Risk factors for threatened preterm labor: a clinical and epidemiological study
Objective. To identify risk factors for threatened preterm labor in modern conditions on the basis of longitudinal clinical and epidemiological study.Nazarova А.О., Malyshkina А.I., Nazarov S.B., Boyko E.L.
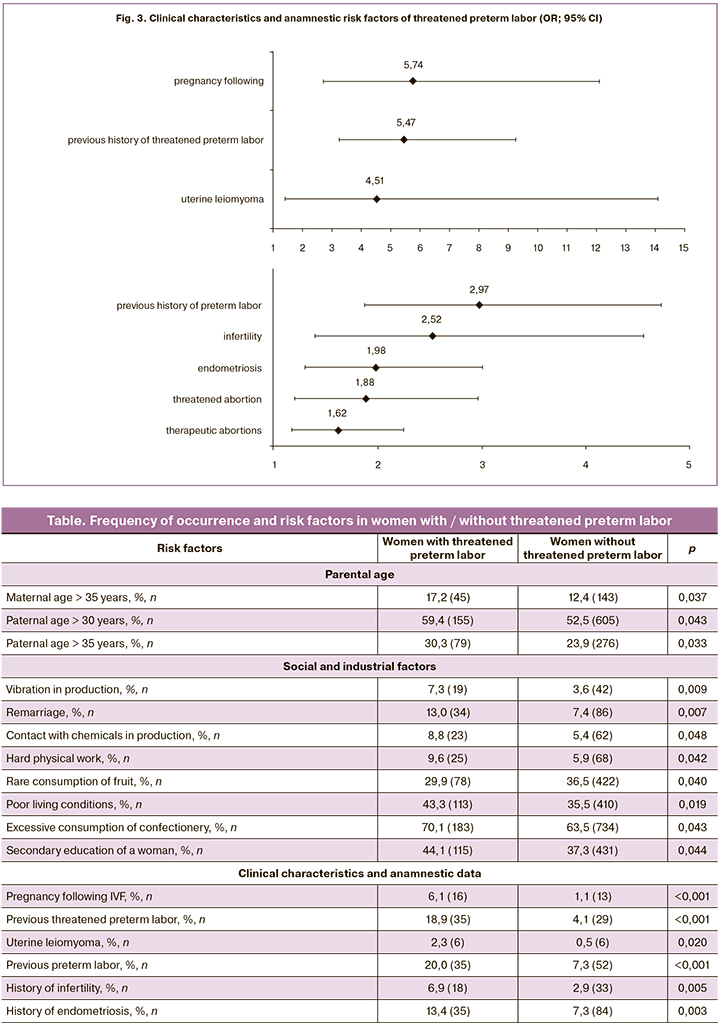
Materials and methods. This was a continuous longitudinal clinical and epidemiological study of 1417 pregnant women of the Ivanovo region in the early stages of pregnancy. The survey included 261 women with a risk of preterm birth during the current pregnancy and 1156 women with normal course of pregnancy or other obstetric abnormalities.
Results. The study revealed 25 risk factors for threatened preterm labor. The most significant factors are pregnancy following IVF, previous history of threatened preterm labor, uterine leiomyoma, previous history of threatened abortion and preterm labor, infertility. The present study identified the differences in risk factors for threatened preterm labor and spontaneous preterm labor.
Conclusion. The findings on risk factors for threatened preterm labor can be included in information systems monitoring pregnant women with the aim of detecting groups at risk and timely decision making about the obstetric department where a pregnant woman should be admitted for the delivery.
Keywords
Preterm labor has been one of the greatest challenges for obstetricians and pediatricians. This is due to the fact that premature newborns account for up to 85% of perinatal mortality and morbidity rate and more than 55% of neonatal mortality rate. Despite the existing arsenal of medicines aimed at prolonging pregnancy, the rate of preterm labor in different countries ranges from 5 to 18% [1, 2]. According to the World Health Organization (WHO), of 65 countries with reliable trend data, all but 3 show an increase in preterm birth rates over the past 20 years. [2].
The knowledge of the risk factors of certain diseases is an important condition for developing prevention strategies at the population level and can provide a personalized approach to prevention and treatment in a particular patient. Risk factors of preterm labor have been investigated in numerous studies and they are well represented in various Russian and foreign guidelines [3–5]. In our previous study, we updated the data on the risk factors of spontaneous preterm labor in modern conditions [6].
However, we have not found information about risk factors of threatened preterm labor in the literature available to us. Preterm labor is preceded by threatened preterm labor which is easier to manage. Therefore, the knowledge of risk factors of threatened preterm labor can assist in preventing premature labor and managing pregnant women.
The aim of the study was to identify risk factors of threatened preterm labor in modern conditions on the basis of longitudinal clinical and epidemiological study.
Materials and Methods
This was a continuous longitudinal clinical and epidemiological study of 1417 pregnant women of the Ivanovo region between 2013 and 2018. The study included 261 women with a risk of preterm birth during the current pregnancy and 1156 women with a normal course of pregnancy or other obstetric abnormalities. Pregnant women were surveyed on the basis of voluntary informed consent when registering at an antenatal clinic in the early stages of pregnancy. For this purpose, a special chart was developed which included characteristics of social, professional, and material conditions, as well as obstetric and gynecological history, somatic anamnesis, and assessment of medical awareness.
Statistical analysis
Differences in relative indicators were determined using chi-square test and considered statistically significant at the level of p<0.05. In order to carry out quantitative assessment of various risk factors, we performed the odds ratio (OR) calculation using the OpenEpi online calculator: Open Source Epidemiological Statistics for Public Health (Version 3.03, www.OpenEpi.com).
 Results and Discussion
Results and Discussion
The results of the study showed that the rate of threatened preterm labor in pregnant women included in the study in the Ivanovo region was 18.4 %. Thus, it was necessary to administer maintenance tocolytic therapy to every fifth woman in an antenatal clinic or obstetric department.
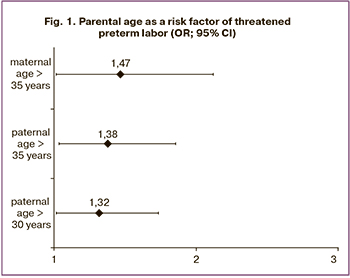
The age of the expectant parents as a risk factor is of critical importance for developing threatened preterm labor. The negative impact of the maternal age manifests only after 35 years (Table, Fig. 1). Paternal age starts being a risk factor of threatened preterm labor after 30 years, but its influence is less remarkable than one of the maternal age.
Among social and industrial factors, women’s secondary education, hard physical work, contact with chemicals in production, remarriage, and vibration in production (this is mainly work in the sewing industry in the Ivanovo region) have a negative impact (Table, Fig. 2). The adverse effect can be produced by excessive consumption of confectionery, insufficient consumption of fresh fruit, and poor living conditions.
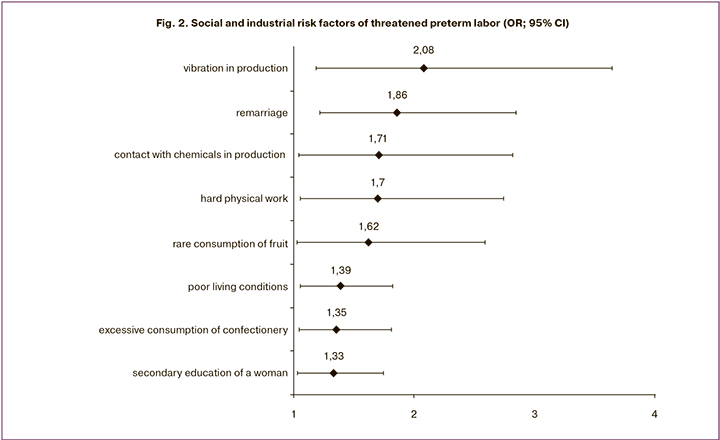
Clinical characteristics and anamnestic risk factors include therapeutic abortion, threatened abortion, endometriosis, infertility, previous preterm labor, uterine leiomyoma, previous threatened preterm labor, pregnancy following IVF (Table, Fig. 3).
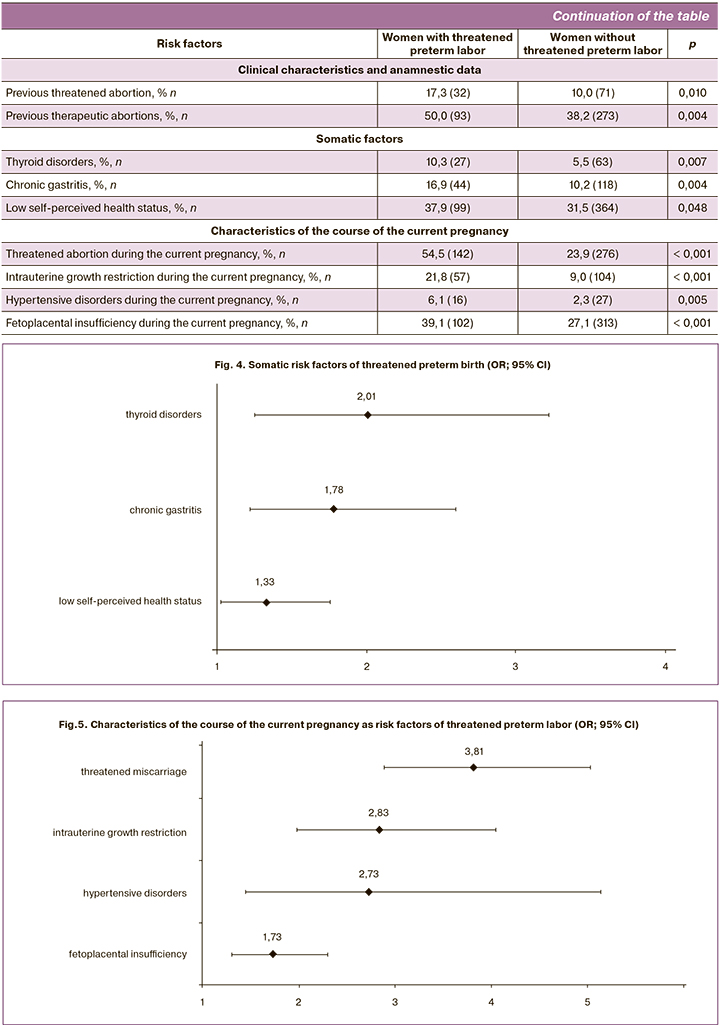
The risk for threatened preterm labor increases in case of somatic disorders. Somatic factors include chronic gastritis and thyroid disorders in combination with low self-perceived health status (Table, Fig. 4).
A number of risk factors of threatened preterm labor additionally appear during the current pregnancy. The risk for threatened preterm pregnancy increases in fetoplacental insufficiency, hypertensive disorders, intrauterine growth restriction and threatened abortion (Table, Fig. 5).
Thus, we evaluated the risk factors of threatened preterm labor on the basis of a continuous longitudinal study of pregnant women of the Ivanovo region, starting from early gestation, and identified 25 risk factors.
The most significant factors are pregnancy following IVF, previous history of threatened preterm labor, uterine leiomyoma, previous history of threatened abortion and preterm labor, infertility.
We conducted a comparative analysis of the obtained data with the results of our previous study of risk factors of preterm labor [6]. A total of 17 factors were identified for spontaneous preterm labor and 25 factors for threatened preterm labor. Most of the high-risk factors are common. An additional high-risk factor for threatened preterm labor is previous history of infertility, which is consistent with the data of the WHO experts, who consider previous infertility as a cause of the increasing frequency of preterm labor in the world [2].
In comparison with preterm labor, additional risk factors of threatened preterm labor are remarriage, contact with chemicals at production, hard physical work, insufficient consumption of fresh fruit, excessive consumption of confectionery, poor living conditions, previous history of endometriosis and threatened abortion, thyroid disorders, chronic gastritis, low self-perceived health status, hypertensive disorders during this pregnancy.
Interestingly, a number of previously identified risk factors of spontaneous preterm labor [6] do not influence threatened preterm labor. These factors include maternal smoking, a previous history of vaginitis, lack of contraception before pregnancy, and premature birth of the mother.
The obtained data can be used in preconception care programs and indicate the need for normalization of the function of the thyroid gland, as well as persistent remission of chronic gastritis. The correction of thyroid function is likely to be particularly relevant in regions that are endemic for iodine deficiency, such as the Ivanovo region [7]. Starting from the early stages of pregnancy, it is necessary to correct the diet, which should increase the consumption of fresh fruit and limit easily digested carbohydrates, which is consistent to the recommendations of other authors [8].
Conclusion
The findings on risk factors for threatened preterm labor can be included in information systems monitoring pregnant women with the aim of detecting groups at risk and timely decision making about the obstetric department where a pregnant woman should be admitted for the delivery.
References
- World Health Organization. Preterm birth. Fact sheet No.363. Update November 2013.
- WHO recommendations on interventions to improve preterm birth outcomes. Guideline WQ 330. November 2015.
- Сухих Г.Т., Серов В.Н., Адамян Л.В., Филиппов О.С., Баев О.Р., Климченко Н.И., Тетруашвили Н.К., Тютюнник В.Л., Ходжаева З.С., Холин А.М. Преждевременные роды. Клинические рекомендации (протокол). М.: Научный центр акушерства, гинекологии и перинатологии имени академика В.И. Кулакова; 2014. 35 с. [Sukhih G.T., Serov V.N., Adamyan L.V., Filippov O.S., Baev O.R., Klimchenko N.I., Tetruashvili N.K.,Tyutyunnik V.L., Khodzhayeva Z.S., Kholin A.M. Preterm birth: Clinical recommendations (Protocol). Moscow: Scientific center of obstetrics, gynecology and Perinatology named after academician V.I. Kulakov; 2014. 35 p. (in Russian)].
- Medical information of Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/preterm-labor/symptoms-causes/syc-20376842.
- Medical information of National Institute of Child Health and Human Development, National Institute of Health, USA. https://www.nichd.nih.gov/health/topics/preterm/conditioninfo/who_risk.
- Назарова А.О., Малышкина А.И., Назаров С.Б. Факторы риска спонтанных преждевременных родов: результаты клинико-эпидемиологического исследования. Акушерство и гинекология. 2019; 9: 82-6. https://dx.doi.org/10.18565/aig.2019.9.82-86. [Nazarova A.O., Malyshkina A.I., Nazarov S.B.Risk factors for spontaneous preterm birth: results of a clinical and epidemiological study. Obstetrics and gynecology. 2019: 9. 82-6. https://doi:10.18565/aig.2019.9.82-86. (in Russian)].
- Суплотова Л.А., Шарухо Г.В., Ковальжина Л.С., Макарова О.Б. Социально-гигиенический мониторинг в реализации региональной стратегии профилактики йодного дефицита. Гигиена и санитария. 2019: 98(2): 225-30. https://dx.doi.org/10.18821/0016-9900-2019-98-2-225-230. [Suplotova L.A.,Sharukho G.V., Kovalzhina L.S., Makarova O.B. Socio-hygienic monitoring in the implementation of the regional strategy for the prevention of iodine deficiency. Hygiene and sanitation. 2019: 98(2): 225-30. https://doi:10.18821/0016-9900-2019-98-2-225-230. (in Russian)].
- Маринкин И.О., Соколова Т.М., Кулешов В.М., Макаров К.Ю.,Кондюрина Е.Г., Зеленская В.В., Усова А.В. Анализ образа жизни, питания и социально-гигиенических факторов в развитии нарушений беременности. Journal of Siberian Medical Sciences. 2019; 2: 4-17. https://doi:10.31549/2542-1174-2019-2-4-17. [Marinkin I.O., Sokolova T.M., Kuleshov V.M., Makarov K.Yu., Kondyurina E.G., Zelenskaya V.V., Usova AV. Analysis of lifestyle, nutrition and socio-hygienic factors in the development of pregnancy disorders. Journal of siberian medical sciences. 2019: 2. 4-17. https://doi:10.31549/2542-1174-2019-2-4-17. (in Russian)].
Received 13.12.2019
Accepted 07.02.2020
About the Authors
Alla O. Nazarova, PhD, Associate professor of the department of obstetrics and gynecology, medical genetics, State Budgetary Educational Institution of higher education «Ivanovo State Medical Academy» Ministry of Health of the Russian Federation. Tel.: +7(902)746-60-00. E-mail: aonazarova02@gmail.com.153000, Ivanovo, Sheremetevsky Ave., 8, Russia.
Anna I. Malyshkina, Doct. of Med. Sci., Professor, Director, Federal State Budgetary Institution “Ivanovo Research Institute of Maternity and Childhood named
after V.N. Gorodkov” Ministry of Health of the Russian Federation, Head of the Department of obstetrics and gynecology, medical genetics, State Budgetary Educational Institution of higher education «Ivanovo State Medical Academy» Ministry of Health of the Russian Federation. Tel.: +7(4932)33-62-63. E-mail: ivniimid@inbox.ru.
153045, Ivanovo, Pobedy st., 20, Russia; 153000, Ivanovo, Sheremetevsky Ave., 8, Russia.
Sergey B. Nazarov, Doct. of Med. Sci., Professor, assistant Director on science, Federal State Budgetary Institution “Ivanovo Research Institute of Maternity and Childhood named after V.N. Gorodkov” Ministry of Health of the Russian Federation, phone: 8902-317-68-11; Head of the department of normal physiology, State Budgetary Educational Institution of higher education «Ivanovo State Medical Academy» Ministry of Health of the Russian Federation. Tel.: +7(902)317-68-11. E-mail: ivniimid@inbox.ru.
153045, Ivanovo, Pobedy st., 20, Russia; 153000, Ivanovo, Sheremetevsky Ave., 8, Russia.
Elena L. Вoyko, Doct. of Med. Sci., Senior Researcher, Department of Obstetrics and Gynecology, Federal State Budgetary Institution “Ivanovo Research Institute of Maternity and Childhood named after V.N. Gorodkov” Ministry of Health of the Russian Federation.
Tel.: +7(4932)93-84-48; +7(4932)33-62-56. E-mail: Dr-Boyko@mail.ru. 153045, Ivanovo, Pobedy st., 20, Russia.
For reference: Nazarova А.О., Malyshkina А.I., Nazarov S.B., Boyko E.L. Risk Factors for Threatened Preterm Labor: a Clinical and Epidemiological Study.
Akusherstvo i Ginekologiya / Obstetrics and Gynecology. 2020; 6: 43-48 (in Russian)
https://dx.doi.org/10.18565/aig.2020.6.43-48