Tuberculosis, fertility and pregnancy: the clinical and experimental aspects
Kayukova S.I., Ulyumdzhieva V.A., Kulakova E.V., Nikonenko B.V., Fortygina Yu.A., Shchelykalina S.P., Karpina N.L.
The epidemiological situation for tuberculosis in the Russian Federation has improved over the last decade. However, fertility potential and unplanned pregnancy in women in detection and treatment of tuberculosis (TB) of the respiratory organs raise concern.
Objective: To explore the relationship between unplanned pregnancy and the course of TB of the respiratory organs in women and assess the influence of tuberculosis infection on fertility of BALB/c female mice to develop a clinical and experimental concept for a possibility of getting pregnant with favorable perinatal outcomes.
Materials and methods: Observational cross-sectional study was carried out at the Central Research Institute of Tuberculosis. The study included 164 patients, who were divided into 2 groups. Group 1 included 82 pregnant women, who had TB of the respiratory organs. Group 2 included 82 non-pregnant women, who had TB of the repiratory organs. The experimental research was conducted using 40 BALB/c female mice. The mice were divided into 2 groups. Group 1 included 20 pregnant mice infected with Mtb. Group 2 included 20 pregnant mice, but not infected with Mtb.
Results: Active TB disease suppresses the reproductive potential in BALB/c female mice. In women, who have TB of the respiratory organs, unfavorable social and fertility factors increase the risk of unplanned pregnancy by 3.5 times, that aggravates the course of tuberculosis compared with non-pregnant patients. Late relapses occur by 2.5 times more often, exudative pleurisy and bronchial tuberculosis by 1.7 times, late detection of cavernous pulmonary tuberculosis by 5.5 times. The reverse negative impact of TB of the respiratory organs on the course of pregnancy, delivery and the postpartum period was not detected.
Conclusion: The scientifically based interdisciplinary approach to pregnancy management, taking into account unfavorable social and fertility factors in women with TB of the respiratory organs, makes it possible to achieve high efficacy of anti-tuberculosis therapy, to reduce the frequency of obstetric complications, and to have favorable perinatal outcomes.
Authors' contributions: Kayukova S.I., Ulyumdzhieva V.A., Kulakova E.V., Nikonenko B.V., Fortygina Yu.A., Shchelykalina S.P., Karpina N.L. – development of the study design, obtaining data for analysis, review of publications on the topic of the article, analysis of the obtained data, article writing.
Conflicts of interest: The authors confirm that they have no conflict of interest to declare.
Funding: The study was conducted within the framework of the fundamental theme “Tuberculosis and respiratory diseases – modern multimodal diagnosis and rehabilitation in comorbid conditions” at the Center for the diagnosis and rehabilitation of respiratory diseases of the Central Research Institute of Tuberculosis, UN FURE-2022-0013. Reg. No.122041200022-2.
Ethical Approval: The study was approved by Research Ethics Committee of the Central Research Institute of Tuberculosis (protocol No. 11, 2020). The experimental procedures were approved by Animal Care Ethics Committee of the Central Research Institute of Tuberculosis (protocol IACUC No. 8).
Patient Consent for Publication: The patients have signed informed consent for publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available on request from the corresponding author after approval from the principal investigator.
For citation: Kayukova S.I., Ulyumdzhieva V.A., Kulakova E.V., Nikonenko B.V., Fortygina Yu.A., Shchelykalina S.P., Karpina N.L. Tuberculosis, fertility and pregnancy: the clinical and experimental aspects.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2025; (6): 140-148 (in Russian)
https://dx.doi.org/10.18565/aig.2025.91
Keywords
Over the last decade, there is a stable reduction in the tuberculosis (TB) incidence and mortality rates in the Russian Federation. From 2010 to 2019, the TB incidence rate reduced by 1.9 times, that has become one of the best indicators in the world. In 2020, our country reached the values of the indicators for elimination of tuberculosis in the "End TB Strategy" developed by the World Health Organization (WHO). In 2021, the WHO excluded the Russian Federation from the list of countries with a high burden of tuberculosis [1].
In addition, currently there is a demographic crisis in Russia not only due to an increase in mortality rate and decrease in life expectancy, but also due to decline in birth rate. From 2019 to 2023, the negative dynamic in population decline from 146,780 to 146,425 million people, and negative population growth rate from -0.06% to -0.37% is registered in our country [2].
Severe systemic inflammation, including tuberculosis have a negative impact on reproductive health [3, 4]. In women with TB of the respiratory organs, fertility potential decreases and hinders the chance of having a normal pregnancy and healthy offspring in future [5–7]. An unplanned but desired pregnancy at the time of detection and treatment of TB of the respiratory organs is a complex issue. A combination of tuberculosis and pregnancy can initiate the relapses of TB of the respiratory organs. In dispensary observation, two types of relapses are being found: early relapse in patients who have been cured of tuberculosis and classified as patients with Class 3 TB (clinical cure); late relapse in patients who previously had tuberculosis and were removed from dispensary observation due to recovery [8].
It is believed that tuberculosis potentiates adverse outcomes for a mother and fetus. However, a number of researchers consider motherhood as a priority and recommend that anti-tuberculosis treatment should be withheld until 12 weeks of gestation, thereby postponing treatment until the second and third trimesters of pregnancy [10, 11].
In view of the above, the purpose of the study was to explore the relationship between unplanned pregnancy and the course of TB of the respiratory organs in women and assess the influence of tuberculosis infection on fertility of female BALB/c mice to develop a clinical and experimental concept for a possibility of getting pregnant with favorable perinatal outcomes.
Material and methods
The study was carried out in two stages (clinical and experimental) at the Central Research Institute of Tuberculosis. In accordance with the purpose and design of the clinical observational, cross-sectional study, as well as inclusion and non-inclusion criteria, the patients, who underwent treatment at the Central Scientific Research Institute of Tuberculosis from 2010–2021 were included in the study. The patients were divided into 2 groups. Group 1 included 82 pregnant women, who had TB of the respiratory organs. Group 2 included 82 non-pregnant women, who had TB of the repiratory organs.
The study was approved by Research Ethics Committee of the Central Research Institute of Tuberculosis (protocol No. 11, 2020). The design of the study was developed in accordance with international recommendations on STrengthening the Reporting of OBservational studies in Epidemiology (STROBE). Inclusion criteria for both groups were the following: comparable reproductive age and clinical forms of TB of the repiratory organs. Non-inclusion criteria for both groups were the presence of oncological, psychiatric disorders, HIV infection.
All patients underwent standard phthisiological, obstetric and gynecological examination: data collection of life and medical history, clinical and laboratory blood tests, comprehensive microbiological and molecular genetic testing of diagnostic material, and X-ray tomography (when indicated, after 12 weeks of pregnancy). When TB of the repiratory organs was diagnosed during pregnancy and in the postpartum period, the medical commission meeting was held to assign chemotherapy regimen in accordance with drug sensitivity of the pathogenic bacteria and the individual tolerance of the patients. The observation period lasted from the onset of pregnancy up to 1 year after giving birth.
The experimental stage of the study was conducted using 40 female BALB/c mice weighing 20–22 g, aged 8 weeks. The mice were bred according to the guidelines No. 755 of the Ministry of Health of Russia – INH Office of Laboratory Animal Welfare (OLAW). The experimental procedures were approved by Animal Care Ethics Committee of the Central Research Institute of Tuberculosis (IACUC protocol No. 8). The laboratory animals were selected in the study groups in accordance with Good Laboratory Practice (GLP) approved by National Standards of the Russian Federation of March 01, 2010. GOST 33044-2014.
Female BALB/c mice (n=40) were divided into 2 groups. Group 1 included pregnant mice infected with Mycobacterium tuberculosis (n=20). Group 2 included pregnant mice, not infected with Mycobacterium tuberculosis (n=20).
The experimental research consisted of 4 steps. Step 1: female BALB/c female mice in group 1 (n=20) were infected with the culture of Mycobacterium tuberculosis of virulent strain H37Rv in the Glas-Col chamber (USA). Step 2: 28 days after female BALB/c mice in groups 1 and 2 were infected, they were crossed with male mice of the same inbred strain (n=40). Step 3: Within 15 days after crossing, pregnancies were determined by the presence of the vaginal plugs. The estimated date of conception and identification numbers of mice were entered into the study protocol. Step 4: observation of offspring in female BALB/c 1-й mice in groups 1 and 2 after parturition (n=40). Duration of the experimental research was 63 (60; 67) days.
Statistical analysis
Statistical analysis of the clinical and experimental data was performed using R scripts v. 3.5 in R Studio. The descriptive statistics for the qualitative variables are represented as absolute (n) and relative (%) values. The median (Me) was chosen as a measure of central tendency for quantitative characteristics, and the upper (Q3) and lower (Q1) quartiles were chosen as interval estimates. The results are represented as Me (Q1; Q3).
The significance of intergroup differences in quantitative variables in independent samples was assessed using the Mann–Whitney U-test for unrelated populations. The qualitative variables were assessed using Fisher’s exact test. The chi-square test was used to compare the observed and expected (equal) frequencies in one group.
The scientific hypothesis was formed based on the following explored variables: social and fertility factors in history (lack of permanent employment and financial instability, irresponsible reproductive behavior, such as unprotected sexual activity), and the severity of the course of TB of the respiratory organs in pregnant and non-pregnant patients (a high rate of late relapses, complications, such as exudative pleurisy and bronchial tuberculosis, formation of cavities in lung tissue). The explored quantitative variables were the following: patient’s age and age at menarche, menstrual cycle and period length, newborn’s body weight and length, duration of the experimental research, gestation length at parturition, the quantity of mouse pups. The data related to all parameters were collected. Missing values were minimal. Imputation technique for missing values was not used.
The likelihood of systematic errors was reduced by carefully monitoring the compliance of inclusion and non-inclusion criteria in data collection and assessment of the between-group comparability by age and clinical forms of TB of the respiratory organs.
The differences were considered to be statistically significant at р<0.05. The odds ratio (OR) with 95% confidence interval (92% CI) was used to assess the influencing factors.
Results
Results of the clinical study
In both studied groups, the women of reproductive age prevailed – 78/82 (95%) and 70/82 (85%) years; the median age was 29.4 (18; 41) and 30.5 (19; 43) years.
Prevalence of social and fertility factors was statistically significant in women in group 1 compared with group 2: lack of permanent employment – 52/82 (63%) and 38/82 (46%) women (р=0.041, OR=2.0 [95% CI 1.1–3.7]), and irresponsible reproductive behavior (contraception refusal) – 59/82 (72%) and 16/82 (20%) women (р<0.001, OR=10.6 [95% CI 5.1–21.9]). In addition, most patients in group 1 did not undergo prophylactic dispensary examination including chest fluorography chest over the last 2–5 years – 49/82 (60%) and 40/82 (49%) women, respectively. There was no statistically significant difference between the groups.
The characteristics of menstrual function in women in the studied groups were analyzed. The values for indicators in groups 1 and 2 were comparable: age at menarche – 13 (12.3; 14) and 13 (12; 13) years; menstrual cycle length – 28 (28; 30) and 28 (28; 29) days, and period length – 5 (5; 6) и 5 (5; 5.6) days, respectively. In both groups, menstruation was predominantly characterized as moderate in 74/82 (90%) and 77/82 (94%) women, and painless in 69/82 (84%) and 69/82 (84%) women.
The burdened gynecological history was more often in women in group 1 compared with group 2 – 44/82 (54%) and 31/82 (38%), respectively, with no statistically significant difference between the groups. However, cervical pathology in women in group 1 was significantly more often compared with women in group 2 – 29/44 (66%) and 13/31 (42%), respectively (р=0.035).
Pregnancies in history were significantly more often in patients in group1 versus group 2 – 81/82 (99%) and 43/82 (52%), respectively (р<0.001, OR=73.5 [95% CI 9.8–553.3]). Previous pregnancies ended in birth more often – 75/81 (93%) and 41/43 (95%), medical abortions were in 20/81 (25%) and 15/43 (35%) women. Spontaneous abortion frequency in history was higher in patients in group 1 compared with group 2 – 11/81 (14%) and 2/43 (5%), but the difference was not statistically significant (р=0.216). At the same, no fetal death, stillbirth and intrauterine fetal abnormalities were registered in medical history of women in both groups.
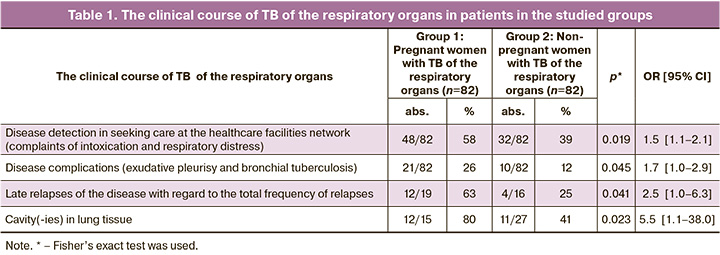
We identified the following features of the course of TB of the respiratory organs combined with pregnancy in women in group 1 compared with group 2: high frequency of late relapses – in 12/19 (63%) and 4/16 (25%) women (р=0.041); detection of TB of the respiratory organs in seeking care at the healthcare facilities network regarding complaints of intoxication and respiratory distress in 48/82 (58%) and 32/82 (39%) women (р<0.019); high frequency of complications of the TB of the respiratory organs – exudative pleurisy and bronchial tuberculosis in 21/82 (26%) and 10/82 (12%) women (р=0.045), as well as formation of cavities in lung tissue in 12/15 (80%) and 11/27 (41%) women, respectively (р=0.023) (Table 1) .
TB of the respiratory organs was found most often in the postpartum period in women in group 1 – 57/82 (70%), and less often during pregnancy 25/82 (30%) (р<0.001). According to “The clinical guidelines for the diagnosis and treatment of tuberculosis of the respiratory organs” of the Russian Society of Phthisiatricians (2014, 2015) [12, 13], anti-tuberculosis therapy was used in 57/57 (100%) in the postpartum period, in 5/25 (20%) women during pregnancy (after 12 weeks of pregnancy), and in 20/25 (80%) women after termination of pregnancy.
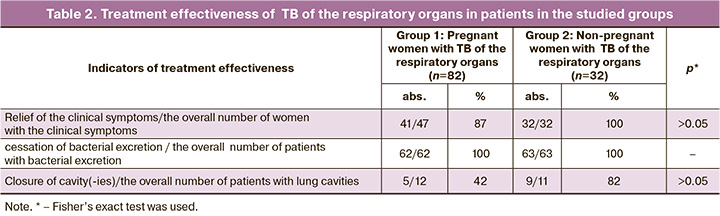
Anti-tuberculosis therapy was effective in both groups and resulted in relief of the clinical symptoms (intoxication and bronchopulmonary syndromes) and cessation of bacterial excretion. Frequency of closure of cavity(-ies) in group 2 was higher compared with group 1. However, the differences were not statistically significant (Table 2).
Current pregnancies occurred spontaneously, without using assisted reproductive technology in all women in group 1. Unplanned pregnancies were in 61/82 (74%) patients in group 1. At the same time, there was no significant difference in the frequency of unplanned pregnancies in the subgroups with primarily detected TB of the respiratory organs and with disease relapses (p=0.132) – 44 (70%) and 17 (90%), respectively. The presence of at least one of social and fertility factors (lack of permanent employment, financial instability, irresponsible reproductive behavior, such as unprotected sexual activity) increased the risk of unplanned pregnancy versus non-pregnancy and planned pregnancy by 3.5 times (95% CI 1.5–8.3].
Two patients in group 1 were not recommended to get pregnant due to multi-drug resistant fibrous-cavernous pulmonary tuberculosis and multi-stage surgical treatment for TB in history [14], as well as relapse of infiltrative pulmonary tuberculosis in the phase of seeding combined with multi-drug resistance of the pathogen. However, the women in both groups ignored recommendations of the phthisiatrician. They got pregnant and underwent follow-up at the women’s clinic and tuberculosis dispensary at the place of residence, and were consulted for hemotherapy regimen and disease management at the Central Research Institute of Tuberculosis. In both cases, women gave birth to full term healthy infants at regional perinatal centers. Breastfeeding was prohibited. The women received the full-fledged anti-tuberculosis treatment, and there were no relapses of TB of the respiratory organs within 1 year after childbirth.
Pregnancy outcomes in women in group 1 were assessed. Current pregnancies ended with birth significantly more often – 62/82 (75%), less often with medical abortion 16/82 (20%) (р<0.001), and spontaneous abortion – 4/82 (5%) (р<0.001). In all cases, medical abortion was performed upon the woman’s request. Spontaneous abortion occurred before 8 weeks of pregnancy in 3 (75%) women and at 17 weeks of pregnancy in 1 woman (25%).
All patients in group 1 who continued their pregnancies, underwent genetic and ultrasound screening at 11–13 and 16–18 weeks. No cases of fetal abnormalities were found. The frequency of obstetric complications during pregnancy in women in group 1 was 19/62 (31%). At the same time, there were no statistically significant differences in the frequency of obstetric complications in the first, second and third trimesters – 5/62 (8.1%), 7/62 (11.3%) and 7/62 (11.3%), respectively.
Early toxicosis in the first trimester of pregnancy was in 4/62 (6.5%) patients with TB of the respiratory organs.
One of the major obstetric complications that pose risk for fetal well-being are threatened miscarriage and preterm birth. However, statistically significant difference in the prevalence of these complications was not found in the first, second and third trimesters of pregnancy – 1/62 (1.6%), 3/62 (4.8%) and 3/62 (4.8%), respectively (р>0.05).
Pregnancy complications were the following: placental insufficiency in the third trimester – in 1/62 (1.6%) woman with TB of the respiratory organs; chronic intrauterine hypoxia – in 3/62 (4.8%). Specialized medical care was timely and effectively provided for these women (Table 3).
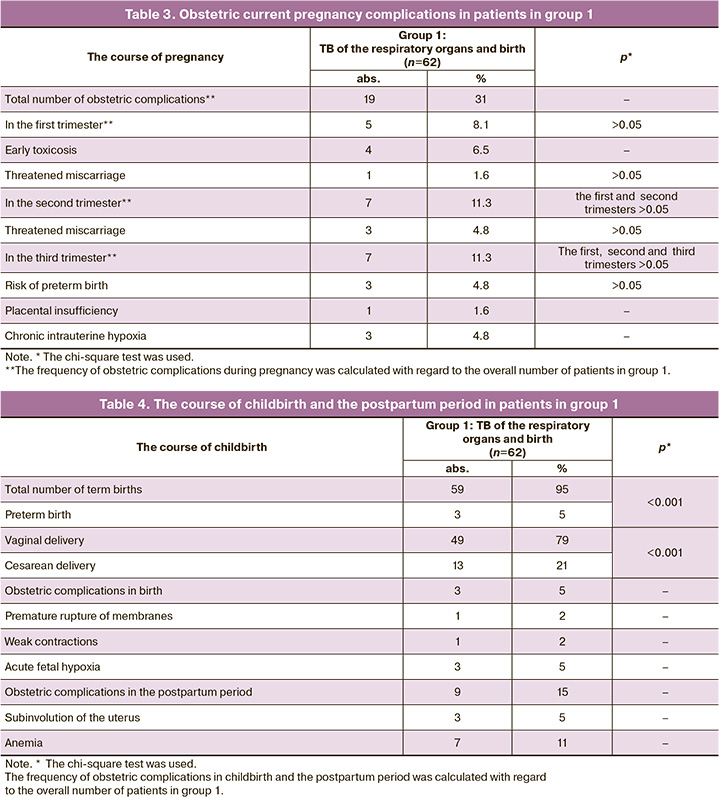
We analyzed the features of the course of childbirth and the postpartum period in women with TB of the respiratory organs. Term births were in the vast majority of patients with TB of the respiratory organs – 59/62 (95%). Preterm births were in 3/62 (5%) women, respectively (р<0.001). At the same time, vaginal delivery was significantly more often versus cesarean delivery – in 49/62 (79%) and 13/62 (21%) women, respectively (р<0.001).
Analysis showed low frequency of obstetric complications in childbirth and the postpartum period – 3/62 (5%) and 9/62 (15%), respectively. At the same time, premature rupture of membranes was in 1/62 (2%), weak contractions were in 1/62 (2%), and acute fetal hypoxia was in 3/62 (5%) cases. In the postpartum period, subinvolution of the uterus was in 3/62 (5%) and anemia in 7/62 (11%) women (Table 4).
All women gave birth to liveborn babies – 62/62 (100%). The median weight of newborns was 3284.5 (2900; 4100) g, body length was 51.5 (45.0; 56.0) cm. The Apgar score was 8 (7; 9) at 5 minutes after birth. The vast majority of newborns were physiologically normal babies – 59/62 (95%) (р<0,001). Pathology was found in 3/62 (5%) newborns: intrauterine pneumonia of viral etiology was in 1/3 (33%) and perinatal encephalopathy in 2/3 (67%) infants. Fetal hypotrophy was registered at preterm birth in 1/62 (2%) case. The Bacillus Calmette–Guérin (BCG) vaccine was administered to 61/62 (98%) newborns (р<0.001); in 1 case vaccination was postponed due to fetal hypotrophy.
Breastfeeding was allowed to 51/62 (82%) women in group 1 (р<0.001). At the same time, in 6/51 (12%) patients, who were allowed breastfeeding, TB of the respiratory organs was detected during pregnancy. For this reason, 1/6 (17%) patient received anti-tuberculosis therapy, and 5/6 (83%) patients did not receive it. However, after childbirth, all these women – 6/6 (100%) discontinued treatment with anti-TB drugs, and due to this fact, there were no contraindications for breastfeeding. According to the data obtained by computed tomography of the chest, no active TB of the respiratory organs was found.
Breastfeeding was not allowed to 11/62 (18%) puerperant women in group 1. Among them, TB of the respiratory organs was found during pregnancy in 6/11 (55%) patients, and 4/6 (67%) patients received anti-tuberculosis therapy both during pregnancy and after childbirth; 2/6 (33%) women did not receive anti-tuberculosis therapy during pregnancy due to their refusal, therefore, the course of anti-tuberculosis therapy was started after childbirth. There were no data on the newborn’s health status after discharge from maternity hospital (Table 5).

The results of the experimental research
We analyzed the impact of tuberculosis on the reproductive function in female BALB/c mice infected with aerosolized Mycobacterium tuberculosis (Mtb). Thirty days after airborne infection with Mtb, female mice in groups 1 and 2 were crossed with healthy, uninfected male mice of the same genetic line.
After crossing the time interval – the number of days from crossing to parturition in female mice – in both groups was calculated. In female BALB/c mice infected with Mycobacterium tuberculosis parturition occurred 29 (22; 38) days after crossing, while in intact mice parturition occurred 24 (21; 34) days after crossing (p≤0.03). The number of baby mice born from each mouse in both groups was calculated. It was found that litter size was significantly smaller in female mice infected with Mycobacterium tuberculosis (group 1) compared with intact female mice (group 2) – 3 (2; 3) (maximum 4) pups, and 4 (4;5) (maximum 9) pups, respectively (p ≤0/001).
Thus, in female BALB/c mice infected with Mycobacterium tuberculosis, pregnancy and parturition occurred later that in intact mice, and litter size (the number of baby mice) was significantly small.
Discussion
The issues of diagnosis and treatment of tuberculosis during pregnancy and breastfeeding continue to be one of the most difficult in phthisiology, obstetrics and gynecology, and neonatology.
It is a generally accepted view that severe and widespread forms of tuberculosis (disseminated, generalized) have a significant negative impact on reproductive potential. Due to this fact, the frequency of spontaneous pregnancies in women with tuberculosis can be quite low [3, 4, 6].
On the one hand, our experimental research confirms this hypothesis, since infection with aerosolized Mycobacterium tuberculosis and subsequent pulmonary tuberculosis showed reduced fertility and litter size in female BALB/c mice. On the other hand, reproductive potential was not fully lost, and generalized forms of tuberculosis were not found in female BALB/c mice with reduced fertility. Comparison of the clinical and experimental data confirms that a number of other factors have impact on realization of reproductive function in women.
It was found that in the presence of adverse fertility factors, such as irresponsible reproductive behavior, contraception refusal, the risk of unplanned pregnancy increases by 3.5 times [95% CI 1.5–8.3]. A combination of adverse social factors, such as absence of permanent employment and stable financial income, as well as not undergoing regular dispensary examination including chest fluorography over the last 2–5 years leads to late and untimely diagnosis of the tuberculosis of the respiratory organs. For this reason, there is a high rate of complications among these women, such as exudative pleurisy and bronchial tuberculosis – 1.5 times higher [95% CI 1.1–2.1] (р=0.019), late relapse of pulmonary tuberculosis – 2.5 time higher [95% CI 1.0–6.3], severe clinical forms of tuberculosis of the respiratory organs at the stage of formation of cavities in lung tissue 5.5 times higher [95% CI 1.1–38.0] compared with non-pregnant patients.
In addition, it can be difficult to diagnose tuberculosis of the respiratory organs in the second and third trimesters of pregnancy by reason of the so-called “period of apparent well-being” due to an increase in size of the uterus, reduction in diaphragmatic excursion, and changes in the ratio between pressure in the chest and the abdominal cavity in the second half of pregnancy. Lung tissue is in the resting state, that creates the conditions for improving the patient's well-being [10, 11].
The reverse negative impact of tuberculosis of the respiratory organs on the course of pregnancy, childbirth and the postpartum period was not found. Although, the study by Pop L.G. et al. (2021) showed that tuberculosis significantly aggravates the course of pregnancy in the first trimester causing severe and frequent early toxicosis with manifestation of the clinical symptoms, such as nausea, vomiting, salivation, dizziness, headaches, general weakness, emotional lability [10]. However, in our clinical research, there was low incidence of early toxicosis among the patients in group 1 in the first trimester of pregnancy.
It is known that active tuberculosis disease can lead to miscarriage and preterm birth due to its toxic effects [11]. In our study, there was low incidence of threatened miscarriage and preterm birth in women with tuberculosis of the respiratory organs.
The following outcomes of the current unplanned pregnancies were significantly more often: term births – 62/82 (75%), absence of fetal abnormalities, low incidence of obstetric complications in childbirth and the postpartum period – 3/62 (5%) and 9/62 (15%), respectively, and favorable pregnancy outcomes.
The results obtained in our clinical and experimental research showed that a combination of social and fertility factors, which can contribute to unplanned pregnancy and complicated course of tuberculosis of the respiratory organs, have a significant negative impact, as well as become an obstacle for safe motherhood. At the same time, the risk of severe obstetric complications due to tuberculosis is exaggerated, and their treatment and prevention require a personalized approach in each clinical situation.
Conclusion
The scientifically based interdisciplinary approach to pregnancy management, taking into account unfavorable social and fertility factors in women with TB of the respiratory organs, makes it possible to achieve high efficacy of anti-tuberculosis therapy, to reduce the frequency of obstetric complications, and to have favorable perinatal outcomes.
References
- https://minzdrav.gov.ru/news/2022/03/24/18525-ministr-zdravoohraneniya-rf-mihail-murashko-zabolevaemost-tuberkulezom-v-rf-uderzhivaetsya-na-istoricheskom-minimume
- Салтыкова Ю.А., Курганская О.В. Демографические проблемы новой реальности России. Социология. 2023; 3: 101-8. [Saltykova Yu.A., Kurganskaya O.V. Demographic problems of Russia’s new reality. Sociology. 2023; (3): 101-8. (in Russian)].
- Клинышкова Т.В., Яковлева А.А. Женское бесплодие, ассоциированное с генитальным туберкулезом. Акушерство, гинекология и репродукция. 2018; 12(1): 74-85. [Klinyshkova T.V., Yakovleva A.A. Female infertility associated with genital tuberculosis. Obstetrics, gynecology and reproduction. 2018; 12(1): 74-85 (in Russian)]. https://dx.doi.org/10.17749/2313-7347.2018.12.1.074-085
- Гопоняко С.В. Туберкулез у женщин репродуктивного возраста. Проблемы здоровья и экологии. 2022; 19(1): 5-12. [Goponiako S.V. Tuberculosis in women of reproductive age. Health and Ecology Issues. 2022; 19(1): 5-12 (in Russian)]. https://dx.doi.org/10.51523/2708-6011.2022-19-1-01
- Tjahyadi D., Ropii B., Tjandraprawira K.D., Parwati I., Djuwantono T., Permadi W. et al. Female genital tuberculosis: clinical presentation, current diagnosis, and treatment. Infect. Dis. Obstet. Gynecol. 2022; 2022: 3548190. https://dx.doi.org/10.1155/2022/3548190
- Datta A., Gupta P., Bhattacharya B., Das A., Chatterjee S., Banerjee A. Evidence of sexual transfer of mycobacteria from male to female partners reporting to an IVF clinic. Trop. Doct. 2022; 52(2): 331-4. https://dx.doi.org/10.1177/00494755221074754
- Dahiya B., Kamra E., Alam D., Chauhan M., Mehta P.K. Insight into diagnosis of female genital tuberculosis. Expert Rev. Mol. Diagn. 2022; 22(6): 625-42. https://dx.doi.org/10.1080/14737159.2022.2016395
- Приказ Минздрава РФ от 21.03. 2003 г. №109 «О совершенствовании противотуберкулезных мероприятий в Российской Федерации». Доступно по: https://www.zakonprost.ru/content/base/156192 [Order of the Ministry of Health of the Russian Federation dated 21.03. 2003 No. 109 "On improving anti-tuberculosis measures in the Russian Federation". Available at: https://www.zakonprost.ru/content/base/156192 (in Russian)].
- Alene K.A., Jegnie A., Adane A.A. Multidrug-resistant tuberculosis during pregnancy and adverse birth outcomes: a systematic review and meta-analysis. BJOG. 2021; 128(7): 1125-33. https://dx.doi.org/10.1111/1471-0528.16573.
- Pop L.G., Bacalbasa N., Suciu I.D., Ionescu P., Toader O.D. Tuberculosis in pregnancy. J. Med. Life. 2021; 14(2): 165-9. doi: 10.25122/jml-2021-0001
- Mathad J.S., Yadav S., Vaidyanathan A., Gupta A., LaCourse S.M. Tuberculosis Infection in pregnant people: current practices and research priorities. Pathogens. 2022; 11(12): 1481. https://dx.doi.org/10.3390/pathogens11121481
- Российское общество фтизиатров. Федеральные клинические рекомендации по диагностике и лечению туберкулеза органов дыхания. М.; 2014. 43с. [Russian Society of Phthisiatricians. Federal clinical guidelines for the diagnosis and treatment of tuberculosis of the respiratory organs. Moscow; 2014. 43p. (in Russian)].
- Российское общество фтизиатров. Федеральные клинические рекомендации по диагностике и лечению туберкулеза органов дыхания с множественной и широкой лекарственной устойчивостью возбудителя. Издание третье. М.; 2015. 35с. [Russian Society of Phthisiatricians. Federal clinical guidelines for the diagnosis and treatment of multidrug-resistant and extensively drug-resistant tuberculosis of the respiratory organs. 3rd ed. Moscow; 2015. 35p. (in Russian)].
- Каюкова С.И., Комиссарова О.Г., Карпина Н.Л., Романов В.В., Уварова Е.В., Лимарова И.В. Ведение беременности, родов и послеродового периода у пациентки с лекарственно-устойчивым, деструктивным туберкулезом легких после этапного хирургического лечения. Туберкулез и болезни легких. 2018; 96(6): 58-63. [Kayukova S.I., Komissarova O.G., Karpina N.L., Romanov V.V., Uvarova E.V., Limarova I.V. Management of pregnancy, delivery and post-natal period in the patient with drug resistant destructive pulmonary tuberculosis after several surgeries. Tuberculosis and Lung Diseases. 2018; 96(6): 58-63. (in Russian)]. https://dx.doi.org/10.21292/2075-1230-2018-96-6-58-63
Received 03.04.2025
Accepted 27.05.2025
About the Authors
Svetlana I. Kayukova, Dr. Med. Sci., obstetrician-gynecologist at the Center for diagnostics and rehabilitation of respiratory diseases, Central Research Institute of Tuberculosis; Professor at the Department of Phthisiology, N.I. Pirogov Russian National Research Medical University, Ministry of Health od Russia, 117513, Russia, Moscow, Ostrovityanov str., 1, +7(915)396-85-34, kajukovalnp@gmail.com, https://orcid.org/0000-0002-5233-3515Valentina A. Ulyumdzhieva, PhD student, Central Research Institute of Tuberculosis, 107564, Russia, Moscow, Yauzskaya alley, 2, +7(937)196-92-22, amulek@bk.ru,
https://orcid.org/0009-0005-8037-249Х
Elena V. Kulakova, PhD, Senior Researcher at the Prof. B.V. Leonov Department of IVF, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia, 117997, Russia, Moscow, Ac. Oparin str., 4, +7(985)769-53-57, e_kulakova@oparina4.ru,
https://orcid.org/0000-0002-4433-4163
Boris V. Nikonenko, Leading Researcher at the Department of Immunology, Central Research Institute of Tuberculosis, 107564, Russia, Moscow, Yauzskaya alley, 2, +7(985)951-95-78, boris.nikonenko52@gmail.com, https://orcid.org/0000-0003-3205-8197
Yulia A. Fortygina, PhD student, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia, 117997, Russia, Moscow, Ac. Oparin str., 4, +7(950)727-07-45, yu_fortygina@oparina4.ru, https://orcid.org/0000-0002-1251-0505
Svetlana P. Shchelykalina, PhD, Associate Professor at the Department of Medical Cybernetics and Computer Science named after S.A. Gasparyan MBF, Pirogov Russian National Research Medical University, Ministry of Health of Russia, 117513, Russia, Moscow, Ostrovityanov str., 1, +7(905)771-46-48, svetlanath@inbox.ru,
https://orcid.org/0000-0003-3292-8949
Natalya L. Karpina, Deputy Director for Science, Central Research Institute of Tuberculosis, 107564, Russia, Moscow, Yauzskaya alley, 2, +7(916)097-36-96,
natalya-karpina@rambler.ru, https://orcid.org/0000-0001-7800-8158
Corresponding author: Svetlana I. Kayukova, kajukovalnp@gmail.com



