Characteristics of reproductive function in women with the recurrent depressive disorder
Objective. To investigate the relationship between reproductive function (RF) and the recurrent depressive disorder (RDD) in women.Ivanets N.N., Tyuvina N.A., Voronina E.O., Balabanova V.V.
Material and methods. The study comprised 120 women with RDD and 120 mentally healthy women aged 18–65 years.
Results. The findings included quantitative characteristics of RF in women with RDD and healthy women. RDD was associated with a later onset and irregularity of menstruation, earlier recovery of menstrual function after childbirth, the occurrence of PMS and premenopause, which leads to a decrease in the number of pregnancies, births, and children. Depression impaired social and family adaptation. Depressions occurring in puberty and postmenopause had the most and the least harmful effect on RF, respectively.
Conclusion. Depressive disorders are associated with periods of hormonal adjustment. Depressive symptoms in PMS may help predict depression in the future or indicate incomplete remission. Women with RDD had impaired menstrual function and decreased childbearing potential.
Keywords
Depression is one of the most common illnesses worldwide. Women comprise 72% of all patients with depressive disorders [1]. For many years, women’s predisposition to depression has been attributed to the action of ovarian hormones [2-11].
There are a relationship and interaction of a woman’s mental state and menstrual function. On the one hand, cyclic changes in the hormonal profile caused by neuroendocrine regulation contribute to mood fluctuations associated with the menstrual cycle, and on the other hand, the biological mechanisms of depressive disorders affect menstrual function [12].
At the same time, a number of long-term studies showed a lack of association between mental changes and the level of female sex hormones [13, 14], in particular between estradiol and FSH and depression [15, 16], as well as between the menstrual cycle phases and mood in women with premenstrual syndrome (PMS) [16]. Also, recent research has not confirmed the assumption that women with premenstrual stress disorder have elevated concentrations of steroids [13, 17]. Thus, mood fluctuations do not seem to be a product of abnormal hormonal levels; instead, they quite likely reflect individual changes in hormonal parameters [18]. Although depressive disorders in women occur during periods of significant hormonal changes (puberty, PMS, pregnancy and the postpartum period, perimenopause) [3, 6–10], mood fluctuations may be caused not by the direct influence of sex hormones, but by the regulating effect of stress-controlling hormones including adrenal hormones [19, 20].
There is a current debate about the role of psychosocial factors in triggering effects of neuro-hormonal adjustment on the genetic predisposition to depression [12, 16].
Although research about the role of menstrual dysfunction in depression and menstrual psychosis dates back to the studies by E. Krepelin (1898) and R. Kraft-Ebing (1897), this topic has not received sufficient coverage over the past few decades. In girls with mood swings, menarche occurs later (15-17 years) than in the general population, and menstruation may be irregular from the very beginning. In severe depression, menstruation may disappear for the entire period of the depressive episode [1]. The prevalence of PMS, which constitutes 30–70% in the general population, is estimated to range from 70 to 100% among women with mental illnesses, specifically among women with manic-depressive psychosis (86%) [21]. However, there is currently no research available exploring individual quantitative indicators of menstrual and reproductive functions, compared with the population of mentally healthy women, while this has not only medical but also of major social implications.
This study aimed to investigate the relationship between reproductive function and the recurrent depressive disorder in women.
Material and methods
The study was conducted from 2014 to 2017at the hospital and outpatient clinic of the S.S. Korsakov Clinic of Psychiatry, I.M. Sechenov First MSMU and comprised 120 women aged from 18 to 65 years, who had a recurrent depressive disorder (RDD) (ICD-10 Code F33.0). The study did not include women with the first or a single episode of depression, pregnant women, and those having decompensated somatic and neurological diseases. For the study, a special survey questionnaire was developed, which included items on the clinical characteristics of the underlying disease (RDD), as well as indicators of menstrual and reproductive function. The Montgomery-Asberg Depression Rating Scale (MADRS) was used to measure the severity of depressive episodes in patients.
The age of patients in the study group was 45.0 [32.5; 54.0] years (min.-max. 18 - 65 years). The disease duration in the study group was 8.0 [4.0, 16.0] years. The number of depressive episodes was 4.0 [3.0; 6.0]. The maximum and minimum duration of depressive episodes was 5.0 [4.0, 7.0] and 2.0 [2.0; 3.0] months, respectively. The median duration of episodes was 3.5 [2.5; 5.0] months. The maximum and minimum duration of remission in the study group was 54.0 [48.0; 84.0] and 6.0 [6.0; 12.0] months, respectively, and median was 33.0 [24.0; 45.0] months. The severity score of depression was 27.0 [26.0; 28.0] on the MADRS scale.
One hundred and twenty mentally healthy women aged from 18 to 65 years comprised a control group. The median age of healthy women in the control group was 42.5 [36.0; 52.0] years.
Statistical analysis was performed using Statistica for Windows 6.0 (StatSoft Inc.). Qualitative variables were described using absolute and relative (%) indicators. The normality of the distribution was tested by the Kolmogorov-Smirnov test
Since most of the quantitative variables were not normally distributed, they were described using the median (Me), and quartiles (Me [25%; 75%]) and non-parametric tests were used to assess the statistical significance of differences between groups. Kruskal–Wallis test was used for comparing numerical data between three groups, and Mann–Whitney U-test for comparing two groups. Categorical variables were compared using the Chi-square test and the two-sided Fisher’s exact test, if necessary.
The critical level of significance was considered at p <0.05. Bonferroni correction was applied for multiple comparisons; in this case, p was defined as p = 0.05/n, where n is the number of pairwise comparisons.
Results and discussion
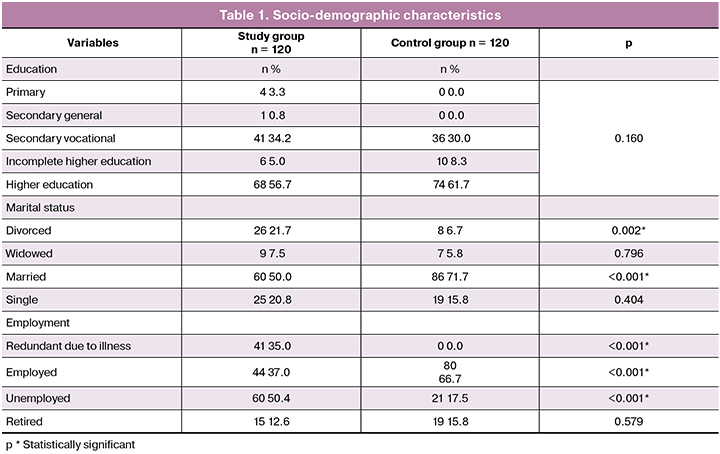
A comparative analysis of socio-demographic indicators showed that women with depression were less adapted to family and social life (Table 1).
A number of indicators of menstrual and reproductive function were significantly different between the groups (Tables 2, 3).
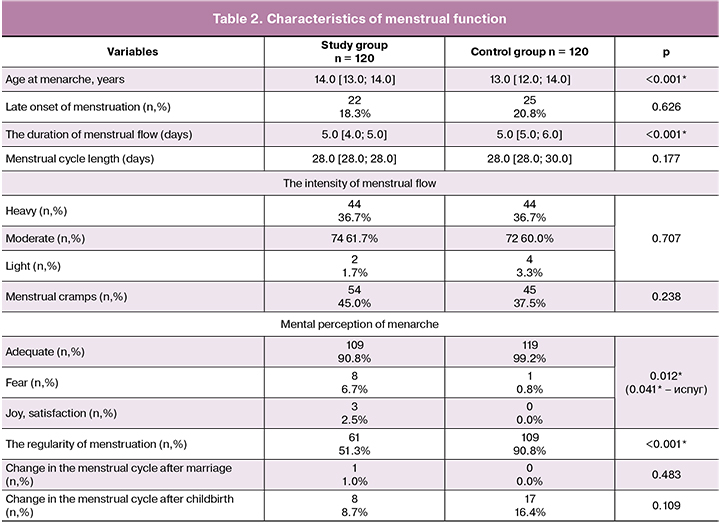
In patients with RDD, the first menstruation occurred significantly later, and the duration of menstrual flow was shorter than in healthy women. Healthy women had a significantly more regular menstrual cycle. The timing of the onset of regular menstruation (established immediately or later), menstrual cycle length, frequency of menstrual cramps and intensity of menstrual flow did not differ significantly. Patients with RDD and healthy women had a different mental perception of the first menstruation, indicating the readiness of the woman’s body to perform the childbearing function. In women with depressive disorders, the onset of menstruation was significantly more likely to cause a polar emotional reaction in the form of fear, panic, or, conversely, joy and delight, unlike healthy ones. In the period of depression, menstruation became irregular or even disappeared completely for a period of a severe depressive episode. These facts support the assumption that the normal menstrual cycle is an indicator of a woman’s physical and mental health.
The groups had significant differences in terms of regularity and satisfaction with sex life (p <0.001). While 78.0% and 70.3% of healthy women had a regular sex life and were satisfied with it, respectively, while among women with RDD only 49.6% had a regular sex life, and 37.8% were satisfied with it.
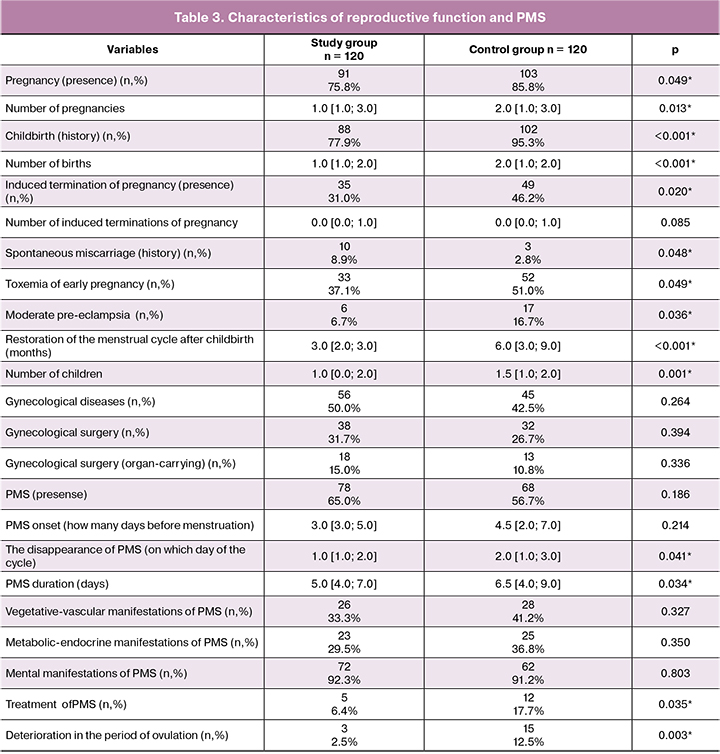
Patients with RDD and healthy women differed significantly in some fertility indicators such as presence and number of pregnancies and deliveries; the average number of children per woman was greater among healthy women. On the other hand, women with RDD were more likely to have a history of spontaneous miscarriages. Therefore, the reproductive function also suffers from depression, which seems to be due to the mental illness itself.
Patients with RDD were more likely to have PMS than healthy women, but the difference was not statistically significant. In healthy women, the duration of PMS was significantly longer; PMS symptoms appeared earlier and disappeared later compared with RDD patients. Healthy women were significantly more likely to use analgesics and antispasmodics for PMS. Only 2.3% of patients with RDD subjectively “felt” ovulation, which is possibly due to a smaller number of ovulatory cycles in women suffering from depression compared with healthy ones (12.5%).
Symptoms of PMS in patients and healthy women manifested equally by a complex of vegetative-vascular, metabolic-endocrine and mental disorders. However, while in healthy women psychopathological symptoms of PMS manifested by asthenic, dysphoric, hysterical symptoms, patients with RDD had symptoms of depression, which has prognostic significance during the disease. Interestingly, depressive symptoms as a manifestation of PMS may appear long before the onset of depression and indicate a predisposition to it, as well as being an indicator of the complete recovery from depression.
In general, among patients with RDD, menopause occurred somewhat earlier (median age 50 years [46.0; 52.0]) compared with healthy women (median age 52.0 years [50.0; 53.0]), although the differences was not statistically significant. Patients with RDD and healthy women started experiencing perimenopause symptoms at 48.0 [45.0; 50.0] and 50.0 [48.0; 52.0] years, respectively, p = 0.035*.
The duration of premenopause was significantly (p = 0.037 *) longer in patients with depression (2.0 [1.0; 4.0] years) than in healthy women (1.0 [1.0; 3.0] year). They also were significantly more likely (p = 0.015 *) to have vegetative-vascular manifestations of premenopause (including hot flashes, sweating) (86.7%) than the healthy women (61.5%).
Conclusion
The findings of our study suggest that depression and reproductive function in women are closely related and exert mutual influence on each other. Depression negatively affects the menstrual function, reduces emotions and feelings, impairs sexual function, and ultimately reduces women’ childbearing potential. In those prone to depression, the emotional component of PMS is significantly different and manifests by depressive symptoms. These facts must be considered not only when assessing the female’s mental and gynecological status, but also when choosing treatment options. Treatment of depression in these patients contributes to the restoration of menstrual and childbearing function.
References
- Тювина Н.А. Депрессии у женщин. М.: Издательство «Сервье»; 2006. [Tyuvina NA. Depressii u zhenshchin (Depressions in women). Moscow: Izdatel’stvo «Serv’e»; 2006. (in Russian)]
- Nolen-Hoekesma S. Gender differences in depression. Curr. Direct. Psychol. Sci. 2001; 10(5): 173-6.
- Жиляева Т.В. Предменструальные расстройства настроения: этиология, патогенез, диагностика и лечение (обзор литературы). Проблемы репродукции. 2015; 21(4): 76-85. [Zhilyaeva T.V. Premenstrual mood disorders: etiology, pathogenesis, diagnosis and treatment (literature review). Reproduction problems. 2015; 21 (4): 76-85. (in Russian)]
- Сметник В.П., Кулаков В.И. Руководство по климактерию. М.: МИА; 2001. [Smetnik V.P., Kulakov V.I. Menopause Guide. M .: MIA; 2001. (in Russian)]
- Сметник В.П., Ткаченко Н.М., Глезер Г.А., Москаленко Н.П. Кли- мактерический синдром. М.; 1988. [Smetnik V.P., Tkachenko N.M., Glezer G.A., Moskalenko N.P. Climacteric syndrome. M .; 1988.(in Russian)]
- Юренева С.В., Каменецкая Т.Я. Депрессивные расстройства у женщин в пери- и постменопаузе. Гинекология. 2007; 9(2): 40-3. [Yureneva S.V., Kamenetskaya T.Ya. Depressive disorders in women in peri-and postmenopausal women. Gynecology. 2007; 9 (2): 40-3. (in Russian)]
- Bennett H.A., Einarson A., Taddio A., Koren G., Einarson T.R. Prevalence of depression during pregnancy: systematic review. Obstet. Gynecol. 2004; 103(4): 698-709.
- Bromberger J.T., Kravitz H.M., Chang Y.F., Cyranowski J.M.,Brown C., Matthews K.A. Major depression during and after the menopausal transition: Study of Women’s Health Across the Nation (SWAN). Psychol. Med. 2011; 41(9): 1879-88.
- Bromberger J.T., Matthews K.A., Schott L.L., Brockwell S., Avis N.E., Kravitz H.M. et al. Depressive symptoms during the menopausal transition: the Study of Women’s Health Across the Nation (SWAN). Affect. Disord. 2007; 103(1-3): 267-72.
- Epperson C.N., Steiner M., Hartlage S.A., Eriksson E., Schmidt P.J., Jones I., Yonkers K.A. Premenstrual dysphoric disorder: evidence for a new category for DSM-5. Am. J. Psychiatry. 2012; 169(5): 465-75.
- Ross L., Steiner M. A biopsychosocial approach to premenstrual dysphoric disorder. Psychiatr. Clin. North Am. 2003; 26(3): 529-46.
- Тювина Н.А., Балабанова В.В., Воронина Е.О. Гендерные особенности депрессивных расстройств у женщин. Неврология, нейропсихиатрия, психосоматика. 2015; 7(2): 75-8. [Tyuvina N.A., Balabanova V.V., Voronina E.O. Gender features of depressive disorders in women. Neurology, neuropsychiatry, psychosomatics. 2015; 7 (2): 75-8. (in Russian)]
- Romans S.E., Kreindler D., Asllani E., Einstein G., Laredo S., Levitt A. et al. Mood and the menstrual cycle. Psychother. Psychosom. 2013; 82(1): 53-60.
- Woods N.F., Smith-Dijulio K., Percival D.B., Tao E.Y., Taylor H.J., Mitchell E.S. Symptoms during the menopausal transition and and early postmenopause and their relation to endocrine levels over time: observations from the Seattle Midlife Women’s Health Study. J. Women’s Health (Larchmt). 2007; 16(5): 667-77.
- Viviand-Taylor J., Hickey M. Menopause and depression: is there a link? Maturitas. 2014; 79(2): 142-6.
- Romans S., Clarkson R., Einstein G., Petrovic M., Stewart D. Mood and the menstrual cycle: a review of prospective data studies. Gend. Med. 2012; 9(5): 361-84.
- Rubinow D.R., Schmidt P.J. Gonadal steroid regulation of mood: the lessons of premenstrual syndrome. Front. Neuroendocrinol. 2006; 27(2): 210-6.
- Lokuge S., Frey B.N., Foster J.A., Soares C.N., Steiner M. Depression in women: windows of vulnerability and new insights into the link between estrogen and serotonin. J. Clin. Psychiatry. 2011; 72(11): 1563-9.
- Weiss E.L., Longhurst J.G., Mazure C.M. Childhood sexual abuse as a risk factor for depression in women: Psychosocial and neurobiological correlates. Am. J. Psychiatry. 1999; 156(6): 816-28.
- Young E., Korszun A. Women, stress, and depression: Sex differences in hypothalamic-pituitary-adrenal axis regulation. J. Gend. Specif. Med. 1998; 1(1): 21-7.
- Тювина Н.А. Клинические особенности предменструального синдрома при основных психических заболеваниях: дисс. ... канд. мед. наук. М.; 1983. [Tyuvina NA. Klinicheskie osobennosti predmen- strual’nogo sindroma pri osnovnykh psikhicheskikh zabolevaniyakh. (Clinical features of premenstrual syndrome with major mental illness). Diss. Moscow; 1983. (In Russian)]
Received 15.06.2018
Accepted 22.06.2018
About the Authors
Ivanets, Nikolai N., MD, professor, corr. member of the RAS; honored scientist of the RF; honorary head of the Department of Psychiatry and Addiction Medicine,I.M. Sechenov First MSMU of Minzdrav of Russia (Sechenov University).
119021, Russia, Moscow, Rossolimo str., 11, Bldg. 9. Tel.: +79859998294. ORCID: http://orcid.org/0000-0002-0013-5031
Tyuvina, Nina A., MD, professor, Department of Psychiatry and Addiction Medicine, I.M. Sechenov First MSMU of Minzdrav of Russia (Sechenov University).
119021, Russia, Moscow, Rossolimo str., 11, Bldg. 9. Tel.: +79031030020. E-mail: natuvina@yandex.ru. ORCID: https://orcid.org/0000-0002-5202-1407
Voronina, Ekaterina O., PhD, teaching assistant, Department of Psychiatry and Addiction Medicine, I.M. Sechenov First MSMU of Minzdrav of Russia (Sechenov University). 119021, Russia, Moscow, Rossolimo str., 11, Bldg. 9. Tel.: + 79660656900. E-mail: ekaterinadolores@gmail.com. ORCID https://orcid.org/0000-0001-5751-0579
Balabanova, Vera V., PhD, associate professor, Department of Psychiatry and Addiction Medicine, I.M. Sechenov First MSMU of Minzdrav of Russia (Sechenov University). 119021, Russia, Moscow, Rossolimo str., 11, Bldg. 9. Tel.: +79039641257. E-mail: balabanova@mail.ru. ORCID: https://orcid.org/0000-0001-7420-9585
For citation: Ivanets N.N., Tyuvina N.A., Voronina E.O., Balabanova V.V. Characteristics of reproductive function in women with the recurrent depressive disorder. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2019; (3): 92-7. (in Russian)
https://dx.doi.org/10.18565/aig.2019.3.92-97