Chronic endometritis and an incompetent uterine scar after cesarean section: long-term outcomes of metroplasty
Objective. To determine the impact of chronic endometritis (CE) on the formation of an incompetent uterine scar (IUS) and the results of laparoscopic metroplasty.Glukhov E.Yu., Dikke G.B., Neff E.I., Glukhova V.E., Svyazhina A.V.
Subjects and methods. The investigation included 50 patients with IUS in the periods longer than 1 year after cesarean section. Laparoscopic metroplasty was performed in conjunction with preparatory and rehabilitation activities. The outcomes were compared between two groups: 1) 26 patients with CE and 2) 24 patients without CE.
Results. The rate of CE in patients with IUS was 52%. The overall efficiency of laparoscopic metroplasty was 92%. The outcomes were the same in patients with and without CE: the onset of pregnancy was 60 and 81%, respectively (p = 0.22), birth was in 60 and 64.7% (p = 0.21), the progression of pregnancy was in 20 and 12.5% (p = 0.35).
Conclusion. The high rate (52%) of CE suggests that the latter has a possible role in the pathogenesis of IUS. Laparoscopic metroplasty in combination with preparation and rehabilitation is effective in 92%.
Keywords
The uterine suture healing after cesarean section (CS) is the critical factor in the formation of the proper scar and satisfactory subsequent pregnancy course and its outcome [1].
In the complex of activities aimed at preparing for the future pregnancy, the assessment of the condition of the uterine scar in the interval period plays an important role. The effective surgical method for correction of the incompetent uterine scar (IUS) is laparoscopic metroplasty (2–5 years after delivery). Laparoscopic metroplasty in the interval period is performed due to the threat of the uterine rupture along the scar during pregnancy and delivery, the high risk of hysterectomy during childbirth when the placenta is ingrown into the scar and the formation of “uterine hernia”, the incompetent scar with clinical manifestations (dysmenorrhea, postmenstrual bleeding) [2].
Laparoscopic metroplasty of the lower uterine segment with the IUS after CS performed in the interval period was described by Tower A.M. and Frishman G.N. (2013), Popov A.A. and Buyanova S.N. (2010) [3, 4]. However, these studies do not provide information about the long-term outcomes.
The objective of the research is to determine the impact of chronic endometritis (CE) on the formation of the incompetent uterine scar and the results of laparoscopic metroplasty.
Materials and Methods
Design: simple prospective observational incomparable clinical research.
Material: During the period from 2009 to 2018 we performed 96 laparoscopic metroplasties of the lower uterine segment for the IUS after CS. The study included 50 patients with IUS who presented to the Center of Operative Gynecology “Women’s Clinic”, Yekaterinburg, and who were operated by one surgeon using one technique in one medical institution; the patients had more than one year after CS and they met the inclusion/exclusion requirements. They were divided into two groups. Group I included 26 patients with CE (N71.1 - chronic inflammatory uterine disease), group II included 24 patients without CE. The diagnosis of CE was made before the surgery or retrospectively after the performance of diagnostic hysteroscopy prior to the surgical intervention (metroplasty); subsequently the diagnosis was confirmed on the basis of morphological study of the uterine cavity aspirate.
Criteria for inclusion in the study were patients’ age of 25–45 years, incompetent uterine scar after cesarean section (ICD-10 code - O34.2), period of time from the CS before inclusion in the study ≥ 12 months, ovulatory menstrual cycle, isocoagulation of blood, voluntary informed consent.
Exclusion criteria were acute contagious diseases, genital malformations, sexually transmitted diseases without prior sanitation, malignant neoplasms of any localization, severe somatic pathology, tuberculosis of any localization, diseases of the endocrine system, incomplete data in the long-term post-operative period.
Diagnostic methods. Ultrasound investigation of the uterus was performed on the 7–9th day of the menstrual cycle with the frontal and lateral projections (Voluson E8, curvilinear transducer 2–5 MHz, vaginal (intracavitary) sensor 4–9 MHz, including 3D Statiсa mode). The scar vascularization was determined by the Doppler velocimetry method. Hysteroscopy was used to determine the signs of the scar incompetency, adenomyosis and endometriosis of the scar and other localizations, to assess the condition of the endometrium, availability of uterine synechiae. The morphological study of endometrial aspirates obtained during hysteroscopy was performed. We also studied myometrial scar tissues excised during the surgery, stained with hematoxylin and eosin, van Gieson’s picro-fuchsin using light microscope ECL1PS 50.
In some patients, prior to the surgery, the culture was taken from the uterine cavity according to the indications (history of previous CE, habitual miscarriage, missed miscarriage, prolonged leukorrhea).
The catamnesis was studied using the telephone survey according to a specially designed questionnaire.
Methods of treatment. When the growth of opportunistic pathogenic microflora in significant titer was revealed prior to the surgical intervention, the antimicrobial therapy (according to the antibiotic susceptibility) was performed in combination with the procedures of irrigating the uterine cavity with the solutions cavitated by the low-frequency ultrasound with FOTEK AK101. We used 0.05% solution of water chlorhexidine, ultrasonic oscillation frequency 25 kHz, consumption of medicinal solution 100–150 ml/minute, infusion volume 200–300 ml. The treatment course consisted of five procedures, each lasting 3-4 minutes [5]. The operative intervention was performed after the control bacteriological study.
Metroplasty was performed on the 4-7th day of menstrual cycle under the endotracheal anesthesia using three-port access laparoscopy for the instruments (K. Storz) inserted in the typical points. Preliminary (under the conditions of single anesthethic support) all patients underwent diagnostic hysteroscopy, endometrial vacuum aspiration. After examination of the pelvic organs and abdominal cavity, adhesiolysis (in case of post-operative adhesions) and surgical treatment of the accompanying gynecologic disorders (myoma, endometriosis, ovarian cysts, etc.) were performed. Then the surgeons proceeded with the main intervention (metroplasty) that was performed according to standard technique supplemented with the argon plasma coagulation. The visible scar tissue was excised with the scissors from the upper and lower edges of the uterine wall defect. The defect edges were treated with the argon plasma flame (FOTEK EA-142, Spray mode, power 60 W) [6]. The 1-2-row separate sutures (vicryl 2.0) were put on the uterine wound. The sutures were tightened extracorporeally. The argon plasma coagulation of suture was repeated. The suture peritonization was not performed. In case of uterine retrodeviation, for the purpose of its temporary reposition (to reduce the load on the suture and prevent the suture cutting out) the plication of round ligaments to the front uterine surface was performed using the separate suture (vicryl 1.0).
Indications for laparoscopic metroplasty were as follows: the desire of the patient to have subsequent pregnancies, defect length of more than 7–8 mm (more than 1/3 of the width of the uterine lower segment in the scar area), the defect width of more than 4 mm, development of isthmocele, uterine wall thickness in the niche apex of less than 2.5 mm, presence of liquid mass in the scar, presence of the defect marginal dimensions in combination with the clinical implications (dysmenorrhea, pain, infertility, postmenstrual spotting) or ultrasound signs of scar endometriosis.
The indications for the surgery were as follows: complex sanitation of CE prior to the surgery (in case of pre-operational identification), scar localization at the level of the internal os or higher, absence of contraindications.
The patients received intravenous injections of Amoxiclav 1.2 g by drop infusion intraoperatively (92% of the total number of the treated people) or ceftriaxone 2.0 g by drop infusion (8% of patients). In case of pronounced signs of CE according to hysteroscopy findings, antibiotics were injected for up to 5 days.
During the postoperative period from the first day after surgery the following treatment was performed: magnetic therapy on the lower abdomen using Polyus 2D device, peak value is 40 mT, frequency is 12.5 Hz, pulsating field type, duration is 20 minutes, 5 sessions; intravenous laser blood irradiation (ILBI), wavelength is 0.63 µm long, duration is 15–20 minutes, 5 sessions per course.
The study was conducted in accordance with the requirements of the international and Russian legislative documents on the legal and ethical principles of medical and biological studies in humans. The study was approved by the ethics committee of the Ural State Medical University of the Ministry of Healthcare of Russia (protocol No. 28 dated April 03, 2015), all patients provided their informed voluntary consent.
Statistical processing of results was carried out using software package Statistica 6.0 and Microsoft Excel 2000. The normality of data distribution of continuous type was determined by the Kolmogorov-Smirnov test. The quantitative data are presented as the mean and standard deviations (M(SD)). Statistical significance of differences between the two average indicators was assessed using the unpaired Student’s t-test (the differences were considered statistically significant when p≤0.05). The qualitative indicators are presented in the form of absolute value in the sampled information and its fraction (n/%). When assessing the reliability of differences in the qualitative indicators, the levels of difference significance were used calculated with the Fischer’s exact test in the module “Tables 2×2” of Statistica 6. When p is less than 0.05, the differences were considered significant. When comparing the small volume groups, the Yates adjustment was applied to the Pearson χ2 criterion, if the absolute frequencies in the table cells were less than 10.
Results
Clinical characteristics of the patients. Age of the examined persons ranged from 25 to 45 years and the mean age was 33.2 (3.7) years. The social status and past medical history data are presented in Table 1.

According to the past medical history, the postoperative period after the CS was complicated by the puerperal endometritis, hyperthermia and/or maturation of the postoperative suture in 15.4% (4/26) of patients from group I and 4.2% (1/24) of patients from group II (p = 0.05), i.e. only 10% of patients with IUS had the acute postpartum infectious and inflammatory diseases.
The clinical presentation of IUS included dysmenorrhea in 19.2% (5/26) and 20.8% (5/24, p = 0.45) of patients, respectively, and postmenstrual spotting in 57.7% (15/26) and 33.3% (8/24, p = 0.04) of patients, respectively.
Features of an objective gynecologic status. Retroflexed uterus was found in 40% (20/50) of patients, namely, 34.6% (9/26) in group I and 45.8% (11/24, p = 0.60) in group II. The defect in the uterine anterior wall was revealed during the vaginal examination in 54% (27/50) of patients.
Results of the laboratory tests. Bacteriological examination (culture from the uterine cavity) was performed according to indications in 14 and 6 patients of groups I and II, respectively. The growth of opportunistic pathogenic microflora was detected in 50% (7/14) and 33.3% (2/6) of patients, respectively (p = 0.18). The expressed microflora was mainly represented by enterococci (E. fecalis) in 56% of cases, enterobacteria (E. coli) in 33% of cases, and by Candida fungi (albicans, krusei) in 22% of cases. In half and more cases (50% and 67%, respectively) the pathogenic causative agents were not identified.
Results of the functional research methods. According to the ultrasound investigation, “niche” (the myometrial defect) was visualized in 100% of cases, the myometrial thickness in the niche apex was 1.7 (0.61) and 1.78 (0.75) mm in groups I and II, respectively (p = 0.39). Moreover, the defect length was 11.8 mm on average and the width was 5.8 mm in both groups. In 30.8% (8/26) and 29.2% (7/24) of patients (p = 0.45), there was a retraction of the uterine outline. In 23.1% (6/26) and 33% (8/24) of the examined people, respectively (p = 0.2), the niches were combined with the fluid inclusions and cavities in the scar area. The comorbid gynecologic conditions were found in 80% (43/50) of patients in both groups: uterine fibroids in 7.7% (2/26) and 4.2% (1/24) of patients, respectively (p = 0.54), and adenomyosis (further confirmed by hysteroscopy) in 76.9% (20/26) and 83.3% (20/24) of women, respectively (p = 0.73).
The signs of scar endometriosis according to the ultrasound examination were found in 28% (14/50) of patients in both groups: 23.1% (6/26) in group I and 33.3% (8/24) in group II (p = 0.2), and the diagnosis was confirmed histologically only in 10% (5/50) of cases.
During hysteroscopy, the special attention was paid to the signs of CE. In aggregate, they were detected not in all patients, and were found only in 23 patients, while morphologically the diagnosis was confirmed in 19 (82.6%) patients. In contrast, in 7 (14%) cases CE was not found according to the hysteroscopic signs, and was identified according to the results of the histological examination.
Based on many years of experience, we have determined hysteroscopic signs of the incompetent scar: the niche in the form of a hemisphere (sometimes with the intersections – “chords”) with the clear even edges which is visualized against a background of the pink endometrium in the lower uterine segment. The niche (or a series of niches in the form of large cells) is inlaid with the white shiny film with the significant vascular tree that is a symptom of “injected sclera”. The “attached” gas bubbles are visualized in the defect area, the foci of endometriosis (black or dark red color) are possible. Along the defect edges on the border with the endometrium, the papillary proliferation is visualized. The bottom niche edge can share border with the internal orifice or develop into the cervical canal, in some patients it looks like the “visor” and makes it difficult to examine the walls and bottom of the defect. The defect is crater-shaped with whitish round edges, occupying the largest part of the lower uterine segment; the defect bottom cannot be examined (as a rule it is a case of isthmocele). During the examination of the niche bottom, the translucent film (peritoneum of the uterovesical fold) is visualized that can confirm the complete myometrial defect.
Features of the ultrasonic and hysteroscopic images using the case of patient K., 31 years old, are shown in Figure 1.

Features of surgical intervention. Additional surgical procedures on the pelvic organs during laparoscopic metroplasty were performed in 56% (28/50) of cases (Table 2).
It is necessary to pay attention to the higher frequency of adhesiolysis and excision of the foci of external endometriosis of the uterosacral ligaments in group I.
The condition of the uterine scar after the laparoscopic metroplasty was evaluated over time (Table 3).
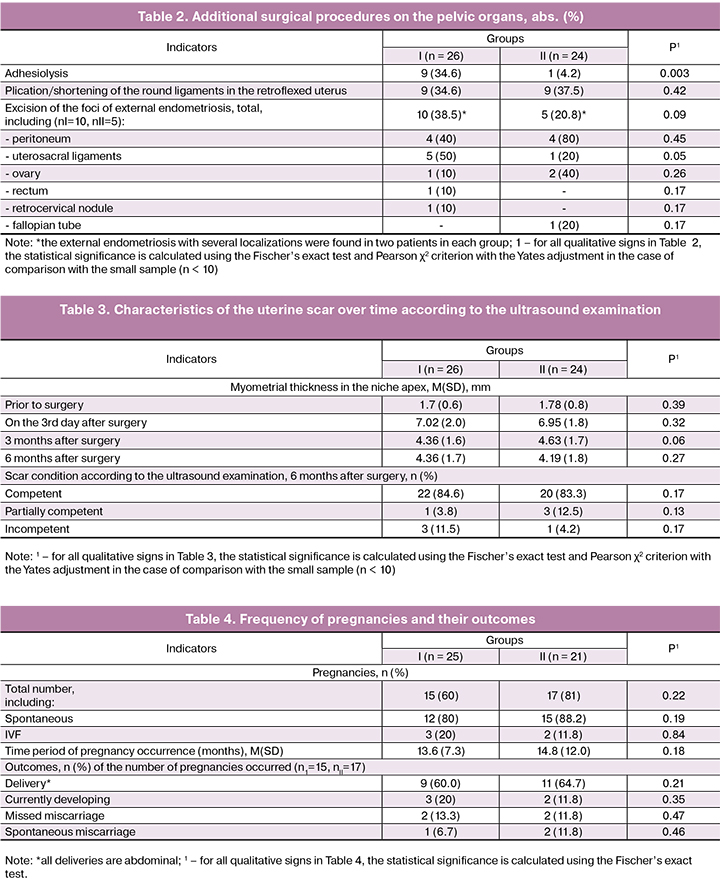
Analysis of Table 3 showed that the statistically significant difference in the results of suture healing after the surgical intervention was not available. However, the negative result of surgical intervention (incompetent scar) in group I was three times as frequently as in group II (in three patients versus one patient, respectively).
Features of the ultrasound image after treatment using the case of patient K., 31 years old, are shown in Figure 2.

The overall effectiveness of metroplasty was 92%. One patient in group I and one patient in group II underwent the repeated laparoscopic metroplasty, in both cases the result was positive and the scar was competent.
The results of the reproductive function implementation (follow-up) are presented in Table 4. We considered the patients who had plans to become pregnant: there were 25 such patients in group I and 21 patients in group II (1 and 3 patients, respectively, refused further pregnancy for different reasons and used contraceptives).
Table 4 shows that the obtained pregnancy indicators and their outcomes do not statistically significantly differ between the groups.
Thus, the background indicators prior to metroplasty in the examined groups were statistically significantly higher in the patients of group I with CE compared with the patients without CE according to the presence of sexually transmitted diseases in the past medical history (11.5% vs. 0%, p = 0.04), perimenstrual spotting (57.7% vs. 33.3%, p = 0.04), adhesive process in the abdominal cavity due to which adhesiolysis was performed (34.6% vs. 4.2%, p = 0.003) and endometriosis of the uterosacral ligaments (50% vs. 20%, respectively, of the number of patients with the identified external endometriosis, p = 0.05). The results of laparoscopic metroplasty were similar in the patients with IUS with CE and without it.
Discussion
Despite the considerable number of studies dedicated to the development of criteria for assessing the uterine scar condition after the CS, the systematic review of the Russian-language studies on the issues of the delivery of patients who underwent operations on the uterus, showed significant diversity in the rate of IUS, namely from 5 to 60% [7].
It is believed that the main reasons leading to the IUS development are the postoperative suppurative-septic complications in the early postoperative period (postpartum endometritis) and the presence of any intrauterine interventions during the first year after the CS [8]. However, in the present study, infectious inflammatory complications after the CS occurred in not more than 10% of patients that means that IUS can be caused by other factors.
More recent attention in literature has focused on the oligosymptomatic course of endometritis, early discharge from an obstetric hospital, late diagnosis of endometritis and uterine scar incompetency [1]. The same authors emphasize that the clinical feature of the formation of incompetent uterine scar is a progressive endometritis which may run two courses: one with severe inflammatory intoxication symptoms (22%) and oligosymptomatic clinical picture with a predominance of asthenic syndrome (30%).
In our opinion, the implementation of surgical methods in the wound surface management of the uterus led to a significant improvement in results of the treatment of postpartum endometritis [6]. However, inadequate attention is paid to the oligosymptomatic forms due to which endometritis runs prolonged chronic course resulting in the formation of the secondary incompetency of the scar.
Our data confirm the thesis of the impact of non-diagnosed, and therefore, non-treated oligosymptomatic forms of postpartum endometritis on the formation of chronic process (52% of patients had CE) that in turn may be one of the factors leading to the partial scar incompetency, and later to the uterine scar after the CS. This is indirectly confirmed by the presence of adhesive process in the anterior recto-uterine pouch (34.6% vs. 4.1% in groups I and II, respectively, p = 0.003) and sexually transmitted diseases in the past medical history (11.5% vs. 0, respectively, p = 0.04) among the examined patients.
In 80% of cases, according to cumulative data of ultrasound examination and hysteroscopy, the studied patients showed adenomyosis that appears to be a factor affecting the IUS development. Postmenstrual spotting which is a sign of clinically significant CE occurred more frequently in group I than in group II (57.7% vs. 33.3%, respectively, p = 0.04); this fact cannot be explained only by the presence of adenomyosis (since its frequency was not statistically significantly different in the compared groups, 77% vs. 83.3%, respectively, p = 0.73) and the degree of the uterine defect (also the same).
We have noted that the diagnostic features of CE detected during hysteroscopy were found only in 82.6% of patients with the CE diagnosis further confirmed morphologically. These data coincide with the research results provided by other authors who have shown that the most informative CE signs, such as uneven endometrial thickness, polypoid vegetation, uneven color and hyperemia of the mucous membrane, are detected hysteroscopically only in 30% of patients. In the meantime, the test sensitivity is only 40%; specificity is 80% (by contrast, the relevant indicators of morphological studies of endometrium aspirates are 93% and 100%) [9]. Therefore, in the case of the suspected CE, hysteroscopy is important for exclusion of the entire range of intrauterine pathologies, but not for verification of the CE diagnosis.
Outcomes of laparoscopic metroplasty performed in the interval period, allowed us to get positive outcomes using the pregnancy occurrence criterion in 60% and 81% of patients in both groups without the statistical difference between them and deliveries in 60% and 64.7%, respectively, and currently developing pregnancy in 20% and 12.5%, respectively. The overall effectiveness of metroplasty was 92%. Absence of the significant difference in the long-term outcomes between the patients with and without CE can be explained by a complex of all measures taken in the perioperative period aimed at preparation for the surgical intervention and rehabilitation performed during the intervention and after it.
Thus, the uterine cavity irrigation by the cavitated solutions in the case of CE has anti-inflammatory effect that was proved on the basis of study of the main inflammatory response mediators (acute phase proteins and cytokine system) in women after missed miscarriage (there is a decrease of the level of IFN-γ and IL-8 concentration by 6 times); it may restore the normal biocenosis and endometrial structure [5].
The therapeutic effect of argon plasma coagulation during metroplasty is based on both direct thermal effect on the microbial agent, and on the activation of reparative processes as a result of deep tissue heating in the suture area [6].
Conclusion
High incidence of chronic endometritis (52%) proves its possible role in the pathogenesis of uterine scar incompetency after the CS. Laparoscopic metroplasty in combination with the preparatory and rehabilitation actions is effective in 92% of cases regardless of the presence or absence of chronic endometritis.
References
- Буянова С.Н., Щукина H.A., Пучкова Н.В. Особенности клинического течения эндомиометрита после кесарева сечения и его исходы. Российский вестник акушера-гинеколога. 2012; 12(5): 84-8. [Buyanova S.N., Shchukina H.A., Puchkova N.V. Features of the clinical course of endomyometritis after cesarean section and its outcomes. Russian Bulletin of the obstetrician-gynecologist. 2012; 12 (5): 84-8. (in Russian)].
- Глухов, Е.Ю., Обоскалова Т.А., Столин А.В., Спирин А.В., Бутунов О.В. Рубец на матке после кесарева сечения в клинике и эксперименте. Российский вестник акушера-гинеколога. 2014; 1: 10-18. [Glukhov, E.Yu., Oboskalova T.A., Stolin A.V., Spirin A.V., Butunov O.V. A scar on the uterus after cesarean section in the clinic and experiment. Russian Bulletin of the obstetrician-gynecologist. 2014; 1: 10-18. (in Russian)].
- Попов А.А., Буянова С.Н., Федоров А.А. Эндоскопические методы диагностики и лечения несостоятельного рубца на матке после кесарева сечения М.: МОНИИАГ; 2010. 124 с. [Popov A.A., Buyanova S.N., Fedorov A.A. Endoscopic methods for the diagnosis and treatment of insolvent scar on the uterus after cesarean section M .: MONIIAH; 2010. 124 p. (in Russian)].
- Tower A.M., Frishman G.N. Cesarean scar defects: an underrecognized cause of abnormal uterine bleeding and other gynecologic complications. J. Minim. Invasive Gynecol. 2013; 20(5): 562-72. DOI: 10.1016/J.JMIG.2013.03.008.
- Кавитированные растворы в репродуктивной медицине. Под ред. В.Е. Радзинского и Е.Ю. Глухова. М.: издательство журнала Status Praesens; 2017. 344 с. [Cavitated solutions in reproductive medicine. Ed. V.E. Radzinsky and E.Yu. Glukhov. M.: Status Praesens magazine publishing; 2017. 344 p. (in Russian)].
- Радиоволна и аргоновая плазма в практике акушера-гинеколога. Под ред. В.Е. Радзинского и Е.Ю. Глухова. М.: издательство журнала Status Praesens, 2016. 216 с. [Radio wave and argon plasma in the practice of an obstetrician-gynecologist. Ed. V.E. Radzinsky and E.Yu. Glukhov. M.: Status Praesens magazine, 2016. 216 p. (in Russian)].
- Телегина И.В., Нежданов И.Г., Павлов Р.В., Аксененко В.А., Демяшкин Г.А. Особенности репарации раны на матке после операции кесарева сечения. Медицинский вестник Северного Кавказа. 2013; 8(2). Эл. ресурс: https://cyberleninka.ru/. [Telegin I.V., Nezhdanov I.G., Pavlov R.V., Aksenenko V.A., Demyashkin G.A. Features of reparation wounds in the uterus after cesarean section. Medical Bulletin of the North Caucasus. 2013; 8 (2). El. resource: https://cyberleninka.ru/. (in Russian)].
- Краснопольский В.И., Логутова Л.С., Буянова С.Н. Несостоятельный рубец на матке после кесарева сечения: причины формирования и лечебная тактика. Акушерство и гинекология. 2013; 12: 28-33. [Krasnopolsky V.I., Logutova L.S., Buyanova S.N. Insolvent uterus scar after cesarean section: causes of formation and treatment tactics. Obstetrics and gynecology. 2013; 12: 28-33. (in Russian)].
- Сухих Г.Т., Шуршалина А.В. Хронический эндометрит: руководство. М.: ГЭОТАР-Медиа; 2013. 64 с. [Sukhikh G.T., Shurshalina A.V. Chronic endometritis: a guide. M .: GEOTAR-Media; 2013. 64 p. (in Russian)].
Received 15.02.2019
Accepted 22.02.2019
About the Authors
Glukhov, Evgeniy Yu., MD, professor of the Department of Obstetrics and Gynecology, Ural State Medical University of the Ministry of Health of Russia.620014, Russia, Yekaterinburg, Sverdlovsk Region, Repina str. 3. Tel .: +73433713490. Chief physician, Center for Operative Gynecology «Women's Clinic».
620066, Russia, Yekaterinburg, Sverdlovsk Region, Botanicheskaya str. 19. Tel .: +73432394713. E-mail: 9222241411@mail.ru.
Dikke, Galina B., MD, associate professor, professor of the Department of Obstetrics and Gynecology with a course of reproductive medicine, Private Educational Institution «Academy of Medical Education named F.I. Inozemtsev».
190013, St. Petersburg, Moscow Ave, 22, letter M. Tel.: +78123347650. E-mail: galadikke@yandex.ru. ORCID.org 0000-0001-9524-8962.
Neff, Ekaterina I., associate professor of medical sciences, Deputy Chief Physician of the Center for Operative Gynecology «Women's Clinic», Ekaterinburg.
620066, Russia, Yekaterinburg, Sverdlovsk Region, Botanicheskaya str., 19. Tel .: +73432394713. E-mail: neff1974@mail.ru
Glukhova, Viktoria E., student, Ural State Medical University, Ministry of Health of Russia.
620014, Russia, Yekaterinburg, Sverdlovsk Region, Repin str. 3. Tel.: +73433713490. E-mail: gluhovav17@mail.ru.
Svyazhina, Anna V., student, Ural State Medical University of the Ministry of Health of Russia.
620014, Russia, Yekaterinburg, Sverdlovsk Region, Repin str., 3. Tel.: +73433713490. E-mail: chizgik@yandex.ru.
For citations: Glukhov E.Yu., Dikke G.B., Neff E.I., Glukhova V.E., Svyazhina A.V. Chronic endometritis and an incompetent uterine scar after cesarean section: long-term outcomes of metroplasty. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2019; (2): 126-34. (in Russian)
http://dx.doi.org/10.18565/aig.2019.2.126-134