Surgical management of placenta accreta spectrum in the Russian Federation (a pilot multicenter study)
Sukhikh G.T., Shmakov R.G., Kurtser M.A., Barinov S.V., Chuprynin V.D., Mikheeva A.A., Amiraslanov E.Yu., Grigoryan A.M., Konoplev B. A.A., Kutakova Yu.Yu., Karapetyan T.E., Vasilchenko O.N., Zabelina T.M., Serova O.F., Pyregov A.V., Kulikov I.A., Belousova T.N., Plakhotina E.N., Penzhoyan G.A., Makukhina T.B., Andreeva M.D., Shapovalova O.A., Kamenskikh G.V., Lobach S.V., Pozdnyakova T.I., Saveljeva I.V., Bukharova E.A., Nosova N.V., Tskhay V.B., Raspopin Yu.S., Garber Yu.G., Wecker I.R., Zhurlova O.N., Nechaeva M.V., Belokoneva T.S., Protopopova N.V., Dudakova V.N., Novichkov D.A., Khvorostukhina N.F., Vladimirova N.Yu., Fedorova K.V., Rinchindorzhieva M.P., Tudupova B.B., Panova T.V., Guseva O.I., Manuilenko O.V., Brum O.Yu., Dorfman O.V., Verovskaya T.A., Babaeva L.K., Rymashevsky A.N., Khvalina T.V., Dmitrieva S.L., Gorev S.N., Malyshkina A.I., Pesikin O.N., Zubenko V.B., Lobach N.V., Briukhacheva T.V., Karavaeva A.A., Bezhenar V.F., Arakelyan B.V., Ralnikova A.Yu., Kurleeva T.Yu., Vologodskaya E.V., Dikareva L.V., Malysheva I.P., Idam-Syuryun A.M., Shakurova E.Yu., Semenov Yu.A., Sherstobitov A.V., Fortygin A.Ia., Ziuzin E.S., Kashlevskaya N.L., Shamina M.S., Gustovarova T.A., Khavansky V.A., Shchegolkov M.E., Kulakova S.A., Klishina V.V.
Objective: This study aimed to analyze the surgical approaches and effectiveness of various methods for managing and preventing bleeding in patients with placenta accreta spectrum disorders in the Russian Federation (RF).
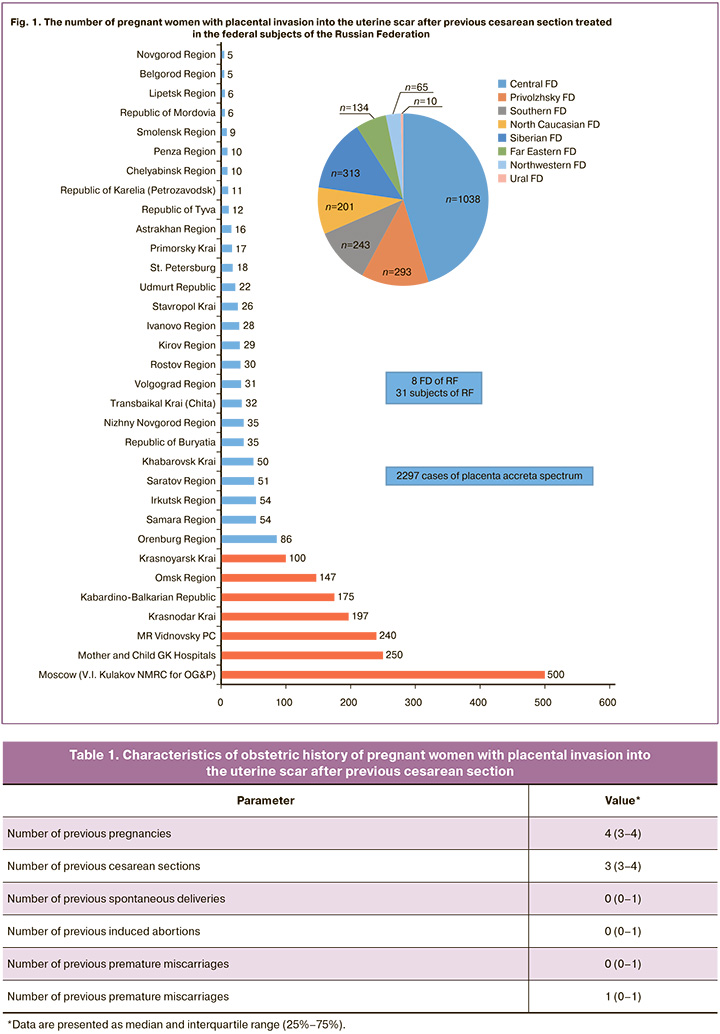
Materials and methods: This retrospective multicenter study analyzed clinical and anamnestic data as well as surgical delivery outcomes of 2297 patients with placenta accreta spectrum who were treated in tertiary-level hospitals over the past 6 years. Data were collected from 33 regions of the Russian Federation, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology of the Ministry of Health of Russia and the Mother and Child Group of Companies.
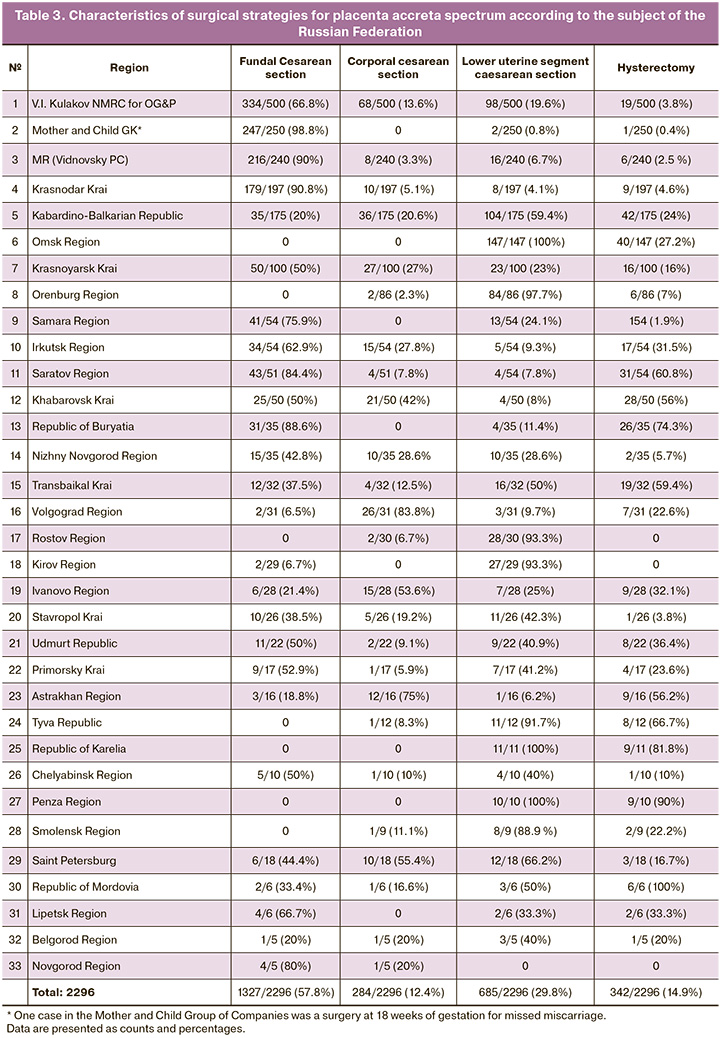
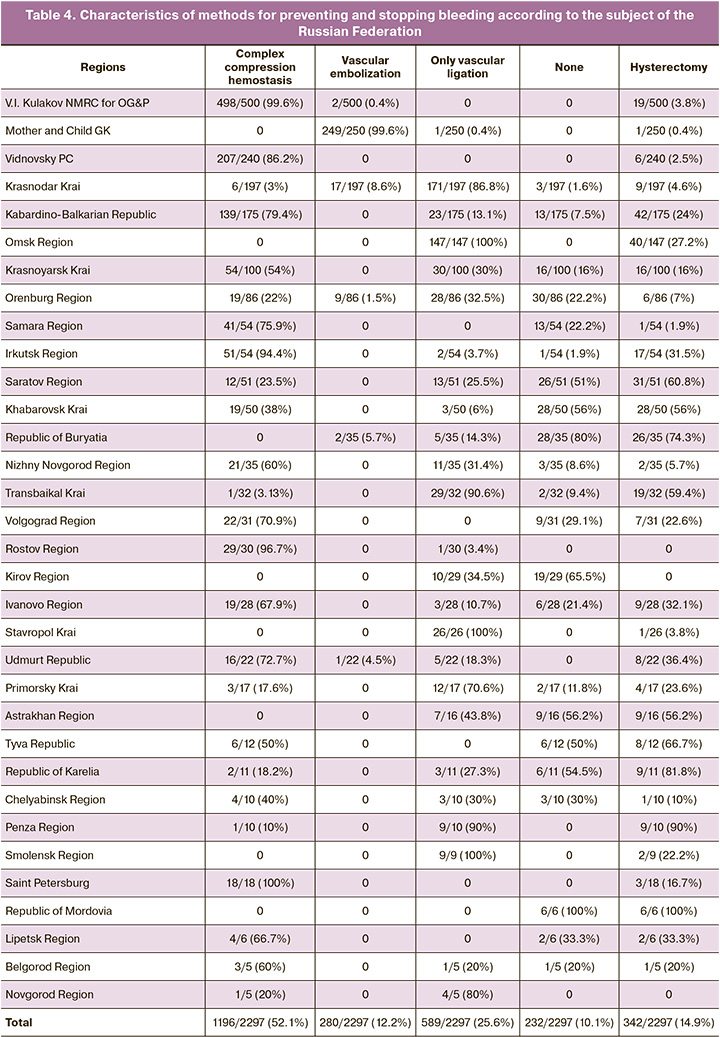
Results: From 2017 to 2023, 2297 patients with placenta accreta spectrum were operated on by multidisciplinary teams of doctors in 33 regions of the Russian Federation. The mean gestational age at delivery was 35.3 (3.3) weeks. Organ-removing surgery was performed in 342 (14.9%) patients, including one surgical delivery at 18 weeks of gestation due to missed miscarriage. Abdominal access techniques included lower midline laparotomy (LML), which was performed in 1954 (85.1%) patients, and transverse suprapubic incision (TSI), which was performed in 343 (14.9%) patients. A fundal uterine incision was used in 1327 (57.7%) patients. Lower uterine segment incision and corporal cesarean sections were performed in 685 (29.9 %) and 284 (12.4%) patients, respectively. The methods used to prevent and stop bleeding included complex compression hemostasis in 1196 (52.1%) patients, temporary balloon occlusion of the common iliac arteries in 280 (12.2%) patients, and other methods in 589 (25.6%) patients.
Conclusion: This pilot multicenter study analyzed the surgical approaches for managing placenta accreta spectrum in various regions of the Russian Federation. The study found that three main methods were used to reduce blood flow in the uterine blood supply system: complex compression hemostasis, ballooning of vessels (internal or common iliac arteries, and aorta), and other methods (ligation of vessels, installation of a vaginal module, and application of compression sutures). Further multicenter prospective studies are necessary to evaluate the factors influencing the development of early and long-term complications and feasibility of subsequent reproductive function.
Conflicts of interest: The authors have no conflicts of interest to declare.
Funding: There was no funding for this study.
Ethical Approval: The study was reviewed and approved by the Research Ethics Committee of the V.I. Kulakov NMRC for OG&P.
Authors' Data Sharing Statement: The data supporting the findings of this study are available upon request from the corresponding author after approval from the principal investigator.
For citation: Sukhikh G.T., Shmakov R.G., Kurtser M.A., Barinov S.V., Chuprynin V.D., Mikheeva A.A., Amiraslanov E.Yu., Grigoryan A.M., Konoplev B.A., Kutakova Yu.Yu., Karapetyan T.E., Vasilchenko O.N., Zabelina T.M., Serova O.F., Pyregov A.V., Kulikov I.A., Belousova T.N., Plakhotina E.N., Penzhoyan G.A., Makukhina T.B., Andreeva M.D., Shapovalova O.A., Kamenskikh G.V., Lobach S.V., Pozdnyakova T.I., Saveljeva I.V., Bukharova E.A., Nosova N.V., Tskhay V.B., Raspopin Yu.S., Garber Yu.G., Wecker I.R., Zhurlova O.N., Nechaeva M.V., Belokoneva T.S., Protopopova N.V., Dudakova V.N., Novichkov D.A., Khvorostukhina N.F., Vladimirova N.Yu., Fedorova K.V., Rinchindorzhieva M.P., Tudupova B.B., Panova T.V., Guseva O.I., Manuilenko O.V., Brum O.Yu., Dorfman O.V., Verovskaya T.A., Babaeva L.K., Rymashevsky A.N., Khvalina T.V., Dmitrieva S.L., Gorev S.N., Malyshkina A.I., Pesikin O.N., Zubenko V.B., Lobach N.V., Briukhacheva T.V., Karavaeva A. A.A., Bezhenar V.F., Arakelyan B.V., Ralnikova A.Yu., Kurleeva T.Yu., Vologodskaya E.V., Dikareva L.V., Malysheva I.P., Idam-Syuryun A.M., Shakurova E.Yu., Semenov Yu.A., Sherstobitov A.V., Fortygin A.Ia., Ziuzin E.S., Kashlevskaya N.L., Shamina M.S.,
Gustovarova T.A., Khavansky V.A., Shchegolkov M.E., Kulakova S.A., Klishina V.V. Surgical management of placenta accreta spectrum in the Russian Federation (a pilot multicenter study).
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2024; (1): 50-66 (in Russian)
https://dx.doi.org/10.18565/aig.2023.306
Keywords
Placenta accreta spectrum is a life-threatening complication of pregnancy, causing massive bleeding, hysterectomy, maternal morbidity, and mortality [1, 2]. Over the past 50 years, there has been a sharp increase in the incidence of this pathology (from 1.7 to 577 per 10,000 births), which may be due to an increase in the frequency of cesarean sections (from 5.5% to 42%) [3, 4]. The increase in the rates of this condition has resulted in a rise in hysterectomies performed during cesarean sections due to an abnormally invasive placenta. The rate of non-organ-sparing surgery for placenta accreta spectrum worldwide averages 46.5% and ranges from 13% to 100%, depending on the surgical technique, material capabilities, and algorithms developed in a particular medical institution [5–7]. Since the 1990s, hysterectomy has been the primary treatment for placenta accreta spectrum. The accumulated experience in managing and delivering pregnant women with this pathology has led to the optimization of surgical strategies, with the main objective of performing metroplasty and preserving fertility [8, 9]. Ensuring adequate hemostasis is the primary requirement for organ-sparing surgery. Currently, several approaches are employed to prevent and stop bleeding, including complex compression hemostasis, temporary occlusion, ligation, embolization, or ballooning of the vessels supplying the uterus. [10–12]. The choice of optimal method for stopping bleeding is based on the clinical and technical capabilities of the medical institution.
Despite the 2022 Clinical Guidelines "Pathological Attachment of the Placenta (Previa and Placenta Accreta Spectrum)”1, which clearly stipulates the timing of delivery, the type of laparotomy, the volume, and method of performing surgical intervention, there are still many controversial and unresolved issues requiring constant study, practical application, and, if necessary, revision.
This study aimed to determine the characteristics of the surgical approaches and the effectiveness of various methods for stopping and preventing bleeding in the placenta accreta spectrum in the Russian Federation.
Materials and methods
This study retrospectively analyzed the characteristics of surgical approaches and methods for stopping and preventing bleeding in the placenta accreta spectrum in the Russian Federation. Information letters were sent to chief non-staff specialists in obstetrics and gynecology in 85 federal subjects of the Russian Federation. Information was provided by 33 federal subjects of the Russian Federation, as well as by Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology, and Perinatology, Ministry of Health of Russia, and the hospitals of the Mother and Child Group of Companies. The study included 2297 pregnant women with placenta accreta spectrum who were examined and delivered in tertiary-level hospitals over the past 6 years. The number of patients varied from 5 to 500 in different subjects (Fig. 1). The largest number of cases was in the V.I. Kulakov NMRC for OG&P (n=500), hospitals of the Mother and Child Group of Companies (n=250), Vidnovsky PC (n=240), Krasnodar Krai (n=197), Kabardino-Balkarian Republic (n=175), Omsk Region (n =147) and Krasnoyarsk Krai (n=100).
Results and discussion
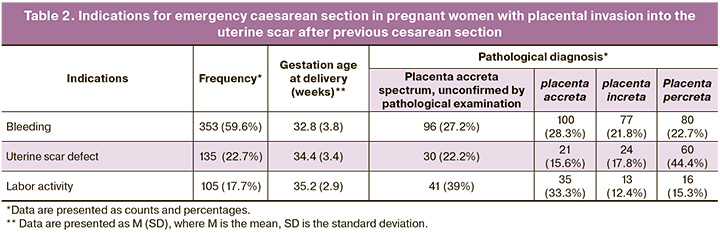
From 2017 to 2023, 2297 patients with placenta accreta spectrum were operated on by multidisciplinary teams of doctors in 33 regions of the Russian Federation.The mean age in the study group was 34 (4,5) years (range: 23–46 years). On an average, this pregnancy was fourth (3–5) in a row. Patients had a history of 2–6 cesarean sections (3 (3–5)), and 191/2297 (8.3%) of the study population had no history of cesarean section. None of the patients included in the study had a history of placenta accreta spectrum or placenta previa. Every third pregnant woman had a history of spontaneous physiological labor (0 (0–1)), every second had an induced termination of pregnancy (0 (0–1)), and an early miscarriage (0 (0–1)). A history of dilation and curettage was observed in 921/2297 (40.1%) patients (1 (0–1)); indications for surgery were the remains of the fetal egg, placental tissue, and lochiometra (Table 1).
In 212/2297 (9.2%) patients the gynecological history was characterized by chronic endometritis as a result of invasive intrauterine procedures (dilatation and curettage), in 178/2297 (7.7%) by large uterine fibroids, in 122/2297 (5.3%) by endometriosis, in 35/2297 (1.5%) by congenital uterine defects (bicornuate uterus). In 191/2297 (8.3%) cases, patients with a complicated gynecological history (history of intrauterine invasive manipulation and chronic endometritis) were diagnosed with true placenta accreta spectrum without a post-cesarean uterine scar.
Pregnancy occurred spontaneously in all patients, and placenta previa was diagnosed in the early stages of pregnancy. Primary diagnosis of placenta accreta spectrum overlying a cesarean section scar according to ultrasound examination (ultrasound) occurred at 23.3 (7.4) weeks of pregnancy. After confirming the diagnosis using magnetic resonance imaging (MRI), the patient was referred to a tertiary hospital for further pregnancy management, examination, and delivery. The patients were examined in accordance with Order of the Ministry of Health of the Russian Federation dated October 20, 2020 No. 1130n “On approval of the procedure for providing medical care in the field of obstetrics and gynecology.” The mean gestational age at the time of hospitalization was 34.4 (6.4) weeks. The gestational age at the time of delivery depended on the estimated depth of the placenta accreta spectrum according to ultrasound and MRI and averaged 35.3 (3.3) weeks. In the Mother and Child Group of Companies, one patient underwent surgery at 18 weeks due to a missed miscarriage.
Despite planning the operation at 34–36 weeks of pregnancy (according to clinical guidelines), 593/2297 (25.8%) women had an emergency caesarean section including 353/593 (59.6%) due to bleeding, 135/593 (22.7%) due to uterine cesarean scar defects, and 105/593 (17.7%) due to the onset of regular labor (Table 2).
Abdominal access techniques included lower midline laparotomy (LML), which was performed in 1954 (85.1%) patients, and transverse suprapubic incision (TSI), which was performed in 343 (14.9%) patients.
Diametrically different approaches for surgical access to the abdominal cavity for placenta accreta spectrum have been established. For example, in the Orenburg Region, in 96.5% of cases with placenta accreta spectrum (83 out of 86 cases), access to the abdominal cavity was performed using TSI. In 10 federal subjects of the Russian Federation (Moscow, Astrakhan, Belgorod, Kirov, Novgorod, Omsk, Penza, Smolensk regions, Stavropol Krai and the Republic of Tyva) this method was not used; in 100% of cases LML was used. It should be noted that the clinical guidelines “Pathological attachment of the placenta (previa and placenta accreta spectrum)” recommend laparotomy with access sufficient to perform the full scope of surgical intervention, and the commentary notes that in case of placenta accreta spectrum, a lower midline laparotomy is preferable. However, in our opinion, the choice of laparotomy method should be up to the operating surgeon, who has sufficient experience in performing such operations and should not be limited to midline laparotomy.
The next important surgical step was the choice of uterine incision level (uterotomy). Uterine fundal incision was the most frequently used uterine incision in 1327/2297 (57.7%) patients. In V.I. Kulakov NMRC for OG&P this incision was used in 334/500 (66.8%) cases, in Mother and Child Group of Companies in 247/250 (98.8%) cases, in Vidnovsky PC in 216/240 (90%) cases, in Krasnodar Krai in 179/197 (90.8%) cases. However, it has never been used in the Omsk, Orenburg, Rostov, Penza, and Smolensk regions, the Republics of Tyva, or Karelia.
Lower uterine segment incision and corporal cesarean section were performed more rarely in 685/2297 (29.9%) and 284/2297 (12.4%) patients, respectively. A corporal cesarean section was most often performed in the Volgograd Region in 26/31 (83.8%) patients. All patients in the Omsk and Penza regions as well as in the Republic of Karelia underwent cesarean section with a lower uterine segment incision (Table 3).
It should be emphasized that the choice of uterine incision should be based on the estimated severity of abnormal placental implantation according to ultrasound and MRI. For placenta percreta and placenta increta, fundal uterine incision is preferable; with other types of placenta accreta spectrum or severe placental attachment, it is possible to make both fundal and corporal uterine incisions (above the edge of the placenta), or even in some cases, in the lower uterine segment. However, it is important to note that the incision should be made outside the area of placental implantation, both with placenta accreta spectrum and placenta previa without abnormal placental implantation, to reduce blood loss. Therefore, intraoperative use of ultrasound navigation is crucial. Clear definitions of the level of uterine incision, specifically for placenta accreta spectrum, are also necessary. Thus, during a cesarean section, a transverse lower uterine segment incision, a corporal incision along the midline of the uterine body (“classic”), and J- and T-shaped incisions are used. However, the method of choice for placenta accreta spectrum differs from the standard method. Most often, surgeons choose a fundal uterine incision. When a choice between a lower segment or corporal incision is possible, the surgeon more often chooses the corporal incision after an intraoperative assessment of invasion severity. Lower uterine segment incision is extremely rare when the placenta is located predominantly along the posterior wall, with a slight transition to the anterior wall. Therefore, it may be necessary to combine these types of incision into a transverse corporal incision along the top of the placenta.
The main stage in the operation for placenta accreta spectrum is the method of reducing the blood supply to the uterus to reduce blood loss volume [13]. The methods used to prevent and stop bleeding included complex compression hemostasis (CCH) in 1196/2297 (52.1%) patients, temporary balloon occlusion (TBO) of the common iliac arteries in 280/2297 (12.2%) patients, and mixed methods (vessel ligation, use of a vaginal module, compression sutures) in 589/2297 (25.6%) patients. In 232/2297 (10.1%) cases, no method for preventing or stopping bleeding was used.
CCH was the most frequently used hemostatic technique at the V.I. Kulakov NMRC for OG&P – 498/500 (99.6%), St. Petersburg – 18/18 (100%), Rostov Region – 29/30 (96.7%), Irkutsk Region – 51/54 (94.4%), Vidnovsky PC – 211/240 (86.2%); in 87.9% CCH was combined with the use of a vaginal module, in the Kabardino-Balkar Republic – 139/175 (79.4%), Samara Region – 41/54 (75.9%); Udmurt Republic – 16/22 (72.7%); Volgograd Region – 22/31 (70.9%); Ivanovo Region – 19/28 (67.9%); Lipetsk Region – 4/6 (66.7%); Nizhny Novgorod Region – 21/35 (60%); Belgorod Region – 3/5 (60%); Republic of Tyva – 6/12 (50%) and Chelyabinsk Region – 4/10 (40%). CCH was not used in the Mother and Child Group of Companies, Astrakhan, Kirov, Omsk, Smolensk regions, or Buryat and Mordovian Republics. In 824/1196 (68.9%) cases, CCH was sufficient to provide adequate hemostasis and metroplasty. In cases of persistent bleeding despite the use of this method, ligation of the uterine arteries was performed in 188/1196 (15.72%) patients and internal iliac arteries in 100/1196 (8.36%) patients, or a combination of both in 28/1196 (2. 34%) cases. The mean blood loss during the use of this method was 1648.15 (1099.17) ml. It should be noted that at the V.I. Kulakov NMRC for OG&P, where this method was invented, tested and introduced into regional practice, the mean blood loss was 973 ml. Organ-sparing surgery was performed in 1150/1196 (96.15%) cases. According to the pathomorphological study, placenta accreta spectrum was confirmed in 1145/1196 (95.7%) cases (placenta accreta – 470/1196 (39.3%); increta – 307/1196 (25.7%); percreta – 368/1196 (30.8%)).
TBO of the common iliac arteries was used in 280/2297 (12.2%) cases. Most cases using this method were in the Mother and Child Group of Companies, with 249/250 (99.6%) patients. The mean blood loss in the Mother and Child group was 1518 (958) ml (400–2900 ml). A total hysterectomy with bilateral adnexectomy was performed in one case (0.4%); in this case, the placenta accreta spectrum was combined with multiple uterine fibroids.
Among the federal subjects of the Russian Federation, vascular embolization was performed in 31/2297 (1.3%) cases. In 4 cases, embolization of the uterine vessels was performed after a cesarean section and delayed (7–14 days) relaparotomy, followed by hysterectomy/metroplasty, in case of severe invasion of the cervix and bladder (placenta percreta) to reduce blood supply and blood loss volume. The mean blood loss volume when using this method in the regions was 2037.24 (1188.34) ml, and total hysterectomy with bilateral adnexectomy was performed in 5/31 (16%) cases. In 30/31 (96.8%) cases, placenta accreta spectrum was confirmed by pathological examination (placenta accrete – 19/31 (61.3%); increta – 6/31 (19.4%); and percreta – 5/31 (16.1%)).
Of the mixed methods, ligation of the major vessels, including the uterine and internal iliac arteries, use of a vaginal module, and application of compression sutures were used as the primary methods to reduce blood supply to the uterus in 589/2297 (25.6%), including the Omsk Region – 147/147 (100%); Smolensk Region – 6/6 (100%); Transbaikal Region – 29/32 (90.6%); Penza Region – 9/10 (90%); Krasnodar Region – 171/197 (86.8%); Novgorod Region – 4/5 (80%); and Primorsky Krai – 12/17 (70.6%). Of the 589 cases in which mixed hemostatic techniques were used, uterine artery ligation was used as an independent method of hemostasis in 245 (41.6%). The mean blood loss was 1952.14 (1315.36) ml, and the hysterectomy rate was 102/589 (17.35%). According to the pathomorphological study, placenta accreta spectrum was confirmed in only 318/589 (53.9%) cases (placenta accrete – 174/589 (29.7%); increta – 92/589 (15.7%); and percreta – 52/589 (8.8%)).
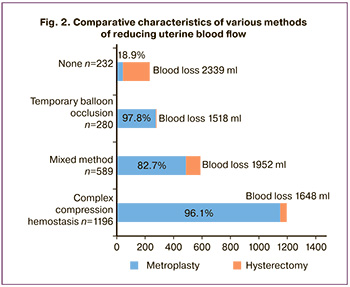
In 232/2297 (10.1%) cases, no method of reducing the blood supply to the uterus was used, while the mean blood loss was 2339.56 (1503.04) ml, and the rate of hysterectomies was 188/232 (81%). In 183/323 (78.9%) cases, placenta accreta spectrum was confirmed by pathological examination (Fig. 2, Table 4).
The feasibility of organ-sparing surgery is a key issue in placenta accreta. First, many women with placenta accreta spectrum have raised the issue of preserving their reproductive function. Second, in the vast majority of cases, if the correct surgical technique is mastered, it is possible to preserve the organ with minimal blood loss without the occurrence of a life-threatening condition for the mother. However, this depends on the level of medical organization, the level of training of the surgical, anesthesia, and transfusion teams, and the severity of the invasion. Therefore, an individual approach is required for each case [14].
Intraoperative hysterectomy was performed in 319/342 patients (93.3% of total hysterectomies) because of uncontrollable massive bleeding (3022.53 (1611.27) ml). In 10/342 (2.9%) cases, organ removal was performed as planned because of the severe type of placenta accreta spectrum (cervical and parametrial invasion). In 12/342 (3.6%) cases, the reason for hysterectomy was early postpartum hemorrhage (mean volume of early postpartum hemorrhage – 1794.23 (1362.76) ml). Hysterectomy was performed in 1/342 (0.2%) cases because of the presence of multiple uterine fibroids.
Delayed hysterectomy was performed in 48 cases, of which early postpartum hemorrhage occurred in 75% (36/48). Relaparotomy was performed due to peritonitis in 9/48 (18.8%) cases and endometritis in 3/48 (6.2%) cases.
In order to correct hemodynamic disorders in cases of massive blood loss, autotransfusion of processed erythrocytes was performed in 100% of cases, in 397/2297 (17.3%) transfusions of fresh frozen plasma (mean volume – 1119.48 (609.86) ml), and 377/2297 (16.4%) transfusions of erythrocytes (mean volume, 760.94 (537.39) ml).
To reduce the risk of early postpartum hypotonic bleeding, intrauterine balloon tamponade was used in 593/2297 (25.8%) patients (exposure of the uterine balloon for a mean of 2–12 h). Despite the use of this technique, 19/593 (3.2%) patients experienced early postpartum hemorrhage, with a mean blood loss of 1241.25 (347.45) ml. Among the 1704 patients who did not undergo intrauterine balloon tamponade, early postpartum hemorrhage occurred in 15 patients (0.9%), with a mean blood loss of 1026.74 (114.98) ml. Thus, the use of intrauterine balloon tamponade for the prevention of postpartum hemorrhage is currently controversial in terms of its effectiveness and requires a randomized trial.
According to a pathomorphological study, placenta accreta spectrum was confirmed in 1652/2297 (71.9%) cases; in other cases, the diagnosis was not confirmed. Placenta accreta was diagnosed in 769/1652 (46.5%) cases (mean blood loss 1789.79 (1247.58) ml), placenta increta in 557/1652 (33.7%) cases (mean blood loss 1736.24 (1246.93) ml), and placenta percreta in 326/1652 (19.8%) cases (mean blood loss 1727.35 (1253.78) ml). The mean length of hospitalization was 7.6 (3.4) days.
Conclusions
- In general, with the emergence of the placenta accreta spectrum epidemic in the Russian Federation, a favorable situation has developed with the possibility of performing operations with good results for the mother and newborn. Maternal mortality in patients with placenta previa and placenta accreta spectrum was 1 case in 2021, 3 cases in 2022, and 2 cases in 2023.
- The safe gestational age for delivery in patients with placenta accreta spectrum is 35–36 weeks owing to the increased risk of bleeding after this period. In this study, the mean time at delivery was 35.3 (3.3) weeks; however, even taking this circumstance into account, in 593 (25.8%) cases the surgery was performed urgently due to the development of bleeding, suspected uterine scar defect, or the onset of labor.
- A uterine incision must be made outside the placental bed to reduce blood loss. The safest method, especially for severe forms of abnormally invasive placenta, is fundal uterine incision. The incision along the upper edge of the placenta is most often made in the area of the uterine body and is therefore called a "transverse corporal incision.” In rare cases, lower uterine segment incision is possible if the placenta is mainly located along the posterior wall.
- Three main methods are used to reduce blood flow in the uterine blood supply system. CCH, with possible additional ligation of the uterine arteries and internal iliac arteries and temporary clipping of the common iliac arteries, is the most accessible and most often used procedure in the Russian Federation and has good indicators in terms of blood loss and the possibility of performing organ-sparing surgery. The high-tech method of ballooning vessels (internal or common iliac arteries, aorta) has shown good effectiveness in the possibility of performing organ-sparing operations and reducing the volume of blood loss, but it is not widely available in the regions of the Russian Federation. The use of other methods (vascular ligation, installation of a vaginal module, compression sutures, or, as data from some regions have shown, the absence of any technologies that reduce blood supply to the uterus) depends on the qualifications of the surgeon and the traditions of the institution, and is inevitably associated with the lack of high-tech equipment.
- In this study, only 342 patients (14.9%) underwent organ-removing surgery. The obtained results indicate a greater possibility of preserving a woman's reproductive function in comparison with colleagues from Europe, North America, and South America. It is necessary to further improve surgical methods for placenta accreta spectrum and introduce organ-sparing surgery for the possible implementation of reproductive function in these women.
Conclusion
For the first time in the Russian Federation, a large-scale study was conducted on one of the most pressing problems in the modern obstetrics–placenta accreta spectrum. The limitations of this study include its retrospective data analysis, the use of different technical and surgical options, the lack of a uniform protocol for preoperative examination, different methods of recording blood loss, and the difficulty in determining the degree of placental invasion based on histological findings. This study is the first (preliminary) stage before conducting a prospective multicenter study on placenta accreta spectrum in the Russian Federation.
____________________
1 https://drive.google.com/file/d/1bjepiVL5-kUPfxuqa4anT8NsLV9dWFr6/view
References
- Wang Y., Zhou Y., Zeng L., Chen L., Zhao Y. Analysis of risk factors for massive intraoperative bleeding in patients with placenta accreta spectrum. BMC Pregnancy Childbirth. 2022; 22(1):116. https//dx.doi.org/10.1186/s12884-022-04391-x.
- Baldwin H.J., Nippita T.A., Torvaldsen S., Ibiebele I., Ford J.B., Patterson J.A. Outcomes of subsequent births after placenta accreta spectrum. Obstet. Gynecol. 2020; 136(4): 745-55. https//dx.doi.org/10.1097/AOG.0000000000004051.
- Hobson S.R., Kingdom J.C., Murji A., Windrim R.C., Carvalho J.C.A., Singh S.S. et al. No. 383-screening, diagnosis, and management of placenta accreta spectrum disorders. J. Obstet. Gynaecol. Can. 2019; 41(7):1035-49. https//dx.doi.org/10.1016/j.jogc.2018.12.004.
- Parveen F., Aijaz S., Aijaz W., Qureshi N. Frequency of obstetrical hysterectomy in morbidly adherent placenta in vomen with previous cesarean section in tertiary care hospital. Pak. J. Med. Heal. Sci. 2023; 17(3): 534-6. https://dx.doi.org/10.53350/pjmhs2023173534.
- Ikram-ul-haq A., Sadiq N., Bashir S., Waheed N., Shabana N., Aqsa U. Emerging trends in peripartum hysterectomy; a high alert in obstetrics. J. Rawalpindi Med. College (JRMC). 2021; 25(3): 395-9. https://dx.doi.org/10.37939/jrmc.v25i3.1664.
- Tahseen H., Khokhar S., Qurban S., Khurshid N., Tayyab M., Muneer N. Morbidly adherent placenta in patients with placenta previa and feto-maternal outcomes. J. Soc. Obstet. Gynaecol. Pak. 2023; 13(2): 69-72.
- Palacios-Jaraquemada J.M., Fiorillo A., Hamer J., Martínez M., Bruno C. Placenta accreta spectrum: a hysterectomy can be prevented in almost 80% of cases using a resective-reconstructive technique. J. Matern. Fetal Neonatal Med. 2022; 35(2): 275-82. https://dx.doi.org/10.1080/14767058.2020.1716715.
- Михеева А.А., Шмаков Р.Г., Рогачевский О.В., Ярыгина Т.А., Низяева Э.Ю., Амирасланов Э.Ю. Возможности сохранения репродуктивной функции у женщин после органосохраняющих операций при врастании плаценты. Акушерство и гинекология. 2022; 1: 90-6. [Mikheeva A.A., Shmakov R.G., Rogachevskiy O.V., Yarygina T.A., Nizyaeva N. V., Amiraslanov E.Yu. Fertility preservation in women with placenta accreta spectrum undergoing organ-sparing surgery. Obstetrics and Gynecology. 2022; (1): 90-6. (in Russian)]. https://dx.doi.org/10.18565/aig.2022.1.90-96.
- Патент RU 2 626 984 C1. Шмаков Р.Г., Чупрынин В.Д., Виницкий А.А. Способ двухуровнего гемостаза при выполнении органосохраняющего оперативного родоразрешения у пациенток с врастанием плаценты. Заявка: 2016139121, 2016.10.05. Опубликовано: 2017.08.02. [PatentRU 2 626 984 C1. Shmakov R.G., Chuprynin V.D., Vinitskij A.A. Method of two-level hemostasis when performing organ-preserving operative delivery in patients with placenta ingrowth. Application 2016139121, 2016.10.05. Publ. 2017.08.02. (in Russian)].
- Курцер М.А., Бреслав И.Ю., Григорьян А.М. Латышкевич О.А., Кутакова Ю.Ю.,Кондратьева М.А. Временная баллонная окклюзия общих подвздошных артерий при осуществлении органосохраняющих операций у пациенток с врастанием плаценты. Акушерство и гинекология: новости, мнения, обучение. 2018; 6(4): 31-7. [Kurtser M.A.,Breslav I.Yu., Griogorian A.M., Latushkevich O.A., Kutakova Yu.Yu., Kondratieva M.A. Temporary balloon occlusion of common iliac arteries during organ preservation surgery in patients with placenta ingrowth. Obstetrics and Gynecology: news, opinions, training. 2018; 6(4): 31-7. (in Russian)]. https//dx.doi.org/10.24411/2303-9698-2018-14003.
- Abbas S., Shaikh F., Nabila Hasan S. Fetomaternal outcome in morbidly adherent placenta. Pak. J. Med. Heal. Sci. 2023; 17(1): 39-41. https://dx.doi.org/10.53350/pjmhs2023171139.
- Виницкий А.А., Шмаков Р.Г., Чупрынин В.Д. Сравнительная оценка эффективности методов хирургического гемостаза при органосохраняющем родоразрешении у пациенток с врастанием плаценты. Акушерство и гинекология. 2017; 7: 68-74. [Vinitsky A.A., Shmakov R.G., Chuprynin V.D. Comparative evaluation of the efficiency of surgical hemostatic techniques during organ-sparing delivery in patients with placenta increta. Obstetrics and Gynecology. 2017; (7): 68-74. (in Russian)]. https://dx.doi.org/10.18565/aig.2017.7.68-74.
- Barinov S.V., Shmakov R.G., Medyannikova I.V., Tirskaya Y.I., Kadtsyna T.V., Lazareva O.V. et al. Efficacy of distal haemostasis during caesarean delivery in women with placenta accreta spectrum disorders. J. Matern. Fetal Neonatal Med. 2022; 35(25): 8778-85. https://dx.doi.org/10.1080/14767058.2021.2005019.
- Palacios-Jaraquemada J.M., D’Antonio F., Buca D., Fiorillo A., Larraza P. Systematic review on near miss cases of placenta accreta spectrum disorders: correlation with invasion topography, prenatal imaging, and surgical outcome. J. Matern. Fetal Neonatal Med. 2020; 33(19): 3377-84. https://dx.doi.org/10.1080/14767058.2019.1570494.
Received 28.12.2023
Accepted 18.01.2024
About the Authors
Gennady T. Sukhikh, Academician of the Russian Academy of Sciences, MD, PhD, Professor, Director, Academician V.I. Kulakov National Medical Research Centerfor Obstetrics, Gynecology, and Perinatology, Ministry of Health of Russia, 117997, Russia, Moscow, Oparin str., 4, g_sukhikh@oparina4.ru,
https://orcid.org/0000-0002-7712-1260
Roman G. Shmakov, MD, PhD, Professor, Professor of the Russian Academy of Sciences, Deputy General Director of the Mother and Child Group of Companies;
Chief non-staff obstetrics specialist of the Ministry of Health of Russia, 117997, Russia, Moscow, Ostrovityanov str., 1, r.shmakov@mcclinics.ru,
https://orcid.org/0000-0002-2206-1002
Mark A. Kurtser, Academician of the Russian Academy of Sciences, MD, PhD, Professor, Head of the Department of Obstetrics and Gynaecology (named after Academician G.M. Savelieva), Pediatric Faculty, N.I. Pirogov Russian National Research Medical University, Ministry of Health of Russia, 117997, Russia, Moscow, Ostrovityanov str., 1, +7(495)719-78-96, m.kurtser@mcclinics.ru, https://orcid.org/0000-0003-0175-1968
Sergey V. Barinov, MD, PhD, Professor, Head of the Department of Obstetrics and Gynecology №2, Omsk State Medical University, Ministry of Health of Russia,
644099, Russia, Omsk, Lenin str., 12, +7(913)633-80-48, barinov_omsk@mail.ru, https://orcid.org/0000-0002-0357-7097
Vladimir D. Chuprynin, PhD, Head of the Surgical Department, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology, and Perinatology, Ministry of Health of Russia, 117997, Russia, Moscow, Oparin str., 4, v_chuprynin@oparina4.ru, https://orcid.org/0000-0002-2997-9019
Alexandra A. Mikheeva, PhD, doctor of the 2nd Department of Obstetrics, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia, 117997, Russia, Moscow, Oparin str., 4, shuratora@mail.ru, https://orcid.org/0000-0002-8159-6373
Elrad Yu. Amiraslanov, PhD, Head of the Department of Obstetrics, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology, and Perinatology, Ministry of Health of Russia, 117997, Russia, Moscow, Oparin str., 4, eldis@mail.ru, https://orcid.org/0000-0001-5601-1241
Ashot M. Grigoryan, PhD, Head of the Interventional Cardiology Department, Lapino Clinical Hospital, https:/orcid.org//0000-0001-9226-0130
Boris A. Konoplev, Obstetrician-Gynecologist, General Manager of HAVEN (Lapino Clinical Hospital) of the Mother and Child Group of Companies,
143030, Russia, Moscow region, Odintsovo district, 1st Uspenskoe highway, 111, +7(495)139-87-26, b.konoplev@mcclinics.ru, https://orcid.org/0000-0001-6347-4375
Yulia Yu. Kutakova, PhD, Medical Manager of the Mother and Child Group of Companies for organizational, scientific and educational work, 143081, Russia, Moscow region, Odintsovo district, Lapino village, 1st Uspenskoe highway 111, y.kutakova@mcclinics.ru
Tamara E. Karapetyan, MD, PhD, doctor of the Obstetric Department, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology, and Perinatology, Ministry of Health of Russia, 117997, Russia, Moscow, Oparin str., 4, tomamed02@mail.ru, https://orcid.org/0000-0003-0025-3182
Oksana N. Vasilchenko, PhD, doctor of the 2nd Maternity Department, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology, and Perinatology, Ministry of Health of Russia, 117997, Russia, Moscow, Oparin str., 4, o_vasilchenko@oparina4.ru, https://orcid.org/0000-0002-5348-8017
Tatyana M. Zabelina, PhD, doctor at Maternity Department, Perinatal Center of City Clinical Hospital No. 31 named after Academician G.M. Savelyeva,
119421 Russia, Moscow, Novatorov str., 3, romashova-1993@bk.ru, https://orcid.org/0009-0005-0344-2669
Olga F. Serova, MD, PhD, Professor, Head Physician of Moscow Regional Perinatal Center, Balashikha; Chief non-staff specialist in obstetric services of the Ministry of Health of the Moscow Region, +7(916)193-46-38, olga-serova@yandex.ru, https://orcid.org/0000-0002-4088-4619
Аlexey V. Pyregov, MD, PhD, Professor, Deputy Head Physician of Moscow Regional Perinatal Center, Balashikha; Chief non-staff specialist in anaestesiology-reanimatology
of the Ministry of Health of the Moscow Region, +7(916)140-65-49, pyregov@mail.ru, https://orcid.org/0000-0001-8382-9671
Ilyas A. Kulikov, PhD, Head of the Department of Pregnancy Pathology, Vidnovsky Perinatal Center, 142700, Russia, Moscow Region, Zavodskaya str., 17, +7(916)752-86-97, aesculap@inbox.ru, https://orcid.org/0000-0002-2460-1623
Tamara N. Belousova, PhD, Head Physician, Vidnovsky Perinatal Center, 142700, Russia, Moscow Region, Zavodskaya str., 17, beltamara1@mail.ru,
https://orcid.org/0000-0003-3804-7691
Elena N. Plakhotina, MD, PhD, Head of the Department of Anesthesiology and Intensive Care, Vidnovsky Perinatal Center,
142700, Russia, Moscow Region, Zavodskaya str., 17, enp2004@inbox.ru, https://orcid.org/0000-0002-6793-2318
Grigory A. Penzhoyan, Head of the Department of Obstetrics, Gynecology and Perinatology, Faculty of Advanced Training and Professional Retraining of Specialists,
Kuban State Medical University, MD, Professor, 350012, Russia, Krasnodar, Krasnykh Partizan str., 6/2, pga05@mail.ru, https://orcid.org/0000-0002-8600-0532
Tatiana B. Makukhina, PhD, Associate Professor of the Department of Obstetrics, Gynecology and Perinatology, Faculty of Advanced Training and Professional Retraining of Specialists, Kuban State Medical University, Ministry of Health of Russia, 350012, Russia, Krasnodar, Krasnykh Partisan str., 6/2, soltatiana@mail.ru,
https://orcid.org/0000-0003-0536-4500
Margarita D. Andreeva, Chief non-staff specialist in obstetrics at the Ministry of Health of the Krasnodar Territory; Professor of the Department of Obstetrics,
Gynecology and Perinatology, Faculty of Advanced Training and Professional Retraining of Specialists, Kuban State Medical University, Ministry of Health of Russia, MD,
350012, Russia, Krasnodar, Krasnykh Partizan str., 6/2, +7(861)222-05-43, andreeva_md@mail.ru, https://orcid.org/0000-0002-6524-3965
Olga A. Shapovalova, Deputy Chief Physician in Obstetrics and Gynecology, Regional Clinical Hospital No. 2, Ministry of Health of the Krasnodar Territory, PhD,
350012, Russia, Krasnodar, Krasnykh Partizan str., 6/2, +7(861)222-04-83, shapovalova_25@mail.ru
Gayane V. Kamenskikh, obstetrician-gynecologist at the Obstetric Observational Department, Regional Clinical Hospital No. 2, Ministry of Health of the Krasnodar Territory, PhD, 350012, Russia, Krasnodar, Krasnykh Partizan str., 6/2, +7(861)222-04-83, gaene@mail.ru
Svetlana V. Lobach, Head of the Department of Obstetric Pathology of Pregnant Women No.1, Regional Clinical Hospital No. 2, Ministry of Health of the
Krasnodar Territory, Obstetrician-gynecologist of the highest category, 350012, Russia, Krasnodar, Krasnykh Partizan str., 6/2, +7(861)222-04-83, lobach_sv@mail.ru
Tamara I. Pozdnyakova, PhD, Deputy Chief Medical Officer, Kabardino-Balkarian Republican Perinatal Center, Ministry of Health of Kabardino-Balkarian Republic,
360032, Russia, KBR, Nalchik, Shogenova str., 34, +7(928)709-93-95, perinatal.nalchik@mail.ru
Irina V. Saveljeva, MD, PhD, Professor, Head of the Department of Obstetrics and Gynecology № 1, Omsk State Medical University, Ministry of Health of Russia,
644099, Omsk, Russia, Lenin str., 12, +7(913)654-35-77, saveljeva_iv_omsk@mail.ru, https://orcid.org/0000-0001-9342-7342
Elena A. Bukharova, PhD, Teaching Assistant at the Department of Obstetrics and Gynecology No. 1, Omsk State Medical University, Ministry of Health of Russia,
644099, Omsk, Russia, Lenin str., 12, +7(913)661-98-88, buxarova88@mail.ru, https://orcid.org/0000-0002-6093-3721
Natalya V. Nosova, Teaching Assistant at the Department of Obstetrics and Gynecology No. 1, Omsk State Medical University, Ministry of Health of Russia,
644099, Omsk, Russia, Lenin str., 12, +7(951)417-44-52, natalya-nosova-85@mail.ru, https://orcid.org/0000-0002-2362-5367
Vitaly B. Tskhay, MD, PhD, Professor, Head of the Department of Perinatology, Obstetrics and Gynecology, Prof. Voino-Yasenetsky Krasnoyarsk State Medical University, Ministry of Health of Russia, 660022, Russia, Krasnoyarsk, Partizan Zheleznyak str. 1, +7(923)287-21-34, tchai@yandex.ru, https://orcid.org/0000-0003-2228-3884
Yuriy S. Raspopin, PhD, Teaching Assistant at the Department of Anesthesiology and Intensive Care of Institute of Postgraduate Education, Prof. Voino-Yasenetsky Krasnoyarsk State Medical University, Ministry of Health of Russia; Krasnoyarsk Regional Clinical Centre for Maternal and Child Health, 660022, Russia, Krasnoyarsk,
Partizan Zheleznyak str., 1, +7(950)413-87-48, oar24@mail.ru, https://orcid.org/0000-0001-5550-1628
Yuliya G. Garber, Deputy Chief Physician for obstetric and gynecological care, Krasnoyarsk Regional Clinical Center for Maternal and Child Health, 660074, Russia, Krasnoyarsk, Academician Kirensky str., 2A, +7(902)940-28-92, kkkc@pericentr.ru
Igor R. Wecker, PhD, Deputy Chief Physician for obstetric and gynecological care, Orenburg Regional Clinical Hospital No. 2, 460000, Russia, Orenburg, Nevelskaya str., 24, +7(3532)446570, ivekker@rambler.ru
Olga N. Jurlova, Obstetrician-Gynecologist, Head of the Department of Pregnancy Pathology, Orenburg Regional Clinical Hospital No. 2, 460000, Russia, Orenburg, Nevelskaya str., 24, +7(3532)44-65-70, anis1979@mail.ru
Marina V. Nechaeva, PhD, Head of the Reception Department of the obstetric building, Samara Regional Clinical Hospital named after V.D. Seredavin, 443095, Russia, Samara, Tashkentskaya str., 159, +7(846)956-12-15, marinanechaeva2010@mail.ru, https://orcid.org/0000-0001-6468-8199
Tatyana S. Belokoneva, PhD, Head of the Department of Antenatal Fetal Protection and Ultrasound Diagnostics of the obstetric building, Samara Regional Clinical Hospital named after V.D. Seredavin, 443095, Russia, Samara, Tashkentskaya str., 159, +7(846)956-12-15, belokonevats@mail.ru, https://orcid.org/0000-0001-5923-9129
Nataliya V. Protopopova, MD, PhD, Professor, Head of the Department of Obstetrics and Gynecology, Irkutsk State Medical Academy of Postgraduate Education - branch of the Russian Medical Academy of Continuous Professional Education, Ministry of Health of Russia, 664049, Russia, Irkutsk, Yubileyny Ave., 100, +7(3952)46-28-01,
doc_protopopova@mail.ru, https://orcid.org/0000-0002-1740-228X
Victoria N. Dudakova, MD, PhD, Associate Professor of the Department of Obstetrics and Gynecology, Irkutsk State Medical Academy of Postgraduate Education - branch of the Russian Medical Academy of Continuous Professional Education, Ministry of Health of Russia, 664049, Russia, Irkutsk, Yubileyny Ave., 100, +7(3952)46-28-01,
vidun@mail.ru, https://orcid.org/0000-0003-2916-5688
Denis A. Novichkov, PhD, Associate Professor of the Department of Obstetrics and Gynecology of the Pediatric Faculty, Saratov State Medical University named after
V.I. Razumovsky, Ministry of Health of Russia; Chief non-staff obstetrician-gynecologist of the Ministry of Health of Saratov Region, 410012, Russia, Saratov, B. Kazachya str., 112, +7(904)241-34-64, dnovichkov@mail.ru, https://orcid.org/0000-0001-6945-835X
Natalia F. Khvorostukhina, MD, PhD, Professor, Head of the Department of Obstetrics and Gynecology of the Pediatric Faculty, Saratov State Medical University named
after V.I. Razumovsky, Ministry of Health of Russia, 410012, Russia, Saratov, B. Kazachya str., 112, +7(927)277-79-35, Khvorostukhina-NF@yandex.ru,
https://orcid.org/0000-0002-5864-3397
Natalia Yu. Vladimirova, MD, PhD, Deputy Chief Physician for Obstetrics and Gynecology, Perinatal Center named after Professor G.S. Postol, Ministry of Health of the Khabarovsk Territory, 680000, Russia, Khabarovsk, Istomina str., 85, +7(4212)45-40-34, zam.pc@mail.ru, https://orcid.org/0009-0004-1776-7168
Ksenia V. Fedorova, Physician at the Maternity Department, Perinatal Center named after Professor G.S. Postol, Ministry of Health of the Khabarovsk Territory,
680000, Russia, Khabarovsk, Istomina str., 85, +7(4212)45-40-34, zam.pc@mail.ru
Marina P. Rinchindorzhieva, PhD, Head of Department, Republican Perinatal Center, Ministry of Health of the Republic of Buryatia; Chief non-staff specialist in obstetrics of the Ministry of Health of the Republic of Buryatia, 670031, Russia, Buryatia, Ulan-Ude, Pirogova str., 15b, +7(301)237-31-76, marirmp@mail.ru,
https://orcid.org/0000-0003-1153-6057
Bairma B. Tudupova, PhD, Head of the Pregnancy Pathology Department, Republican Perinatal Center, Ministry of Health of the Republic of Buryatia, 670031, Russia, Buryatia, Ulan-Ude, Pirogova str., 15b, +7(301)237-19-76, tudupova.76@mail.ru, https://orcid.org/0009-0000-6444-2471
Tatiana V. Panova, PhD, Obstetrician-Gynecologist, Head of the Regional Perinatal Center of City Clinical Hospital No. 40, 603083, Russia, Nizhny Novgorod,
Smirnov Hero str., 71/5, +7(831)217-63-43, tatvpanova@yandex.ru
Olga I. Guseva, MD, PhD, Professor of the Department of Obstetrics and Gynecology, Privolzhsky Research Medical University, Ministry of Health of Russia,
603005, Russia, Nizhny Novgorod, Minin and Pozharsky sqr., 10/1, +7(831)465-75-75, alisa52@yandex.ru, https://orcid.org/0009-0002-1241-7076
Olga V. Manuilenko, PhD, Chief Physician of City Clinical Hospital No. 40, 603083, Russia, Nizhny Novgorod, Smirnov Hero str., 71/5, +7(831)217-63-43, o-v-man@mail.ru
Olga Yu. Brum, Deputy Chief Physician for Obstetrics and Gynecological Care, Transbaikal Regional Perinatal Center; Chief non-staff specialist in obstetrics and gynecology
of the Ministry of Health of Transbaikal region, 672038, Russia, Chita, Transbaikal region, Kokhansky str., 16, +7(914)457-11-38, ymnenkaya@yandex.ru
Oksana V. Dorfman, Head of the Maternity Department, Transbaikal Regional Perinatal Center, 672038, Russia, Chita, Transbaikal region, Kokhansky str., 16,
+7(924)381-76-92, Oksana-dorfman@yandex.ru
Tatiana A. Verovskaya, Chief non-staff obstetrician-gynecologist at the Health Committee of the Volgograd region; Chief Physician, Volgograd Regional Clinical Perinatal Center No. 2, 400008, Russia, Volgograd, Marshal Vasilevsky str., 70, +7(8442)99-07-18, vokpc2@volganet.ru
Lalita K. Babaeva, Obstetrician-gynecologist, Volgograd Regional Clinical Perinatal Center No. 2, 400008, Russia, Volgograd, Marshal Vasilevsky str., 70, +7(8442)99-07-18, vokpc2@volganet.ru
Alexander N. Rymashevsky, MD, PhD, Professor, Head of the Department of Obstetrics and Gynecology No. 1, Rostov State Medical University, Ministry of Health of Russia, 344022, Russia, Rostov-on-Don, Suvorov str., 119, rymashevskyan@mail.ru, https://orcid.org//0000-0003-3349-6914
Тatyana V. Khvalina, Head of the Department of Pathology of Pregnancy, Rostov Regional Perinatal Center, 344068, Russia, Rostov-on-Don, Bodray str., 90,
super-x-n2012@yandex.ru
Svetlana L. Dmitrieva, PhD, Deputy Chief Physician for obstetric and gynecological care, Kirov Regional Clinical Perinatal Center; obstetrician-gynecologist,
Associate Professor of the Department of Obstetrics and Gynecology, Kirov State Medical University, Ministry of Health of Russia,
610048, Russia, Kirov, Moskovskaya str., 163, +7(909)720-19-99, swdmitr09@yandex.ru, https://orcid.org/0000-0002-2505-0202
Sergey N. Gorev, Head of the Delivery Department, Kirov Regional Clinical Perinatal Center, 610048, Russia, Kirov, Moskovskaya str., 163, +7(964)254-23-89,
gorew.sergei2018@yandex.ru
Anna I. Malyshkina, MD, PhD, Professor, Director of the Ivanovo Research Institute of Motherhood and Childhood named after V.N. Gorodkov, Ministry of Health of Russia, 153045, Russia, Ivanovo, Pobedy str., 20; Head of the Department of Obstetrics and Gynecology, Medical Genetics, Ivanovo State Medical Academy, Ministry of Health
of Russia, 153012, Russia, Ivanovo, Sheremetevsky Ave., 8; Chief non-staff specialist in obstetrics, gynecology and reproductive health of women of the Ministry of Health
of Russia in the Central Federal District of Russia, +7(4932)33-62-63, ivniimid@inbox.ru, https:/orcid.org/0000-0002-1145-0563
Oleg N. Pesikin, PhD, Deputy Director for Medical Work, Head of the Department of Medical and Social Research, Monitoring and Curation, Ivanovo Research Institute
of Motherhood and Childhood named after V.N. Gorodkov, Ministry of Health of Russia, 153045, Russia, Ivanovo, Pobedy str., 20, +7(4932)33-70-13, pesikin@inbox.ru,
https://orcid.org/0000-0002-3666-5309
Vladislav B. Zubenko, Deputy Chief Physician for obstetric and gynecological care, Stavropol Krai Clinical Perinatal Center, 355041 Russia, Stavropol Krai, Stavropol, Lomonosov str., 44, +7(865)223-93-80, zubenkomd@gmail.com
Natalia V. Lobach, Head of the Obstetric Department of Pregnancy Pathology, Stavropol Krai Clinical Perinatal Center, 355041, Russia, Stavropol Krai, Stavropol, Lomonosov str., 44, +7(865)223-93-80, Natasha-lobach@yandex.ru
Tatyana V Briukhacheva, Physician at the Obstetric Department of Pregnancy Pathology, First Republican Clinical Hospital, Perinatal Center, 426039, Russia, Izhevsk,
V. Highway str., 57, +7(904)315-40-57, fildepersovaya1@yandex.ru
Alyona A. Karavaeva, Physician at the Obstetric Department of Pregnancy Pathology, First Republican Clinical Hospital, Perinatal Center, 426039, Russia, Izhevsk,
V. Highway str., 57, +7(912)021-15-18, alenka-kara88@mail.ru
Vitaly F. Bezhenar, MD, PhD, Professor, Head of the Department of Obstetrics, Gynecology and Neonatology/Reproductology, Head of the Clinic of Obstetrics and Gynecology, Pavlov First St. Petersburg State Medical University, Ministry of Health of Russia, 197022, Russia, St. Petersburg, Leo Tolstoy str., 6-8, +7(812)338-78-66,
bez-vitaly@yandex.ru, https://orcid.org/0000-0002-7807-4929
Byuzand V. Arakelyan, MD, PhD, Professor of the Department of Obstetrics, Gynecology and Neonatology, Pavlov First St. Petersburg State Medical University,
Ministry of Health of Russia, 197022, Russia, St. Petersburg, Leo Tolstoy str., 6-8, +7(812)338-78-66, byuzand@mail.ru, https://orcid.org/0000-0002-2868-7997
Anna Yu. Ralnikova, Obstetrician-Gynecologist at the Obstetric Department of Pregnancy Pathology at the Clinic of Obstetrics and Gynecology, Pavlov First
St. Petersburg State Medical University, Ministry of Health of Russia, 197022, Russia, St. Petersburg, Leo Tolstoy str., 6-8, +7(812)338-78-66, anna.ralnikova1510@gmail.com,
https:/orcid.org//0000-0003-1875-4567
Tatyana Yu. Kurleeva, PhD, Chief Physician, Primorsky Regional Perinatal Center, 690011, Russia, Vladivostok, Mozhayskaya str., 1B, +7(423)227-63-79, ktu-pc@perinatalvl.ru
Elizaveta V. Vologodskaya, Head of the Obstetric Department of Pregnancy Pathology, Primorsky Regional Perinatal Center, 690011, Russia, Vladivostok, Mozhayskaya str., 1B, +7(423)227-63-79, vologodskaya@perinatalvl.ru
Lyudmila V. Dikareva, MD, PhD, Professor, Head of the Department Obstetrics and Gynecology of Pediatric Faculty with Postgraduate Education Course, Astrakhan State Medical University, Ministry of Health of Russia, 414000, Russia, Astrakhan, Bakinskaya str., 121, +7(927)661-58-01, dikarevalv@mail.ru,
https://orcid.org/0000-0001-9179-1669
Irina P. Malysheva, Deputy Head of Obstetrics and Gynecology, Regional Perinatal Center, Aleksanrdo-Mariinskaya Regional Clinical Hospital, 414056, Russia, Astrakhan, Тatishcheva str., 2, +7(903)348-98-74, irina.malysheva@ro.ru, https://orcid.org/0009-0002-1878-8644
Azimaa M. Idam-Syuryun, Deputy Chief Physician for Obstetric and Gynecological Care, Perinatal Center of Republic of Tyva, 667011, Russia, Tyva Republic, Kyzyl,
Oyuna Kursedi str., 59A, +7(999)179-85-65, azimaa2012@yandex.ru
Elena Yu. Shakurova, PhD, Deputy Chief Physician, Republic Perinatal Center, 185002, Russia, Petrozavodsk, Syktyvkar str., 9, shakurova@rpc.karelia.ru
Yurii A. Semenov, PhD, Chief Physician, Regional Perinatal Center, 454000, Russia, Chelyabinsk, Vorovskogo str., 70-12, u-sirius@mail.ru
Aleksei V. Sherstobitov, Chief non-staff specialist - obstetrician-gynecologist at the Ministry of Health of Chelyabinsk Region; Deputy Chief Physician of Obstetrics,
Regional Perinatal Center, 454000, Russia, Chelyabinsk, Vorovskogo str., 70-12, Arno1980@yandex.ru
Aleksei Ia. Fortygin, Deputy Chief of Gynecology, Regional Perinatal Center, 454000, Russia, Chelyabinsk, Vorovskogo str., 70-12, Le.fort@mail.ru
Evgenii S. Ziuzin, Head of the Surgery Department, Regional Perinatal Center, 454000, Russia, Chelyabinsk, Vorovskogo str., 70-12, ipselux@gmail.com
Natalya L. Kashlevskaya, Chief non-staff specialist of the Penza region in obstetrics and gynecology; Deputy Chief Physician for obstetric and gynecological care,
Penza Regional Clinical Hospital named after N.N. Burdenko, 440026, Russia, Penza, Lermontov str., 28, +7(937)402-55-25, natela807@mail.ru
Margarita S. Shamina, Obstetrician-Gynecologist at the Department of Pregnancy Pathology, Perinatal Center, Penza Regional Clinical Hospital named after N.N. Burdenko, 440026, Russia, Penza, Lermontov str., 28, +7(961)354-24-77, mar-cergevna@yandex.ru
Tatyana A. Gustovarova, MD, PhD, Professor, Head of the Department of Obstetrics and Gynecology FDPO, Smolensk State Medical University, Ministry of Health of Russia, 214019, Russia, Smolensk, Krupskoj str., 28, +7(910)788-07-13, tanya.prof@yandex.ru
Valeriy А. Khavansky, Obstetrician-Gynecologist, Head of the Maternity Department, Mordovian Republican Central Clinical Hospital, 430013, Russia, Saransk, Pobedy str., 14/5, building 1, +7(834)276-42-99, hva1964@mail.ru
Mikhail E. Shchegolkov, Chief Physician, Lipetsk Regional Perinatal Center, 398050, Russia, Lipetsk, Zegelya str., 6, +7(4742)31-45-96, lopc@zdrav48.ru
Svetlana A. Kulakova, PhD, Obstetrician-Gynecologist, Head of the Labor Department, Perinatal Center, Belgorod Regional Clinical Hospital of St. Joasaph,
308007, Russia, Belgorod, Nekrasova str., 8/9.
Viktoria V. Klishina, Deputy Chief Physician, Obstetrician-Gynecologist, V.Y. Mishekurin Novgorod Regional Clinical Perinatal Center; Chief non-staff specialist in obstetrics and gynecology of the Ministry of Health of Novgorod Region, 173001, Russia, Veliky Novgorod, Tihviskaya str., 9/11, +7(921)699-01-12, 853vvk@gmail.com
Corresponding author: Alexandra A. Mikheeva, shuratora@mail.ru