle;
2) normal uterine cavity according to ultrasound (US) examination and/or hysteroscopy and tubal patency assessment by hysterosalpingography and/or laparoscopy;
3) compliance of spermogram results with reference values of the World Health Organization (WHO) [13].
Exclusion criteria for UI:
- age of women under 35 years at the time of diagnosed infertility;
- duration of infertility not less than 3 years;
- no obvious reasons for infertility отсутствие очевидных причин бесплодия;
- normal female karyotype (46ХХ) and male karyotype (46ХУ).
Patient evaluation included:
- anamnestic data collection (questionnaire);
- examination of patients according to the requirements for undergoing IVF programs (Order No. 803 n of July 31, 2020).
The patients underwent treatment in F. Paulsen Scientific and Clinical Department of ART, the National Medical Research Center for Obstetrics, Gynecology and Perinatology named after Academician V.I. Kulakov of the Ministry of Health of the Russian Federation based on standard protocols routinely used in the Departments of IVF, which are in compliance with the international and European criteria of quality. The ovarian stimulation short protocol with gonadotropin-releasing hormone (GnRH) antagonist, and less commonly long protocol with GnRH agonists were used. The starting daily dose of gonadotropins was selected individually depending on the BMI, patient’s age, the level of anti-Müllerian hormone (AMH) and antral follicle count (AFC) and averaged 225 IU. All manipulations, cultivation conditions, and work of medical personnel was performed in the same manner as it has been done for more than 5 years of functioning of the Department and the standards. IVF/ICSI was performed according to indications: failed or low frequency (<20%) of fertilization in the previous IVF attempt, obBlastocyst cultivation was carried out using IVF Cleavage Medium (COOK), embryos were transferred 5 days after obtaining oocytes. According to the clinical recommendations of the Russian Federation, no more than 2 embryos were transferred into the uterus.
Statistical analysis
Clinical and embryological data base were created using Microsoft Excel software program and were used for storage and preliminary data processing. Statistical data processing was carried out using absolute relative and mean values, criteria of diversity of the variations, the method of standardization method, parametric methods for assessment of reliability of the results: estimation of the representativeness error, assessment of statistical significance of the difference in the results (t criterion, probability of error-free prediction P), determination of confidence limits for mean and relative values.
The blastulation rate was considered to be the endpoint in IVF treatment programs.
Results
At stage I of the study, the anamnestic, clinical, laboratory and instrumental parameters in patients with UI and TPFI were evaluated.
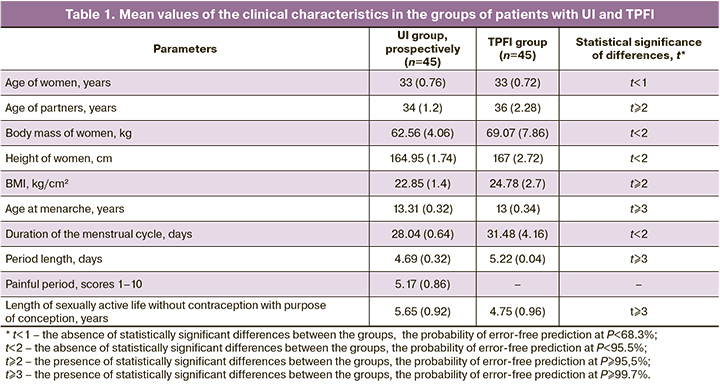
Despite the absence of difference in the mean age of women, the individual analysis showed that the proportion of women aged ≤ 35 in the group with unexplained infertility was 87% and was statistically lower versus the group with tubal and peritoneal factors of infertility – 96%. In the group of women with TPFI, the partners’ mean age was statistically significantly higher than in group with UI (Table 1). Statistically the number of women with body mass 60–70 kg was significantly high in UI group versus TPFI group; the mean BMI and number of women with excessive body mass (BMI>25 kg/cm2) was significantly high in TPFI group versus UI group.
In UI group, the number of women with cancer burden was statistically higher – 47% or with diabetes mellitus – 44% in hereditary anamnesis versus TPFI group (24% and 14%, respectively).
Evaluation of somatic health of women in the study groups showed that significantly more often thyroid disorders were in UI group – in 31% of women and diseases of digestive system were in 29% of women. In TPFI group significantly more often were gynecological diseases – in 66% of patients (endometriosis, adnomiosis was in 13%, mastopathy in 11%, fibroids in 9%, chronic endometritis in 9%, chronic salpingo-oophoritis in 7%, polycystic ovary syndrome (PCOS) in 4%, other diseases in 13% of patients), including pelvic inflammatory disease in 38% of women, which were unspecific for UI group (11% and 13%, respectively).
Statistically, the number of women, who underwent laparoscopy – 94%, hysteroscopy – 88%, endometrial biopsy 83%, the results of which showed concomitant changes – 50%, other interventions – 82%, including laparotomy – 64%, restoration of tubal patency – 33%, surgery on the cervix in anamnesis – 67%, was significantly higher in TPFI group (47%, 58%, 56%, 27%, 24%, 2%, 7% and 24%, respectively, and this was specific for pathogenesis of TPFI.
According to the anamnestic data, the presence of ectopic pregnancies, pelvic inflammatory disease, gynecological diseases, interventions for the diagnosis and treatment of pelvic organs and the abdominal cavity were in 94% of patients with TPFI, and only in 58% of women with UI, who underwent mainly diagnostic interventions.
Statistically, the mean age at menarche was significantly higher in UI group than in TBFI group. At the same time, the number of women, whose age for menarche was less than 12 years, in TBFI group was significantly higher versus in UI group (Table 1). The average period length in TPFI group was significantly longer versus UI group (Table 1). In UI group, the number of women, who had painful periods, was significantly higher – 64% versus 29% in TBFI group. The average period pain according to the score points from 1 to 10 was 5.17, the average range was 4.31–6.03 points, and this corresponded to the upper limit of moderate pain (up to 5 points) and to the lower limit of severe pain (above 6 points) 6) (Table 1). It is probable that due to this fact the number who took pain medications to treat period pain was significantly higher than in UI group. Currently, pathogenetic association between primary dysmenorrhea and unexplained infertility is not established [14].
The differences between UI group and TPFI group with regard to pregnancies that ended with births in anamnesis in 11% and 21% of women, respectively; and with regard to pregnancies with adverse outcomes in anamnesis in 44% and 54% of women, respectively.
Statistically, the average length of sexually active life without contraception with purpose of conception was significantly longer in UI group – 5.65 years versus 4.75 years in TBFI group. At the same time, the number of women who had sexually active life without contraception with purpose of conception lasting for more than 6 years was significantly higher in UI group – 43% versus 29% in TPFI group. In UI group the number of women who used contraception before pregnancy was 76% versus 19% in TPFI group. Presumably, this was associated with patients’ awareness about low probability of spontaneous pregnancy in cases of TPFI.
Statistically, the number of women with previously established diagnosis of infertility factor was significantly higher in TPFI group – 100% versus 69% in UI group. The number of women in TPFI group, who underwent ART in anamnesis with the purpose to conceive, was significantly higher – 89% versus 67% in UI group. In UI group, 27% of patients had intrauterine insemination in anamnesis: in 25% of women it failed, 2% of women had miscarriage. Moreover, the average time period before seeking healthcare in the IVF clinic in this subgroup was 6.33 years. The number of women with failed IVF attempts in medical history was significantly high in TPFI group – 54% versus 38% in UI group. Statistically significant differences between the groups in the outcomes of IVF programs in anamnesis were not found: birth rates were 4.4% and 5,4%, miscarriage – 2.2% and 5.4%, missed miscarriage – 7% and 5.4%, biochemical pregnancy – 4.4% and 8%, respectively. The number of women with one IVF attempt in anamnesis was significantly high in TPFI group – 39%, and in UI group with two UVF attempts in anamnesis – 36 %. The differences between the groups with 3 or more IVF attempts in anamnesis were not found.
The obtained data can be explained by the fact, that patients with UI do not undergo medical screening over the course of many years, due to this the cause of infertility remains unexplained, and the attempts to conceive or “recover” fail. This is the reason why the patients seek IVF too late. In patients with TPFI, the cause of infertility is obvious, and IVF is the only possible way to achieve pregnancy for them, so the patients timely seek appropriate medical care.
Indicators of ovarian reserve status – the level of AMH not less than 1.2 ng/mL and antral follicular count (AFC) not less than 5 assessed by US imaging in patients in the follicular phase, corresponded with the values regulating the IVF program according to the clinical recommendations. Statistically significant differences between the mean values of AMH in the groups (2.44 ng/mL in UI group and 2.34 ng/mL in TPFI group). According to US assessment in the follicular phase, the number of women with multifollicular ovaries was significantly high (37%) in TPFI group, and a high number of women with 8–12 antral follicles (31%) was in UI group.
Thus, a “clinical portrait” of the patient with UI was described: a woman aged 33 years (the partner’s age 34 years), with body mass 62.56 kg, height 164.95 cm, normal BMI 22.85 kg/cm2, age at menarche 13.31 years, duration of the menstrual cycle 28.04 days, period length 4.69 days, moderate period pain score of 5.17 points, length of sexually active life without contraception with purpose of conception 5.65 years, cancer or diabetes mellitus in hereditary anamnesis in the half of cases, with thyroid disorders or diseases of digestive system were the one third of cases, absence of infectious or non-infectious gynecological diseases, no pelvic and cervix surgery, births in anamnesis in one tenth of cases, adverse pregnancy outcomes in anamnesis in half of cases, previously diagnosed infertility and two IVF attempts in two thirds of cases, birth rate as a result of IVF 4.4–7.4%, normal ovarian reserve according AMH test – 2.44 ng/mL and AFC – 8–12 in the follicular phase.
At the second stage of the study, embryological parameters in IVF programs in patients with UI and TPFI were assessed. According to the obtained mean values, sufficient number of mature oocytes, normal fertilization rate and low blastulation rate in IVF programs were observe in UI group (Table 2). This suggests a lack of blastulation in cases of UI, i.e., abnormally low ratio of the number of blastocysts to the number of fertilizations (zygotes).
Discussion
The results of the study confirmed the data in a number of publications about delayed healthcare seeking in the IFV clinics by patients diagnosed with UI, and as a consequence their age was higher [3, 15, 16]. According to the mathematical model, 2 years after regular sexually active life the frequency of false-positive diagnosis of UI increases from 10% in women under 35 years of age to 50% in women over 37 years of age and reaches more than 80% in women over 40 years of age [3, 17]. In our study the age of patients in both groups was limited to 35 years. Nevertheless, the number of women under 35 years of age in TPFI group was higher than in in UI group (96% and 87%, respectively). It is natural that the patients with UI underwent medical examination for a long period of time and other methods were used for their treatment. The issue of expectant management and other methods of treatment, primarily intrauterine insemination in cases of UI is disputable [9]. Intrauterine insemination was performed in 27% of patients with UI and had low efficiency: 2% of achieved pregnancies were non-developing pregnancies.
Anamnestic and phenotypic characteristics specific for the patients with UI were identified. The conditions that may be categorized as autoimmune diseases: thyroid disorders (autoimmune thyroiditis) and gastrointestinal disorders (chronic gastritis, chronic gastroduodenitis, biliary dyskinesia) were most common in cases of UI – 31% and 29%, respectively; while the rate of gynecological diseases (endometriosis, adenomiosis, mastopathy, fibroids, chronic endometritis, chronic salpingo-oophoritis, PCOS and other conditions), pelvic inflammatory disease was significantly high in cases of TPFI – 66% and 38%, respectively, and the rate of surgical interventions (laparoscopy, hysteroscopy, restoration of tubal patency, surgery on the cervix and other surgical procedures) was 94%. Most commonly these surgical interventions were performed repeatedly, including laparotomy, and were the cause of TPFI. In UI group, uterine fibroids and endometriosis lesions were less common versus TPFI group (2 and 9%, respectively) and (9% and 13%, respectively), which theoretically can be the cause of infertility. Moreover, excessive body weight and other phenotypic and clinical features, such as polycystic ovaries, hirsutism, insulin resistance, were not specific for women with UI.
A number of studies presented the data that patients with UI can have low ovarian reserve, which is defined by abnormal levels of AMH and AFC in the follicular phase [12, 16, 18]. This study did not confirm this suggestion. According to the obtained data, ovarian reserve in women with UI was comparable with ovarian reserve in cases of TPFI and was normal for the patients of lower age. The only difference was that AFC tended to decrease. This can be explained by the fact that there were no women with polycystic ovaries among the patients with UI versus the patients with TPFI.
Therefore, the clinical and anamnestic characteristics and parameters of the reproductive system were quite normal in patients with UI, for this reason, at this stage of the study, there was no answer to the question, why pregnancy did not occur
In this respect, the embryological stage of IVF programs was investigated. The obtained data indicated that in cases of UI, the number of mature oocytes was sufficient, the fertilization rate was normal. However, the blastulation rate was low, and could be an indirect sign of impaired early embryogenesis and, therefore, an indication for early use of IVF with purpose of achieving pregnancy. Limited information is presented in literature about embryological parameters in patients with UI. The existing data suggesting that the rate of fertilization failures after IVF in patients with UI reaches 43% and exceeds the rate of fertilization failures after IVF/ICSI is controversial and were not confirmed by our study [19]. In this study, fertilization was achieved in UI group in 67% of cases using ICSI, and this largely reflects generally accepted clinical practice. However the comparison between IVF and IVF/ICSI showed that the rates of fertilization were similar.
The results of our study showed that statistically significant difference of the embryological stage of IVF programs was a low blastulation rate in patients with UI versus patients with TPFI (45.53% and 57.31%, respectively) due to a low quality of oocytes and/or genetic or epigenetic factors that have an impact on the process of early embryogenesis [19, 20]. Investigation of possible causes and factors of impaired early embryogenesis is a relevant objective of modern science [21–23].
Conclusion
This study identified the clinical characteristics and embryological parameters in IVF programs for women with unexplained infertility. A "clinical portrait" of women with unexplained infertility was described and specific features of infertility were identified versus the women with tubal and peritoneal factors of infertility. Low blastulation rate was considered to be the endpoint in IVF treatment programs, and in was significantly low in the group of women with unexplained infertility.
The obtained data demonstrating impaired parameters of early embryogenesis in idiopatic infertility suggest to use the strategy of early IVF in this category of patients.
References
- Practice Committee of the American Society for Reproductive Medicine. Electronic address: asrm@asrm.org; Practice Committee of the American Society for Reproductive Medicine. Evidence-based treatments for couples with unexplained infertility: a guideline. Fertil. Steril. 2020; 113(2): 305-22. https://dx.doi.org/10.1016/j.fertnstert.2019.10.014.
- ACOG Committee. Infertility workup for the women’s health specialist: ACOG Committee Opinion, Number 781. Obstet. Gynecol. 2019; 133(6): e377-84. https://dx.doi.org/10.1097/AOG.0000000000003271.
- Buckett W., Sierra S. The management of unexplained infertility: an evidence-based guideline from the Canadian Fertility and Andrology Society. Reprod. Biomed. Online. 2019; 39(4): 633-40. https://dx.doi.org/10.1016/j.rbmo.2019.05.023.
- National Institute for Health Care Excellence Fertility Problems: Assessment and Treatment NICE Clinical Guidelines [CG156]. United Kingdom: NICE; 2017.
- Назаренко Т.А. Вспомогательная репродукция в клинической практике. Разбор клинических случаев с использованием международных и отечественных рекомендаций. М.: МедКом-Про; 2020. 121с. [Nazarenko T.A. Assisted reproduction in clinical practice. Analysis of clinical cases using international and domestic recommendations. M.: MedKom-Pro; 2020. 121 p. (in Russian)].
- Gunn D.D., Bates G.W. Evidence-based approach to unexplained infertility: a systematic review. Fertil. Steril. 2016; 105(6): 1566-74.e1. https://dx.doi.org/10.1016/j.fertnstert.2016.02.001.
- Nandi A., Gudi A., Shah A., Homburg R. An online survey of specialists' opinion on first line management options for unexplained subfertility. Hum. Fertil. (Camb.). 2015; 18(1): 48-53. https://dx.doi.org/10.3109/14647273.2014.948081.
- Gleicher N., Barad D. Unexplained infertility: does it really exist? Hum. Reprod. 2006; 21(8): 1951-5. https://dx.doi.org/10.1093/humrep/del135.
- Abrahami N., Izhaki I., Younis J.S. Do young women with unexplained infertility show manifestations of decreased ovarian reserve? J. Assist. Reprod. Genet. 2019; 36(6): 1143-52. https://dx.doi.org/10.1007/s10815-019-01467-0.
- Wang R., Danhof N.A., Tjon-Kon-Fat R.I., Eijkemans M.J., Bossuyt P.M., Mochtar M.H. et al. Interventions for unexplained infertility: a systematic review and network meta-analysis. Cochrane Database Syst. Rev. 2019; 9(9): CD012692. https://dx.doi.org/10.1002/14651858.CD012692.pub2.
- Tjon-Kon-Fat R.I., Tajik P., Zafarmand M.H., Bensdorp A.J., Bossuyt P.M.M., Oosterhuis G.J.E. et al. IVF or IUI as first-line treatment in unexplained subfertility: the conundrum of treatment selection markers. Hum. Reprod. 2017; 32(5): 1028-32. https://dx.doi.org/10.1093/humrep/dex037.
- Киракосян Е.В., Назаренко Т.А., Павлович С.В. Поиск причин формирования нарушений репродуктивной системы: обзор научных исследований. Акушерство и гинекология. 2021; 11: 18-25. [Kirakosyan E.V., Nazarenko T.A., Pavlovich S.V. Search for the causes of reproductive system disorders: a research review. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2021; 11: 18-25. (in Russian)]. https://dx.doi.org/10.18565/aig.2021.11.18-25.
- World Health Organization. WHO laboratory manual for the examination and processing of human semen, 5th ed. WHO; 2010.
- Madendag I.C., Sahin M.E., Madendag Y., Sahin E., Demir M.B., Ozdemir F. et al. Effect of the anterior uterocervical angle in unexplained infertility: a prospective cohort study. J Int. Med. Res. 2020; 48(4): 300060519893497. https://dx.doi.org/10.1177/0300060519893497.
- Siristatidis C., Pouliakis A., Sergentanis T.N. Special characteristics, reproductive, and clinical profile of women with unexplained infertility versus other causes of infertility: a comparative study. J. Assist. Reprod. Genet. 2020; 37(8): 1923-30. https://dx.doi.org/10.1007/s10815-020-01845-z.
- Yücel B., Kelekci S., Demirel E. Decline in ovarian reserve may be an undiagnosed reason for unexplained infertility: a cohort study. Arch. Med. Sci. 2018; 14(3): 527-31. https://dx.doi.org/10.5114/aoms.2016.58843.
- Vogiatzi P., Pouliakis A., Siristatidis C. An artificial neural network for the prediction of assisted reproduction outcome. J. Assist. Reprod. Genet. 2019; 36(7): 1441-8. https://dx.doi.org/10.1007/s10815-019-01498-7.
- Bosch E., Alviggi C., Lispi M., Conforti A., Hanyaloglu A.C., Chuderland D. et al. Reduced FSH and LH action: implications for medically assisted reproduction. Hum. Reprod. 2021; 36(6): 1469-80. https://dx.doi.org/10.1093/humrep/deab065.
- Bosselut H., Paulmyer-Lacroix O., Gnisci A., Bretelle F., Perrin J., Courbiere B. Facteurs pronostiques des chances de naissance vivante enfécondation in vitro pour infertilité inexpliquée: étude de cohorte. Gynécol. Obstét. Fertil. Sénol. 2021; 49 (7-8): 601-7. https://dx.doi.org/10.1016/j.gofs.2021.01.002.
- Larbuisson A., Raick D., Demelenne S., Delvigne A. ICSI diagnostic: a way to prevent total fertilization failure after 4 unsuccessful IUI. Basic Clin. Androl. 2017; 27: 18. https://dx.doi.org/10.1186/s12610-017-0061-z.
- Киракосян Е.В., Екимов А.Н., Павлович С.В. Значение ооцитарного фактора в развитии бесплодия неясного генеза. Акушерство и гинекология. 2022; 1: 14-21. [Kirakosyan E.V., Ekimov A.N., Pavlovich S.V. The significance of the oocyte factor in the development of infertility of unclear genesis. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2022; 1: 14-21. (in Russian)]. https://dx.doi.org/10.18565/aig.2022.1.14-21.
- Mansour R., El-Faissal Y., Kamel A., Kamal O., Aboulserour G., Aboulghar M. et al. Increased insulin resistance in men with unexplained infertility. Reprod. Biomed. Online. 2017; 35(5): 571-5. https://dx.doi.org/10.1016/j.rbmo.2017.08.020.
- Sfakianoudis K., Maziotis E., Karantzali E., Kokkini G., Grigoriadis S., Pantou A. et al. Molecular drivers of developmental arrest in the human preimplantation embryo: a systematic review and critical analysis leading to mapping future research. Int. J. Mol. Sci. 2021; 22(15): 8353. https://dx.doi.org/10.3390/ijms22158353.
Received 05.04.2022
Accepted 06.05.2022
About the Authors
Evgeniya V. Kirakosyan, Ph.D. student, Department of Obstetrics, Gynecology, Perinatology and Reproductology, I.M. Sechenov First Moscow State Medical University, Ministry of Health of the Russian Federation (Sechenov University), Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of the Russian Federation, +7(916)574-79-63, evgeniya.kirakosyan@mail.ru, https://orcid.org/0000-0002-6021-2449, 4 Akademika Oparina str., Moscow 117997, Russia.Tatyana A. Nazarenko, Dr. Med. Sci., Professor, Director of the Institute of Reproductive Medicine, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of the Russian Federation, +7(495)531-44-44, t_nazarenko@oparina4.ru, https://orcid.org/0000-0002-5823-1667, 4 Akademika Oparina str., Moscow 117997, Russia.
Alexey V. Bachurin, Ph.D., Head of the Laboratory of Clinical Embryology, Scientific and Clinical Department of ART named after F. Paulsen, Academician V.I. Kulakov
National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of the Russian Federation, a_bachurin@oparina4.ru,
https://orcid.org/0000-0002-3768-7657, 4 Akademika Oparina str., Moscow 117997, Russia.
Stanislav V. Pavlovich, Ph.D., Academic Secretary, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of the Russian Federation; Professor, Department of Obstetrics, Gynecology, Perinatology and Reproductology, I.M. Sechenov First Moscow State Medical University,
Ministry of Health of the Russian Federation (Sechenov University), +7(495)438-20-88, s_pavlovich@oparina4.ru, https://orcid.org/0000-0002-1313-7079,
4 Akademika Oparina str., Moscow 117997, Russia.
Corresponding author: Evgeniya V. Kirakosyan, evgeniya.kirakosyan@mail.ru
Author’s contributions: Kirakosyan E.V., Nazarenko T.A., Pavlovich S.V. – the concept and design of the study; Kirakosyan E.V., Nazarenko T.A., Bachurin A.V. – material collection and processing; Kirakosyan E.V. – statistical data processing, article writing; Kirakosyan E.V., Nazarenko T.A., Bachurin A.V., Pavlovich S.V. – published data analysis, article editing.
Conflicts of interest: The authors declare that they have no conflict of interests regarding this publication.
Funding: No financial support has been provided for this work.
Ethical Approval: The study was approved by the Academic Council (extract from the Order No. 4070/OP-32 of September 30, 2020) and the local Ethics Committee (extract from Protocol No.33-20 of November 25, 2020) of I.M. Sechenov First Moscow State Medical University of the Ministry of Health of the Russian Federation; and by the Ethics Committee for biomedical researches (extract from Protocol No. 11 of November 12, 2020) of the Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of the Russian Federation.
Patient Consent for Publication: All patients provided informed consent for the publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available on request from the corresponding author after approval from the principal investigator.
For citation: Kirakosyan E.V., Nazarenko T.A.,
Bachurin A.V., Pavlovich S.V. Clinical characteristics and
embryological parameters in IVF programs for women with unexplained infertility.
Akusherstvo i Gynecologia/Obstetrics and Gynecology. 2022; 5: 83-90 (in Russian)
https://dx.doi.org/10.18565/aig.2022.5.83-90