Analysis of perinatal outcomes and maternal morbidity associated with vacuum-assisted vaginal delivery
Aim. To compare early neonatal and postpartum complications in puerperal women after vacuum-assisted vaginal delivery using various vacuum extractor systems.Kaganova M.A., Spiridonova N.V., Kaganova T.I., Syresina S.V., Devyatova O.O., Galkina D.A., Golovina O.N.
Materials and methods. We conducted a prospective analysis of birth data and child’s medical records of patients who were admitted to maternity wards of the N.I. Pirogov Samara City Clinical Hospital No. and underwent vacuum-assisted vaginal delivery using a Kiwi vacuum system. The historical control group comprised 34 patients who underwent vacuum-assisted vaginal delivery using a reusable Silc cup vacuum extractor with a silicone cup. The groups were comparable. The indication for vacuum-assisted vaginal delivery in all cases was fetal distress.
Results. The study group had shorter delivery time, lower episiotomy rate, a lower rate of transfers of the newborns to the next stage of nursing, lower perineal injury rate, and shorter hospital stay.
Conclusion. Vacuum-assisted delivery using Kiwi disposable vacuum extractors does not increase the risk of early neonatal and postpartum complications compared with reusable silicone cups.
Keywords
Operative vaginal delivery is an integral part of obstetrics aimed at improving perinatal outcomes and reducing cesarean section (CS) rates in patients with non-obstetric comorbidities, who need to minimize active maternal pushing efforts. The second stage of labor can be completed by forceps-assisted or vacuum-assisted deliveries, depending on the clinical situation and indications. According to the literature, the operative vaginal delivery rates have remained stable at between 10% and 13% in the UK (RCOG, 2011); in Russia in 2017, this figure barely reached 6%, and 4.5% of them are vacuum-assisted vaginal deliveries [1, 2]. Such low operative vaginal delivery rates may be attributed to a groundless assumption of obstetrician-gynecologists about a high risk of fetal injuries associated with forceps-assisted and vacuum-assisted deliveries. However, perinatal mortality and morbidity are more affected by timely diagnosis and delivery, as well as the advances and achievements of neonatology [3].
According to the clinical guidelines “Providing specialized medical care by Operative vaginal delivery in the presence of a live fetus (using obstetric forceps or vacuum extraction or using another obstetric delivery modes) “2017 [4], indications for performing fetal vacuum extraction are: identification of fetal distress or an increase in its severity during the second stage of labor and acute fetal hypoxia with the fetal head in the pelvic outlet, hypotonic uterine action in the second stage of labor.
Vacuum systems differ by the type of vacuum mechanism (conventional vs. hand-held), cup material and rigidity (metal, plastic or silicone), cup shape (mushroom or bell), and whether they are disposable or reusable. These characteristics are thought to affect the efficacy and the profile of adverse outcomes, as reflected in several studies [5, 6]. The need to make an informed choice of a vacuum system taking into account the conditions and contraindications is an important task for the obstetrician. All studies emphasize that adverse fetal outcomes are associated mainly with unsuccessful attempts to attach the cup to the fetal head with multiple cup detachments and conversion to another delivery mode, including CS.
The Kiwi Omnicup Vacuum Delivery System (Clinical Innovations, Murray, USA) system includes a rigid plastic cup with a central connection to the suction catheter. It has a flexible traction wire that can be recessed into a groove on top of the cup, which improves maneuverability within the vagina to aid the correct placement of the cup over the fetal flexion point. This design allows it to be used for occipito-anterior, occipito-transverse, and occipito-posterior positions. It incorporates a handheld pump, which eliminates the need for a separate electric pump, increases the mobility of the device, and, accordingly, reduces the time from the moment a decision is made to the moment the intervention is performed. This device is a disposable instrument, which may help reduce the potential transmission of infections.
Standard reusable Silc 50 and 60 mm silicone cups for vacuum extraction have a one-piece design with a slow-moving handle and a suction pump (hose) with a groove on the cup for rotation control. A stationary vacuum aspirator or a hand-held vacuum pump can be used for creating a vacuum. The second option is preferable due to better mobility of the device. The hand-held pump is designed to create a negative pressure up to 80 kPa (0.7–0.8 atm) or 550 mmHg. The angle for traction depends on the fetal head position relative to the plane of the maternal pelvis.
However, there is some evidence that the Kiwi system has a higher rate of detachment compared to other reusable silicone cups [1, 2]. Conventional reusable cups have a larger diameter (60 mm) compared to Kiwi cups (50 mm). Accordingly, the likelihood of detachment is higher for a cup with a smaller diameter, but such cups also cause less damage to the fetal scalp, because a smaller volume of soft tissue gets into the cup when a negative vacuum is applied, which in this case interests us the most. Both devices are designed to create a similar negative pressure of about 600 mmHg. According to the literature, given proper technique of vacuum-assisted vaginal delivery, the mean traction force is 9 kg/m2, which is sufficient for standard operation; vacuum deliveries rarely require a maximum allowable traction force of 14 kg/m2.
This study aimed to compare early neonatal and postpartum complications in puerperal women after vacuum-assisted vaginal delivery using various vacuum extractor systems.
Materials and methods
In this study, we conducted a prospective analysis of birth data and child’s medical records of patients who were admitted to maternity wards of the N.I. Pirogov Samara City Clinical Hospital No. and underwent vacuum-assisted vaginal delivery. Maternity wards are part of a multidisciplinary hospital and belong to the second group of care, where, on average, about 4000 births occur annually. The structure of surgical interventions is presented in the figure and corresponds to the general structure of surgical interventions of maternity wards of the second level of obstetric care in the Russian Federation. The graph shows that the rate of forceps delivery is minimal, averaging 0.1%, which represents isolated cases throughout the study period; the CS rate increased by almost 3% (from 24.5 to 27.1%), and vacuum-assisted delivery rate over four years fluctuated around 1%. Encouraging for us was a decrease in perinatal mortality among full-term infants in 2018. Accordingly, the total operative vaginal delivery rate remains low compared with European countries and the USA.
To perform a comparative analysis, we formed two groups: group 1 consisted of 44 patients, who underwent vacuum-assisted delivery using a disposable Kiwi system, and group 2 comprised 34 patients who underwent vacuum-assisted delivery using a reusable Silc cup vacuum extractor with a silicone cup.
The indication for vacuum-assisted vaginal delivery in all cases was fetal distress according to cardiotocography (CTG). CTG was performed using the Sonicaid Team Care device by the generally accepted method. The diagnosis of intrapartum fetal distress was based on the FIGO consensus guidelines [7]. The diagnosis of fetal intranatal distress was made based on the appearance of repeated late decelerations with the amplitude of more than 45 bpm or variable decelerations of more than 60 beats, lowering the basal rhythm to 100 bpm and lower. The vacuum extractor cup was attached when the head was in the pelvic outlet (the fetal head station below +2 relative to the ischial spines). There were no statistically significant differences between the groups in CTG changes.
Exclusion criteria were a uterine scar after cesarean section or conservative myomectomy, the position of the fetal head above the pelvic outlet, occiput posterior fetal position, and extended head insertion options.
We also excluded from the analysis all patients with obstetric and non-obstetric comorbidities that could affect the condition of the fetus: diabetes and gestational diabetes, preterm pregnancy, pre-eclampsia (PE) and chronic placental insufficiency in combination with fetal growth restriction syndrome (FGR), signs of an acute infection, and post-term pregnancy.
Statistical analysis was performed using the Statistica10 statistical package. Quantitative variables showing normal distribution were expressed as means (M) and standard deviation (SD). The normality of the distribution was tested by the Shapiro-Wilk test. Categorical variables were reported by frequencies and percentages and compared by the χ2 test and two-tailed Fisher’s exact test. Differences between groups were analyzed using either Student’s t-test or Mann-Whitney U test, or ANOVA where appropriate. The Spearman test was used for the correlation analysis.
Results
The groups were comparable in age, which averaged 29.36 (5.19) years in group 1and 28.64 (4.39) years in group 2 (t = 0.49; p = 0.52). In both groups, the patients were predominantly primiparous including 36 (81.8%) patients in group 1 and 24 (70.6%) in group 2 (p = 0.20). One-third of women had one previous birth, and only one patient had a third birth (table 1).

According to the ACOG Bulletin (2003), the risk of difficult delivery was increased for women of short stature (less than 150 cm), age greater than 35 years, gestational age greater than 41 weeks, interval between epidural induction and full cervical dilation of greater than 6 hours, fetal station above +2 cm at full cervical dilation, or occiput posterior fetal position. Accordingly, possible risk factors in the groups were subjected to a more thorough analysis to rule out their influence on operative delivery results.
All patients had full-term pregnancy with mean gestational ages of 39.74 (1.02) and 40.05 (0.66) weeks in groups 1 and 2, respectively (t = -1.54; p = 0.12). Gestational age greater than 41 weeks is an additional risk factor for various birth complications, including meconium-stained amniotic fluid, hypotonic uterine action, and fetal distress; therefore, these patients were also excluded. The number of pregnant women with a tendency to post-term pregnancy did not differ significantly between the groups and was 12 (27.3%) and 6 (17.6%, p = 0.41), respectively. One of the risk factors for difficult delivery is short parental stature. In our study, the number of patients with height less than 160 cm did not significantly differ between the groups (6.8% and 5.9%, respectively).
Exclusion criteria also included some somatic comorbidities, for example, diabetes mellitus (DM), chronic arterial hypertension (CAH), which affect fetal compensatory mechanisms. Most often, patients of both groups were diagnosed with chronic pyelonephritis: 7 (15.9%) and 8 (23.5%), p = 0.79, diseases of hepatopancreatoduodenal area: 9 (25.7%) and 4 (13.3%), p = 0.47, maternal chronic infections without exacerbation, such as toxoplasma, cytomegalovirus and herpetic infections: 2 (4.5%) and 4 (11.5%), p = 0, 44 and a history of chlamydial infection: 6 (13.6%) and 3 (8.82%), p = 0.76. Gynecological comorbidities included chronic salpingoophoritis, bartholinitis, disorders of the ovarian-menstrual cycle, but the rates were similar to those in the general population and did not differ between the study groups.
Most often, pregnancy was complicated by acute respiratory diseases (ARI), threatened miscarriage and preterm birth, anemia. Less common were vomiting in pregnancy, placental insufficiency, oligohydramnios or polyhydramnios. Accordingly, the groups were comparable in the rates of comorbidities and pregnancy complications by trimesters.
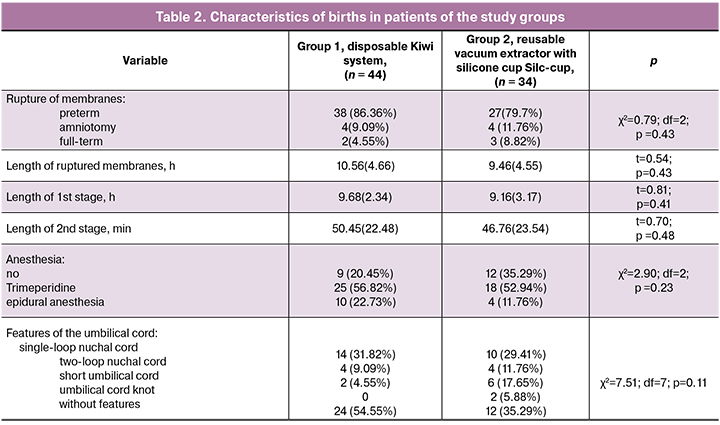
We analyzed the causes of acute fetal hypoxia during labor that required vacuum extraction (Table 2). Noteworthy are high rates of preterm rupture of membranes, both in group 1 (n=38; 86.36%) and group 2 (n = 27; 79.7%). The mean length of ruptured membranes was 10.56 (4.66) and 9.46 (4.55) hours in groups 1 and 2, respectively (t = 0.54; p = 0.43). Ruptured membranes longer than 18 hours were observed in 2 (4.7%) and 4 (11.7%) patients, p = 0.44. The duration of the first and second stage of labor was consistent with the generally accepted ranges and did not significantly differ between the groups. One of risk factors for difficult delivery in the second stage of labor is epidural anesthesia. In our study, the percentage of epidural anesthesia was 22.7% and 11.7% in groups 1 and 2, respectively (p = 0.34). Most commonly, the patients received a narcotic analgesic Trimeperidin, which was used in half of the subjects. Besides, 32 (72.7%) and 21 (61.7%) patients in groups 1 and 2, respectively (p = 0.31) were administered an oxytocin infusion to increase the strength of the contractions or for labor induction.
One of the criteria for unfavorable outcomes of vacuum-assisted delivery is cup detachments. Cup detachment rates were comparable in both groups and amounted to 6 (13.6%) in group 1 and 5 (14.7%) in group 2, p = 0.96. All vacuum-assisted deliveries were effective; there was no conversion to other delivery modes. The total vacuum extraction time was statistically significantly shorter in group 1: 6.20 (2.20) min versus 7.62 (2.28) min in group 2 (U = 472.50; Z = -2, 77; p = 0.005). There were no significant differences in the number of tractions the groups: 3.09 (1.07) in group 1 and 3.76 (1.41) in group 2 (U = 554.50; Z = -1.94; p = 0.05). All three parameters were significantly correlated with each other: the strongest was the correlation between the vacuum extraction time and the number of tractions (r = 0.88), followed by the correlation between the vacuum extraction time and the number of cup detachments (r = 0.46). The number of traction and slippage had a weaker correlation (r = 0.40); there was a significant positive correlation of the number of cup detachments the fetal body mass (r = 0.54), which is understandable because the large size of the fetus contributes to difficulties of delivery.
The most interesting results were obtained for perinatal outcomes. The type of vacuum extractor used during delivery did not affect the severity of fetal asphyxia and the first neonatal assessment by Apgar score (6.91 (0.29) and 6.59 (1.10), U = 636; Z = 1, 12; p = 0.26); however, the second Apgar score was statistically significantly higher in group 1 (8.23 ± 0.52) than in group 2 (7.58 ± 1.05) (U = 437; Z = 3.12; p = 0.001 )
All infants had transient cosmetic defects. In group 1, a “chignon” was observed - the scalp imprint of a rigid cup of a vacuum extractor. Infants in group 2 had ecchymoses and bruising from the cup. Scalp abrasions, lacerations, bruises, and cyanosis were noted in 5 (11.36%) and 10 (24%) cases in groups 1 and 2, respectively (p = 0.08). A pronounced caput succedaneum was observed in 16 (36.4%) and (55.8%) neonates groups 1 and 2, respectively, p = 0.08. At the same time, the cephalohematoma rate was significantly higher in group 2 (n = 18; 52.9%) than in group 1 (n = 12; 27.3%), p = 0.03. No scalp wounds and intracranial hemorrhages were observed in our study; there were 2 cases of subgaleal hematomaы in group 2 (5.8%, p = 0.18); however, the differences were not statistically significant due to the low rates of this complication. Subgaleal hematomas occurred in patients with a large caput succedaneum, a pronounced configuration of the head, and were associated more with prelabor rupture of membranes and hypotonic uterine action. Cup detachments were observed in the same cases.
Indirect and combined effects of vacuum-assisted delivery included brachial plexus injury and clavicle fracture associated with shoulder dystocia. Clavicle fracture rates were similar in both groups, and there was one case of facial nerve paresis group 2.
One of the complications associated with vacuum-assisted delivery is neonatal jaundice (3–30%) [8]. The rates of neonatal jaundice, muscular dystonia syndrome, and cerebral ischemia did not depend on the type of vacuum extractor, but were associated with a newborn’s condition at birth, Apgar score, and, accordingly, the severity of asphyxia. In group 1, the adaptation and recovery time was shorter, and the mean length of hospital stay of newborns discharged home was 4.77 (1.36, from 3 to 8 days) and 4.85 days (2.06, from 4 to11 days) in groups 1 and 2, respectively. Five (11.3%) newborns were transferred to the second stage of nursing, which was twice less than in group 2 - 11 (32.3%), p = 0.04 (Table 3).

Since the diameter and height of Kiwi cups are smaller than that of standard silicone cups, the episiotomy rate in group 1 (38.64%) was almost twice lower than in group 2 (64.70%), p = 0.03. Vaginal and perineal tear rates, as well as clinically significant hematomas (with severe anemia and blood transfusion), were similar in both groups. Patients in group 2 had a higher percentage of postpartum hematometra than that in group 1- 2 (4.55%) versus 8 (23.53%), p = 0.01.
Discussion
Vacuum-assisted delivery has established itself as a safe delivery mode given the conditions, indications, and contraindications are observed. Various devices for vacuum extraction have their pros and cons. Thus, there is some evidence that the Kiwi system has a higher rate of detachment (9.6%) compared to reusable silicone cups (0.7%) [2, 5, 9]. However, our results did not show significant differences. This absence of differences and intervention failure is associated with the study inclusion criteria (vacuum-assisted delivery was performed with the fetal head stations below +2).
Another factor limiting the use of vacuum extraction is the increased risk of maternal and fetal injury. Fetal injuries during instrumental vaginal delivery are divided into two categories. The first includes injuries associated with hypoxia and ischemia, and the second is mechanical injuries, which, in turn, are divided into extracranial, cranial and intracranial. Separately, as a variant of the norm, cosmetic injuries related to using vacuum extractors are distinguished, which are found in 100% and are cup imprints, bruising, or the so-called “chignon,” which is characteristic of Kiwi system. Clinically insignificant injuries include retinal hemorrhage (1–29%), superficial abrasion (2–10%), subcutaneous hematoma and cephalohematoma (6–11%) [8, 10]. Clinically significant to fetal head injuries include scalp wounds, subgaleal hematoma (0.5-1%), subarachnoid hemorrhage (0.8%), and the rarest complication for vacuum extraction is skull bone fractures (< 0.1%) [10]. In our study, cosmetic defects were observed in almost all newborns, but they did not have clinical significance. The cephalohematoma was observed in 52% and 27% of patients in group 2 and 1, respectively, which was the reason for a longer hospital stay. For comparison, according to the literature, cephalohematoma rates during natural childbirth and forceps-assisted delivery is 4.6% and 34.6%, respectively [6].
According to reviews [11–13], the rate of subgaleal hematomas associated with vacuum-assisted delivery is 1.5% and is a serious complication with a high percentage (25%) of newborn mortality. According to the review by Vacca A. [8], the formation of subgaleal hematomas does not depend on the type of cup (rigid or soft), which is generally consistent with our study.
In the postpartum period, a hematometra was observed more often in group 2 than in group 1, which we attribute to a change in uterine contractile activity in the postpartum period in response to the use of more voluminous cups and, consequently, resulting in greater likelihood of injury to the cervix, upper and the middle third of the vagina, which has a reflex effect on the subsequent uterine contractile activity.
Conclusion
Vacuum-assisted delivery using Kiwi disposable vacuum extractors allows a more gentle delivery and reduces the risk of both maternal (episiotomy, hematometra) and neonatal (cephalohematoma, subgaleal hematoma, the need to transfer to the next stage of nursing) morbidity. When vacuum extraction is performed with the fetal head within the pelvic outlet and lower, the risks of the vacuum extraction failure and cup detachment are minimal for both disposable rigid cups (Kiwi system) and reusable silicone cups. Moreover, the operative vaginal delivery time is significantly shorter for disposable cups, which is important for deliveries for fetal distress. The unique advantage of Kiwi cups is their mobility, low risk of infection, and low invasiveness. To conclude, vacuum-assisted delivery using the Kiwi vacuum extractor with the fetal head station below +2 relative to the ischial spines is a safe, effective delivery mode that is free from the disadvantages such as traction failure and cup detachment.
References
- Черненков Ю.В., Нечаев В.Н., Кушеков Ф.А. Особенности состояния здоровья новорожденных после родоразрешения методом вакуум-экстракции плода. Саратовский научно-медицинский журнал. 2017; 13(3): 498-501.[Chernenkov Yu.V., Nechaev V.N., Kushekov F.A. Health status of newborns after vacuum extraction. Saratovskij nauchno-medicinskij zhurnal. 2017; 13(3): 498-501. (In Russian)]. eLIBRARY ID: 32484231
- Медведева И.Н., Святченко К.С., Барбашова Ю.Ю. Вакуум-экстракция плода: версии и контраверсии. Журнал акушерства и женских болезней. 2017; 66(1): 21-26. [Medvedeva I.N., Svyatchenko K.S., Barbashova Y.Y. Acuum extraction of the fetus: the version and controversy. Journal of Obstetrics and Women’s Diseases. 2017; 66(1): 21-26. (In Russian)]. doi: 10.17816/JOWD66121-26
- Петрухин В.А., Ахвледиани К.Н., Логутова Л.С., Иванкова Н.М., Мельников А.П., Чечнева М.А., Башакин Н.Ф., Коваленко Т.С., Реброва Т.В. Вакуум-экстракция плода в современном акушерстве. Российский вестник акушера-гинеколога. 2013; 6: 53-59. [Petrukhin V.A., Akhvlediani K.N., Logutova L.S., Ivankova N.M., Mel’nikov A.P., Chechneva M.A., Bashakin N.F., Kovalenko T.S., Rebrova T.V. Fetal vacuum extraction in modern obstetrics. Rossijskij vestnik akushera-ginekologa. 2013; 6: 53-59.(In Russian)].
- Клинические рекомендации «Оказание специализированной медицинской помощи при оперативных влагалищных родах при наличии живого плода (с помощью акушерских щипцов или с применением вакуум-экстрактора или родоразрешение с использованием другого акушерского пособия)». М., 2017. [Klinicheskie rekomendacii «Okazanie specializirovannoj medicinskoj pomoshhi pri operativnyh vlagalishhnyh rodah pri nalichii zhivogo ploda (s pomoshh’ju akusherskih shhipcov ili s primeneniem vakuum-jekstraktora ili rodorazreshenie s ispol’zovaniem drugogo akusherskogo posobija)» M., 2017.(In Russian)].
- Harlev A., Fatool S.K., Sergienko R., Sheiner E. Non-progressive labor in the second stage leading to vacuum extraction is a risk factor for recurrent non-progressive labor. Arch. Gynecol Obstet. 2017; 295(6): 1393-8. DOI: 10.1007/s00404-017-4359-z
- Weissbach T., Hag-Yahia N., Ovadia M., Tzadikevitch Geffen K., Weitzner O., Biron-Shental T. Kiwi OmniCup Handheld vs. Mityvac M-Style conventional vacuum system: a retrospective observational study. J. Matern. Fetal Neonatal Med. 2017; 17: 1-8. Available at: http://www.tandfonline.com/loi/ijmf20
- Ayres-de-Campos D., Spong C.Y., Chandraharan E.; FIGO Intrapartum Fetal Monitoring Expert Consensus Panel. FIGO consensus guidelines on intrapartumfetal monitoring: Cardiotocography. Int. J. Gynaecol. Obstet. 2015; 131(1): 13-24. https://doi.org/10.1016/j.ijgo.2015.06.020
- Vacca A. Handbook of vacuum delivery in obstetric practice. 2nd ed. Brisbane: Vacca Research; 2003
- Royal College of Obstetricians and Gynaecologists. Operative vaginal delivery. Green-top Guideline No. 26. January 2011.
- O’Mahony F., Hofmeyr G.J., Menon V. Instruments for assisted vaginal delivery. Cochrane Database Syst. Rev. 2010; (11): CD005455.http://dx.doi.org/10.1002/14651858.CD005455.pub2
- Ekéus C., Wrangsell K., Penttinen S., Åberg K. Neonatal complications among 596 infants delivered by vacuum extraction (in relation to characteristics of the extraction). J. Matern. Fetal Neonatal Med. 2018; 31(18): 2402-8. https://doi.org/10.1080/14767058.2017.1344631
- Muraca G.M., Sabr Y., Lisonkova S., Skoll A., Brant R., Cundiff G.W., Joseph K.S. Perinatal and maternal morbidity and mortality after attempted operative vaginal delivery at midpelvic station. CMAJ. 2017; 189(22): E764-72.https://doi.org/10.1503/cmaj.161156
- Власюк В.В. Родовая травма и перинатальные нарушения мозгового кровообращения. СПб.: Нестор-История, 2009. 252 с. [Vlasjuk V.V. Rodovaja travma i perinatal’nye narushenija mozgovogo krovoobrashhenija.SPb.: Nestor-Istorija, 2009. 252 s (In Russian)]. ISBN:978-5-98187-373-7
Received 22.05.2019
Accepted 21.06.2109
About the Authors
Maria A. Kaganova, candidate of medical sciences, docent of the Department of Obstetrics and Gynecology of the Institute for Improvement of Physicians, Samara State Medical University, Ministry of Health of Russia. ORCID: 0000-0001-5879-418x 443100, Russia, Samara, Polevaya str. 80. Tel.: +78462071968. E-mail: mkaganova@yandex.ruNatalya V. Spiridonova, doctor of medical sciences, professor, head of the Department of Obstetrics and Gynecology of the Institute for Improvement of Physicians,
Samara State Medical University, Ministry of Health of Russia. ORCID: 0000-0003-3928-3784 443100, Russia, Samara, Polevaya str. 80.
Tel.: +78462071968. E-mail: nvspiridonova@mail.ru
Tatyana I. Kaganova, professor, head of the Department of Pediatrics of the Institute for Improvement of Physicians, Samara State Medical University,
Ministry of Health of Russia. 443100, Russia, Samara, Chapaevskaya str. 89. Tel.: +78462600812. E-mail: t.kaganova2010@yandex.ru
Svetlana V. Syresina, head of 21 maternity wards, obstetrician-gynecologist, GBUZ SGKB No. 1 named after N.I. Pirogov. Tel .: +7 (846) 2071949.
E-mail: svetlana.syresina@yandex.ru 443100, Russia, Samara, ul. Field, d. 80.
Olga O. Devyatova, Doctor obstetrician-gynecologist, N.I.Pirogov Sity clinical hospital №1.443100, Russia, Samara, Polevaya str. 80. Tel.: +78462071949.
E-mail: dewyatowa.olya@yandex.ru
Daria A. Galkina, doctor obstetrician-gynecologist, N.I.Pirogov Sity clinical hospital №1. 443100, Russia, Samara, Polevaya str. 80. Tel.: +78462071949.
E-mail: darya.golubeva.1992@mail.ru
Olga N. Golovina, doctor obstetrician-gynecologist, N.I.Pirogov Sity clinical hospital №1. 443100, Russia, Samara, Polevaya str. 80. Tel.: +78462071949.
E-mail: doktorola@yandex.ru
For citation: Kaganova M.A., Spiridonova N.V., Kaganova T.I., Syresina S.V., Devyatova O.O., Galkina D.A., Golovina O.N. Analysis of perinatal outcomes and maternal morbidity associated with vacuum-assisted vaginal delivery.
Akusherstvo i Ginekologiya / Obstetrics and gynecology. 2019; 10: 92-9.(In Russian).
https://dx.doi.org/10.18565/aig.2019.10.92-99