The severity of the climacteric syndrome and mobility impairments in women with musculoskeletal disorders and different types of menopause
Nosova L.A., Khashukoeva A.Z., Naumov A.V., Soloveva A.M., Smagina Yu.A.
Relevance: With increasing life expectancy in developed countries, the incidence of age-related musculoskeletal disorders (MSDs) has increased in postmenoupausal women. There is a growing need for exploring new methods for early diagnosis of these conditions.
Objective: To explore the severity of the climacteric syndrome (CS) and mobility impairments in women aged 55–60 years with MSDs and with natural and surgical menopause.
Materials and methods: The study included 104 female patients aged 55–60 years with CS. They were divided into 2 groups; group 1 included 54 women with natural menopause, and group 2 included 50 women with surgical menopause. Assessment of the severity of CS and locomotive syndrome (LS), the state of bone tissue measured by using fragility score, bioimpedance analysis to evaluate muscle tissue status, hand grip dynamometry, and the sit-and-rise test (5 times with no hands) was conducted.
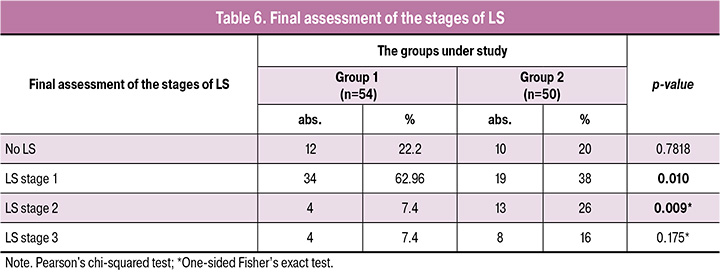
Results: It was found that the group of women with surgical menopause developed severe CS manifestations. The median score of the Greene climacteric scale in this group was 12 (6;19), that was significantly higher than in the group of women with natural menopause – 8.5 (6;17) (p=0.0177). The fragility score of the lumbar spine was lower in group 1 – 26.1 (24.7; 30.8) in comparison with group 2 – 31.1 (26.1; 33.2) (p=0.023). According to the "Locomo 25" questionnaire, the median in group 2 was significantly higher – 12.0 (8; 18) versus 9.6 (3.5; 12) in group 1 (p=0.017). It was found that LS stage 1 was more common in women with natural menopause, while LS stage 2 was associated with surgical menopause.
Conclusion: The obtained results indicate a high prevalence of mobility impairments and musculoskeletal diseases in 55–60 year old women with climacteric syndrome. Therefore, further large-scale multicenter studies are needed.
Authors' contributions: Khashukoeva A.Z., Naumov A.V., Nosova L.A. – development of the concept and design of the study, statistical data analysis; Nosova L.A., Soloveva A.M., Smagina Yu.A. – material collection and processing, manuscript writing; Khashukoeva A.Z. – manuscript editing.
Conflicts of interest: The authors confirm that they have no conflict of interest to declare.
Funding: The study was carried out without any sponsorship.
Ethical Approval: The study was approved by Independent Ethics Committee of the Pirogov Russian National Research Medical University, Ministry of Health of Russia (protocol No. 213 of December 13, 2021).
Patient Consent for Publication: The patients have signed informed consent for publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available on request from the corresponding author after approval from the principal investigator.
For citation: Nosova L.A., Khashukoeva A.Z., Naumov A.V., Soloveva A.M., Smagina Yu.A.
The severity of the climacteric syndrome and mobility impairments in women
with musculoskeletal disorders and different types of menopause.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2025; (3): 92-100 (in Russian)
https://dx.doi.org/10.18565/aig.2025.50
Keywords
In recent decades, there has been the global trend towards increase in life expectancy [1]. Thus, women spend a third of their lives during the postmenopausal period [2].
At the same time, one of the most important problems for women in peri- and postmenopause remains impaired mobility that occurs as a result of musculoskeletal diseases (MSDs) – osteoarthritis, osteoporosis and sarcopenia caused primarily by estrogen deficiency [1, 3–5].
Research on quality of life highlights the growing importance of factors, such as low level of physical activity, musculoskeletal problems, social and role functioning, changes in mental health and sexual dysfunction in menopause [6, 7]. It is known that natural and surgical menopause have different consequences for womеn's health. In particular, surgical menopause is often accompanied by sharp and sudden changes in hormonal status of women, that commonly leads to more pronounced clinical manifestations of the climacteric syndrome (CS) [6, 8–11].
Literature data on relationship between the type of menopause and mobility impairments are controversial.
On the one hand, the women who have undergone surgical menopause have a higher risk of developing musculoskeletal disorders, that highlights the potential importance of hormonal levels in the development of musculoskeletal diseases in postmenopause [1, 10, 12].
On the other hand, there are data indicating no association between surgical menopause and the development of senile asthenia (or frailty) in future. However, inclusion criteria in the study were relatively healthy women [13].
Given the importance of complications of MSDs, such as increased risk of mortality and disability in older adults, it is necessary to explore early measures for the detection and prevention of these diseases [14].
In 2007, the Japanese Orthopedic Association proposed a concept of locomotive syndrome, which is defined as reduced mobility due to impairment of locomotive organs [15–17]. Initially it was intended to detect LS in older people, but event among young population, one in five persons has LS [18].
The prevalence of LS in postmenopausal women is significantly higher compared with men – 88.4% and 66.7, respectively [19, 20].
A number of authors reported that the use of menopausal hormone therapy (MHT) can reduce the risk of developing MSDs [21, 22]. Given the fact that modern women want to maintain active and healthy longevity, the existing problem plays one of the leading roles in ensuring quality of life in peri- and postmenopause.
The aim of this study was to explore the severity of the climacteric syndrome and mobility impairments in women aged 55–60 years with MSDs and with natural and surgical menopause.
Material and methods
The study included 104 female patients aged 55–60 years with the climacteric syndrome. They were divided into 2 groups: group 1 included 54 women with natural menopause, and group 2 included 50 women with surgical menopause, who underwent bilateral oophorectomy or adnexectomy in history.
Inclusion criteria were women with CS aged 55–60 years.
Non-inclusion criteria were oncological diseases, disorders of the hematopoietic system, neurodegenerative disorders, past strokes, cognitive impairment, Parkinson's disease and Alzheimer's disease, fever, unexplained weight loss, gastrointestinal diseases requiring parenteral nutrition, rheumatism, chronic kidney disease, the use of menopausal hormone therapy, as well as no desire or ability to participate in the study.
Assessment of the severity of CS in women at that time and retrospective analysis of the severity of CS in perimenopause or in the perioperative period was performed using of the Greene climacteric scale [23, 24].
Assessment of muscle mass and strength was conducted using hand-grip dynamometry, bioimpedansometry, five times sit-to-stand test (5xSST) without use of arms. Bone mineral density (BMD) of lumbar spine and the proximal femur was assessed using Radiofrequency Echographic Multi Spectrometry (REMS).
Assessment of LS was performed using the stand-up test from stools of different heights, two-step test, and the 25-question Geriatric Locomotive Function Scale (GLFS-25). The severity of LS was determined by the worst test score.
The study was carried out in compliance with ethical norms and standards.
Statistical analysis
Statistical software packages IBM SPSS Statistics V22 (IBM Corp., США) and Statistica V12 were used for statistical data analysis.
The obtained quantitative parameters were tested for compliance with the normal distribution using the Shapiro–Wilk test. It was assumed that distribution was similar to the normal distribution (the null hypothesis suggests that the distributions are identical). When p-value was less than 0.05, the null hypothesis was rejected. Accordingly, distribution of the data in the study differed from the normal distribution.
The numerical parameters with normal distribution are represented as M (SD), where M is the mean value, SD is the standard deviation. The parameters different from the normal distribution are represented as Me (Q25%; Q75%), where Me is the median, and Q25% and Q75% are the upper and lower quartiles. The qualitative data are represented as absolute and relative values (%).
Student’s t-test was used to find the differences between the groups of patients in normally distributed numerical indicators for two independent samples. When confirmation of the hypothesis of normal distribution failed, the nonparametric Mann–Whitney U-test for two unrelated groups was used to compare the quantitative data.
Pearson's chi-squared test with Yates' continuity correction or Fisher's exact test for small samples was used to compare dichotomous variables between independent samples. When Pearson's chi squared test was not the appropriate test, the Z-test for comparing the proportions (similar to Student's t-test for proportions) and with correction of endpoints for the proportions of 0% and 100%, was used.
To test statistical hypotheses, the critical value of significance level was equal to 0.05. Correlation analysis was on carried out on the basis of nonparametric Spearman's rank correlation.
Results
There was no significant difference in the mean age of the participants in the groups, and was 57.9 (1.6) years и 57.6 (2,2) years, respectively (р>0.05).
Assessment of body mass index (BMI) showed that only 9.3% (5/54) of patients in group 1, and 30.0% (15/50) of patients in group 2 had normal weight. Obesity was in the other patients – stage one in 74.1% (40/54) and 60.0% (30/50), stage 2 in 11.0% (6/54) and 6.0% (3/50), stage 3 in 5.6% (3/54) and 4.0% (2/50) of women, respectively.
Hypertension was diagnosed in 40.7% (22/54) and 38.0% (19/50) of women; varicose veins were in 25.9% (14/54) and 32.0% (16/50) of women; gastrointestinal diseases were detected in 20.4% (11/54) and 28.0% (14/50) of patients; type 2 diabetes mellitus was in 7.4% (4/54) and 12.0% (6/50) of women, respectively (р>0.05).
The mean age of the onset of menopause was significantly higher in group 1 and was 51 (2.7) years versus 48.18 (2.5) years in group 2 (р=0,026, the Student’s t-test). The length of postmenopause by the time of patient examination was 7 (5; 10) years in group 1 versus 9.5 (7; 11) years in group 2 (р=0.0002, the Mann–Whitney U-test).
The typical climacteric symptoms were in all participants of the study. There were no statistically significant differences in complaints (р>0.05) (Table 1).
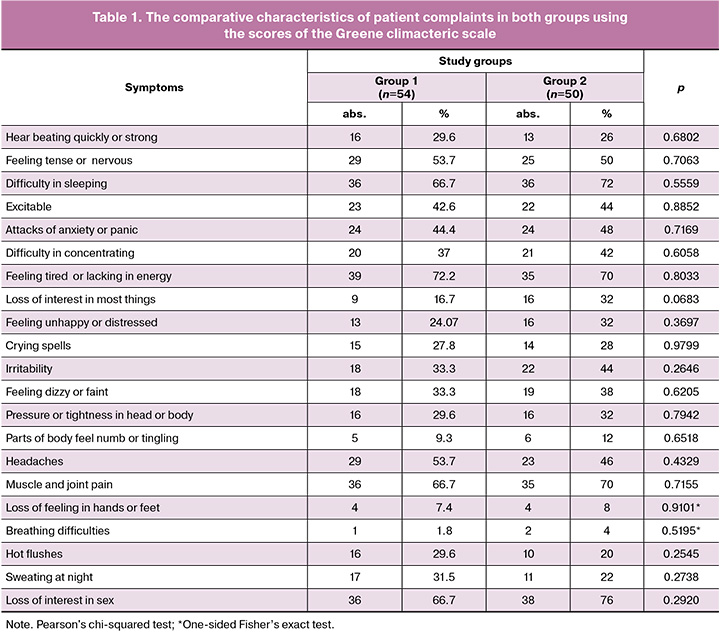
Muscle and joint pain was a health complaint in 66.7% (36/54) of women in group 1 and 70.0% (35/50) of women in group two. Difficulty in sleeping was a complaint in 66.7% (36/54) and 72.0% (36/50) of women, respectively (р>0.05).
However, analysis of the data showed that in general, in the group of women with surgical menopause the degree of severity of the climacteric syndrome was higher. The median score of the Greene climacteric scale was significantly higher in group 2 and was 12 (6;19) versus 8.5 (6;17) in the group of women with natural menopause (р=0.0177, the Mann–Whitney U test (Fig. 1).
Assessment of the severity of CS found no statistically significant differences between the groups (р>0.05).
At the same time, the retrospective analysis showed that women who underwent surgical menopause, had severe symptoms of CS in the postoperative period more often versus women with natural menopause in the perimenopausal period. Thus, in group 2, 16 patients experienced severe manifestations of CS in the early postoperative period, and 8 patients in group 1 had severe CS in perimenopause (р=0.038, Pearson's chi-squared test).
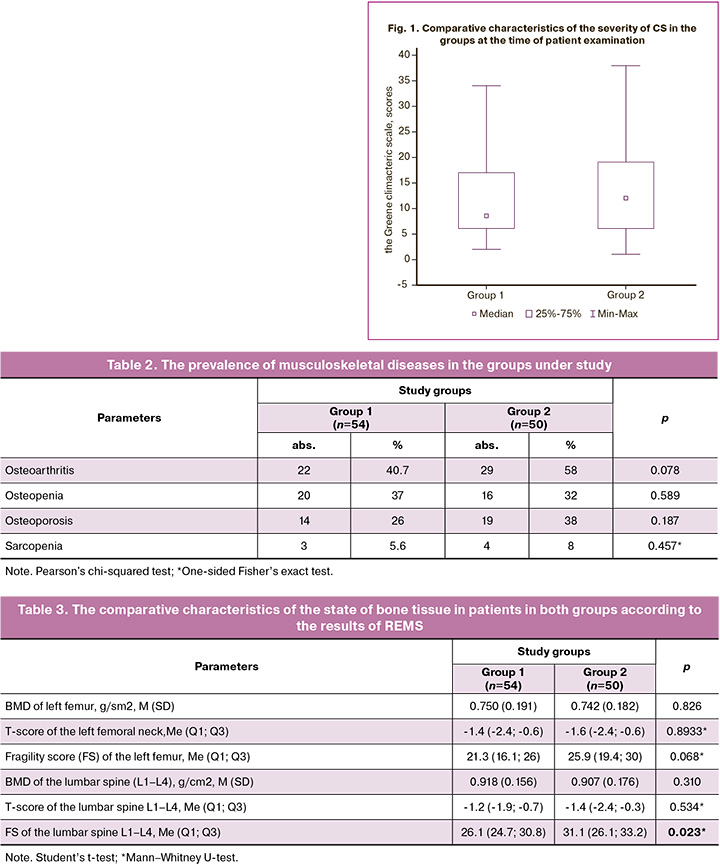
There were no statistically significant differences in the prevalence of musculoskeletal diseases between the groups (Table 2).
The comparative characteristics of the state of bone tissue according to the results of REMS is represented in Table 3.
Fragility score of lumbar spine was significantly low in group 1 – 26.1 (24.7; 30.8), while it was 31.1 (26.1; 33.2) (р=0,023) in group 2.
Assessment of mobility impairments is represented in Table 4.
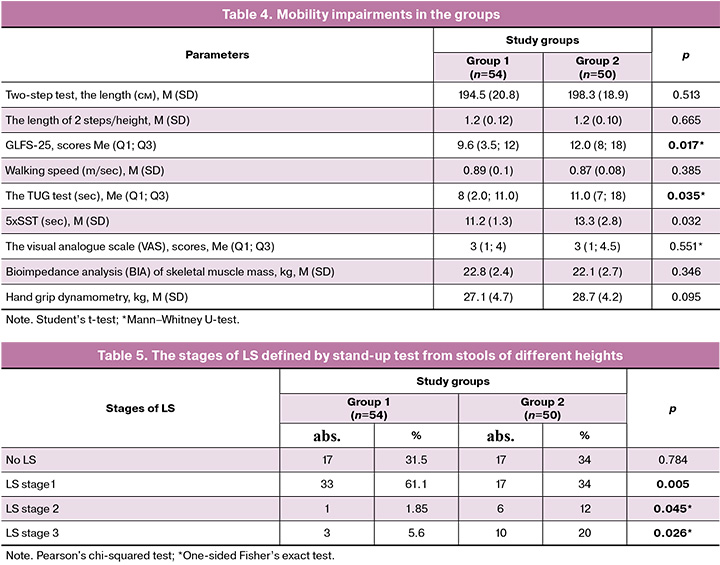
Assessment of the main parameters of LS in the groups showed that statistically significant differences were found in the scores of the 25-question Geriatric Locomotive Function Scale and the Timed Up and Go test (TUG), that indicates more pronounced mobility impairments in group 2.
Thus, in group 2, the median score of GLFS-25 was significantly higher – 12.0 (8; 18) versus 9.6 (3.5; 12) in group 1 (р=0.017, the Mann–Whitney U-test), that indicates more pronounced mobility impairments in group 2 (Fig. 2).
In group 1, the mean time of Up and Go test was significantly less and was 6.9 (6.2; 9.5) seconds versus 7.8 (6.4; 9.5) seconds in group 2 (р=0.035), that indicated more pronounced movement impairments in group 2 (Fig. 3).

Assessment of LS using stand-up test from stools of different heights showed that severe stages of LS were found in women with surgical menopause (Table 5).
Final assessment of the stages of LS found no statistically significant differences in the groups between the absence of LS and the most severe stage 3. However, LS stage 1 (mild stage) was significantly more common in women aged 55–60 with natural menopause (p=0.010), and LS stage 2 was more common in women aged 55–60 with surgical menopause (p=0.009).
Discussion
The study found high prevalence of MSDs in women with CS in postmenopause: in group 1, osteoarthritis was in 40.7% of women; osteopenia was in 37.0%, osteoporosis was in 26.0%, sarcopenia was in 5.6% of patients; in group 2, MSDs were in 58.0, 32.0, 38.0 and 8.0% of women, respectively.
MSDs are interrelated. Osteoarthritis often accompanies osteopenia (osteoporosis), and osteopenia accompanies sarcopenia [25, 26]. Also it was found that bone mineral density (BMD) is low in women aged 35–69 years (the mean age 54.7 (9.1) years and is associated with a high risk of sarcopenia (OR=1.77; 95% CI 1.02–3.06) [27].
However, according to the data obtained by bioimpedansometry and functional strength tests in our study, the percentage of detected sarcopenia was lower than osteopenic syndrome, that may indicate the need to identify women with the osteopenic syndrome as a separate risk group for developing this disease in future. Sarcopenia and osteoporosis can be asymptomatic for a long time. So, the study by Sriramaneni N. et al. (2024) reported that most women felt physically strong (according to the scores of SARC-F questionnaire), despite the presence of sarcopenia [28]. Hormonal changes associated with menopause may contribute to the development of sarcopenia and osteoporosis in most women, as well as lead to mobility-related disability and falls at a later age [29].
It is known that low estrogen secretion by the ovaries in postmenopause contributes to the rapid bone loss [30]. The study by Sipilä S. et al. (2020) reported that a decrease in bone mineral density and skeletal muscles weakness are associated with the menopause transition [29]. Also, estrogen deficiency in peri- and early postmenopause is associated with loss of BMD and degenerative changes in cartilage and skeletal muscles [22].
Musculoskeletal pain (myalgia) and joint pain (arthralgia) are the most prominent manifestations of CS.
It is estimated that over 50% of women experience arthralgia or arthritis at the time of menopause [31].
Given the fact that this is an important and common problem, a review of scientific papers was published in 2024, where a new term "the musculoskeletal syndrome of menopause” was offered to describe the common musculoskeletal signs and symptoms related to loss of estrogen levels. The musculoskeletal syndrome of menopause includes musculoskeletal pain, arthralgia, loss of dry muscle mass, loss of bone density with increased risk of the subsequent fracture, tendon and ligament injuries, adhesive capsulitis and cartilage matrix fragility with progression of osteoarthritis [32].
It has been shown that cartilage degradation is less in women taking levormeloxifene – a selective estrogen receptor modulator, or MHT. In addition, the women taking MHT demonstrated reduced rate of cartilage degeneration [33]. Health study “The Women's Health Initiative” (WHI) also showed the total number of joint surgeries reduced by 45% among women taking MHT compared to patients taking a placebo [34]. The women with surgical menopause suffer from severe CS and MSDs more often, that is consistent with the results obtained in our study. [10, 35].
Early diagnosis of LS makes it possible to use preventive and therapeutic interventions to prevent its progression [17].
Conclusion
The study showed that in women with surgical menopause, severe CS most often occurred in the early postoperative period. Higher fragility score according to REMS and LS stage 2 was in 55–60 year old women, that may indicate severe mobility impairments in women with natural menopause.
This study is the first stage of a research project aimed at assessment of further strategy for management and improvement of quality of life of women with CS.
The most promising direction for further research is exploration of preventive measures for progression of LS in women with CS.
References
- Сулима А.Н., Булюк В.В., Митрофанова О.А. Постменопаузальный остеопороз. Акушерство и гинекология. 2023; 9: 52-59. [Sulima A.N., Bulyuk V.V., Mitrofanova O.A. Postmenopausal osteoporosis. Obstetrics and Gynecology. 2023; (9): 52-9. (in Russian)]. https://dx.doi.org/10.18565/aig.2023.103.
- Хашукоева А.З., Кузнецова О.В., Оверко А.В., Дмитрашко Т.Е. Как жить пожилой женщине с выпадением половых органов? Лечащий Врач. 2021; 12(24): 10-6. [Khashukoeva A.Z., Kuznetsova O.V., Overko A.V., Dmitrashko I.E. How to live an elderly woman with prolapse of the genitals? Lechaschy Vrach Journal. 2021; 12(24): 10-6. (in Russian)]. https://dx.doi.org/10.51793/OS.2021.24.12.001.
- Jin Z., Tian C., Kang M., Hu S., Zhao L., Zhang W. The 100 top-cited articles in menopausal syndrome: a bibliometric analysis. Reprod. Health. 2024; 21(1): 47. https://dx.doi.org/10.1186/s12978-024-01770-9.
- Усова Н.Н., Ходькова Ю.В. Особенности развития болевых синдромов в пожилом возрасте. Медицинские новости. 2022; 2: 24-7. [Usava N.N., Khodkova Yu.V. Features of the development of pain syndromes in old age. Medical News. 2022; 2: 24-7. (in Russian)].
- Di Martino A., Barile F., D'Agostino C., Castafaro V., Cerasoli T., Mora P. et al. Are there gender-specific differences in hip and knee cartilage composition and degeneration? A systematic literature review. Eur. J. Orthop. Surg. Traumatol. 2024; 34(4): 1901-10. https://dx.doi.org/10.1007/s00590-024-03871-4.
- Брюхина Е.В., Усольцева Е.Н., Иванова О.В. Качество жизни женщин в зависимости от проявлений климактерического синдрома. Акушерство и гинекология. 2014; 10: 52-8. [Bryukhina E.V., Usoltseva E.N., Ivanova O.V. The quality of life in women according to climacteric syndrome. Obstetrics and Gynecology. 2014; (10): 52-8. (in Russian)].
- Умарова Н.М., Абдикулова Н.Х., Нигматова Г.М. Остеопороз у женщин в перименопаузе. Пути диагностики, коррекции и профилактики (обзор литературы). Журнал репродуктивного здоровья и уро-нефрологических исследований. 2024; 5(1): 5-8. [Umarova N.M., Abdikulova N.Kh., Nigmatova G.M. Osteoporosis in perimenopausal women. Diagnostic, correction and prevention pathways (literature review). Journal of Reproductive Health and Uro-Nephrological Research. 2024; 5(1): 5-8. (in Russian)]. https://dx.doi.org/10.5281/zenodo.10909224.
- Tomida M., Otsuka R., Tange C., Nishita Y., Kimura T., Stoelzel M. et al. Vasomotor symptoms, sleep problems, and depressive symptoms in community-dwelling Japanese women. J. Obstet. Gynaecol. Res. 2021; 47(10): 3677-90. https://dx.doi.org/10.1111/jog.14937.
- Pillay O.C., Manyonda I. The surgical menopause. Best Pract. Res. Clin. Obstet. Gynaecol. 2022; 81: 111-8. https://dx.doi.org/10.1016/j.bpobgyn.2022.03.001.
- Ozdemir S., Celik C., Görkemli H., Kiyici A., Kaya B. Compared effects of surgical and natural menopause on climacteric symptoms, osteoporosis, and metabolic syndrome. Int. J. Gynaecol. Obstet. 2009; 106(1): 57-61. https://dx.doi.org/10.1016/j.ijgo.2009.03.016.
- Коротких И.Н., Савельева Н.В., Боржи У.М. Основные проблемы естественной и хирургической менопаузы. Научно-медицинский вестник Центрального Черноземья. 2006; 26: 85-9. [Korotkikh I.N., Savelyeva N.V., Borzhi U.M. Main problems of natural and surgical menopause. Medical Scientific Bulletin of Central Chernozemye. 2006; 26: 85-9. (in Russian)]. https://dx.doi.org/10.18499/1990-472X-2006-0-26-85-89.
- Vallejo M.S., Blümel J.E., Chedraui P., Tserotas K., Salinas C., Rodrigues M.A. et al. Association of muscle disorders in late postmenopausal women according to the type of experienced menopause. Menopause. 2024; 31(7): 641-6. https://dx.doi.org/10.1097/GME.0000000000002367.
- Huang G., Coviello A., LaValley M.P., Ensrud K.E., Cauley J.A., Cawthon P.M. et al. Surgical menopause and frailty risk in community-dwelling older women: study of osteoporotic fractures. J. Am. Geriatr. Soc. 2018; 66(11): 2172-7. https://dx.doi.org/10.1111/jgs.15505.
- Veronese N., Ragusa F.S., Sabico S., Dominguez L.J., Barbagallo M., Duque G. et al. Osteosarcopenia increases the risk of mortality: a systematic review and meta-analysis of prospective observational studies. Aging Clin. Exp. Res. 2024; 36(1): 132. https://dx.doi.org/10.1007/s40520-024-02785-9.
- Nakamura K. A "super-aged" society and the "locomotive syndrome". J. Orthop. Sci. 2008; 13(1): 1-2. https://dx.doi.org/10.1007/s00776-007-1202-6.
- Nakamura K., Ogata T. Locomotive syndrome: definition and management. Clin. Rev. Bone Miner. Metab. 2016; 14(2): 56-67. https://dx.doi.org/10.1007/s12018-016-9208-2.
- Shibata S., Kon S. Functional ingredients associated with the prevention and suppression of locomotive syndrome: a review. Biol. Pharm. Bull. 2024; 47(12): 1978-91. https://dx.doi.org/10.1248/bpb.b24-00443.
- Sawaya Y., Hirose T., Onuma S., Nakajima R., Fujita S., Muroi S. et al. Prevalence and associated factors of locomotive syndrome in young Japanese adults: a cross-sectional study. BMC Musculoskelet. Disord. 2024; 25(1): 366. https://dx.doi.org/10.1186/s12891-024-07493-z.
- Тополянская С.В., Романова М.А., Вакуленко О.Н., Бубман Л.И., Елисеева Т.А., Ларина Д.С., Рачина С.А., Дворецкий Л.И. «Локомотивный синдром» в практике гериатрического стационара. Медицинский алфавит. 2023; 13: 36-41. [Topolyanskaya S.V., Romanova M.A., Vakulenko O.N., Bubman L.I., Eliseeva T.A., Larina D.S., Ratchina S.A., Dvoretski L.I. «Locomotive syndrome» in patients in the geriatric hospital. Medical Alphabet. 2023; (13): 36-41. (in Russian)]. https://dx.doi.org/10.33667/10.33667/2078-5631-2023-13-36-41.
- Ikemoto T., Arai Y.C. Locomotive syndrome: clinical perspectives. Clin. Interv. Aging. 2018; 13: 819-27. https://dx.doi.org/10.2147/CIA.S148683.
- Ota K. Clinical anti-aging medicine: Anti-aging medicine for female reproductive organs. In: Yamada H., Yuji N., eds. Anti-aging medicine. Basics and clinical practice. Springer; 2025: 325-9. https://dx.doi.org/10.1007/978-981-97-8514-8_81.
- Якушевская О.В., Юренева С.В., Комедина В.И. Па-де-де остеопороза и саркопении: остеосаркопения. Медицинский совет. 2022; 6: 116-21. [Yakushevskaya O.V., Yureneva S.V., Komedina V.I. A pas de deux of osteoporosis and sarcopenia: osteosarcopenia. Medical Council. 2022; (6): 116-21. (in Russian)]. https://dx.doi.org/10.21518/2079-701X-2022-16-6-116-121.
- Greene J.G. Constructing a standard climacteric scale. Maturitas. 2008; 61(1-2): 78-84. https://dx.doi.org/10.1016/j.maturitas.2008.09.011.
- Sourouni M., Zangger M., Honermann L., Foth D., Stute P. Assessment of the climacteric syndrome: a narrative review. Arch. Gynecol. Obstet. 2021; 304(4): 855-62. https://dx.doi.org/10.1007/s00404-021-06139-y.
- Osawa Y., An Y., Nishita Y., Matsui Y., Takemura M., Simonsick E.M. et al. Longitudinal association between muscle and bone loss: Results of US and Japanese cohort studies. J. Cachexia Sarcopenia Muscle. 2024; 15(2): 746-55. https://dx.doi.org/10.1002/jcsm.13438.
- Торопцова Н.В. Взаимосвязь остеопороза и остеоартроза. Лечащий врач. 2006; 2: 38-42. [Toroptsova N.V. Relationship between osteoporosis and osteoarthritis. Lechaschi Vrach Journal. 2006; (2): 38-42. (in Russian)].
- Campodónico I., Blümel J.E., Arteaga E., Vallejo M.S., Valdivia M.I. Low bone mineral density in middle-aged women: a red flag for sarcopenia. Menopause. 2018; 25(3): 324-8. https://dx.doi.org/10.1097/GME.0000000000000995.
- Sriramaneni N., Selvan C., Kumar S.N., Kalra P., P G.Y., R M.P. et al. Quality of life in postmenopausal women and its association with sarcopenia. Menopause. 2024; 31(8): 679-85. https://dx.doi.org/10.1097/GME.0000000000002378.
- Sipilä S., Törmäkangas T., Sillanpää E., Aukee P., Kujala U.M., Kovanen V. et al. Muscle and bone mass in middle-aged women: role of menopausal status and physical activity. Journal of Cachexia, Sarcopenia and Muscle. 2020; 11(3):698-709. https://dx.doi.org/10.1002/jcsm.12547.
- Кузнецов С.Ю. Клинические аспекты женского здоровья: половые стероиды и костная ткань. Остеопороз и остеопатии. 2022; 25(3): 72-3. [Kuznetsov S.Yu. Clinical aspects of women's health: sex steroids and bone tissue. Osteoporosis and Bone Diseases. 2022; 25(3): 72-3. (in Russian)]. https://dx.doi.org/10.14341/osteo13041.
- Blumer J. Arthralgia of menopause - A retrospective review. Post Reprod. Health. 2023; 29(2): 95-7. https://dx.doi.org/10.1177/20533691231172565.
- Wright V.J., Schwartzman J.D., Itinoche R., Wittstein J. The musculoskeletal syndrome of menopause. Climacteric. 2024; 27(5): 466-72. https://dx.doi.org/10.1080/13697137.2024.2380363.
- Wluka A.E., Davis S.R., Bailey M., Stuckey S.L., Cicuttini F.M. Users of oestrogen replacement therapy have more knee cartilage than non-users. Ann. Rheum. Dis. 2001; 60: 332-6. https://dx.doi.org/10.1136/ard.60.4.332.
- Cirillo D.J., Wallace R.B., Wu L., Yood R.A. Effect of hormone therapy on risk of hip and knee joint replacement in the Women's Health Initiative. Arthritis. Rheum. 2006; 54(10): 3194-204. https://dx.doi.org/10.1002/art.22138.
- Колбасова Е.А., Киселева Н.И., Арестова И.М. Сравнительная клинико-гормональная характеристика состояния здоровья и качество жизни женщин с хирургической и естественной менопаузой. Вестник Витебского государственного медицинского университета. 2014; 13(2): 78-86. [Kolbasova E.A., Kiseleva N.I., Arestova I.M. Comparative clinical and hormonal characteristics of the state of health and quality of life of women with surgical and natural menopause. Bulletin of Vitebsk State Medical University. 2014; 13(2): 78-86. (in Russian)].
Received 30.01.2025
Accepted 26.02.2025
About the Authors
Lilia A. Nosova, Teaching Assistant at the Department of Obstetrics and Gynecology, Institute of Surgery, Pirogov Russian National Research Medical University,Ministry of Health of Russia, 117997, Russia, Moscow, Ostrovityanov str., 1, karelina_lilia@mail.ru, https://orcid.org/0000-0002-0925-3755
Asiyat Z. Khashukoeva, Dr. Med. Sci., Professor, Professor at the Department of Obstetrics and Gynecology, Institute of Surgery, Pirogov Russian National Research Medical University, Ministry of Health of Russia, 117997, Russia, Moscow, Ostrovityanov str., 1; obstetrician-gynecologist, Russian Gerontological Research and Clinical Center, 129226, Russia, Moscow, 1st Leonova str., 16, azk05@mail.ru, https://orcid.org/0000-0001-7591-6281
Anton V. Naumov, Dr. Med. Sci., Professor at the Department of Diseases of Aging, Faculty of Additional Professional Education, Pirogov Russian National Research Medical University, Ministry of Health of Russia, 117997, Russia, Moscow, Ostrovityanov str., 1; Head of the Laboratory of Diseases of the Musculoskeletal System, Russian Gerontological Research and Clinical Center, 129226, Russia, Moscow, 1st Leonova str., 16, nanton@mail.ru, https://orcid.org/0000-0002-6253-621X
Anna M. Soloveva, student, Pirogov Russian National Research Medical University, Ministry of Health of Russia, 117997, Russia, Moscow, Ostrovityanov str., 1,
annasol02@yandex.ru, https://orcid.org/0009-0006-9569-5045
Yulia A. Smagina, student, Pirogov Russian National Research Medical University, Ministry of Health of Russia, 117997, Russia, Moscow, Ostrovityanov str., 1,
yulia-smagina709@mail.ru, https://orcid.org/0009-0009-3893-4988
Corresponding author: Asiyat Z. Khashukoeva, azk05@mail.ru