Relationship between spontaneous abortion history and treatment outcomes in patients with threatened abortion: a prospective cohort study
Grudnitskaya E.N.
Objective: Identification of relationship between the history of spontaneous abortion (SA) and miscarriage in patients with singleton pregnancy associated with threatened miscarriage (TM) in singleton pregnancy.
Materials and methods: A prospective cohort study was carried out among the patients who were admitted to hospital and underwent treatment due to TM in 2021. The patients were divided into two groups. The exposed group included 97 women with spontaneous abortion history, and the unexposed group comprised 145 women without SA history. Both groups were divided into the subgroups based on the obstetric outcomes – prolongation of pregnancy or SA. The relationship between SA history and miscarriage in cases of threatened abortion, as well as the differences between the clinical and laboratory parameters on the first day of hospitalization due to TM in patients with and without SA history were identified based on the results of comprehensive physical exam.
Results: The women with TM and singleton pregnancy, who had SA history, relative risk of adverse pregnancy outcome, particularly termination of pregnancy was 3.3 (95% CI 1.2–9.2), р=0.018, that contributed to the increased number of cases of habitual abortion (HA). The incidence rate of SA in the cohort was 6.6%. All patients with TM (in the exposed and unexposed groups) had latent iron deficiency characterized by the median ferritin level below 30 μg/L. Double increase in the frequency of hypothyroidism detection in patients with previous SA (OR 2.0; 95% CI 0.9–4.3; p=0.073) did not reach statistical significance of the obtained results.
Conclusion: Given that in pregnant women with the diagnosis of threatened miscarriage, who previously experienced SA, relative risk of recurrent miscarriage is 3.3-fold higher, that can lead to habitual abortion, it is necessary that the patients with the burdened anamnesis should be carefully monitored. Particularly, it is necessary to develop and closely monitor management strategy for these women during the pregravid preparation, that is highly important for reducing the risk.
Conflicts of interest: The author has no conflict of interest to declare.
Funding: The study was carried within the State program of scientific researches of the Republic of Belarus “Translational medicine”, assignment No. 3.47 «To develop the method of preventive healthcare for spontaneous abortions and preterm births in pregnant women with connective tissue dysplasia”, state registration No. 20220318, implementation term 01.01.2022–31.12.2024.
Gratitude: The author of the article expresses gratitude to S.L. Voskresensky, Professor, MD, for consultations in planning this study.
Ethical Approval: The study was approved by the Ethics Committee of Belarusian Medical Academy of Postgraduate Education" (Protocol No. 1 of February 06, 2020).
Patient Consent for Publication: The patients have signed informed consent for publication of the obtained data.
Author's Data Sharing Statement: The data supporting the findings of this study are available on request from the author.
For citation: Grudnitskaya E.N. Relationship between spontaneous abortion history and
treatment outcomes in patients with threatened abortion: a prospective cohort study.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2025; (11): 77-85 (in Russian)
https://dx.doi.org/10.18565/aig.2025.203
Keywords
Reproductive losses are a significant problem in modern obstetrics [1–3]. In all registered pregnancies the overall risk of miscarriage is 15/3% (95% CI 12.5– 18.7%) [1]. According to the available data, threatened abortion (TA), also called threatened miscarriage (TM) is a cause of hospitalization of 15% of all pregnant women in the Republic of Belarus annually, and this is a significant medical and social issue. Pregnancy outcome associated with TM is spontaneous abortion (SA), and it depends on several factors. The immediate cause of spontaneous expulsion of an embryo from the uterus is a suboptimal embryo or less than ideal maternal environment. The events happening in early pregnancy have a significant impact on pregnancy outcome. A series of currently published research papers reported relationship between spontaneous abortion and reproductive complications in future [4–7]. In the existing literature, there is no information about the influence of previous spontaneous abortions on treatment effectiveness in women, who experienced TM. The data on the impact of SA history on treatment outcomes in women with TM are important, since habitual miscarriage (HM) is diagnosed in pregnancies complicated by threatened miscarriage and results in spontaneous abortion in patients with previous SA history. Knowing past history of miscarriages is very important for successful treatment of women with TM. This will help improve the effectiveness of medical care, pregravid preparation, the diagnosis and treatment of women planning pregnancy, since recurrent miscarriages indicate potential problems requiring careful attention and specialized approach to planning and management of subsequent pregnancies. Information on the impact of previous SA on the outcome of treatment of threatened miscarriage will help the specialists to improve effectiveness of risk assessment and indicate optimal treatment aimed at preserving future pregnancies.
Materials and methods
This prospective cohort study included 520 patients, who were admitted to the clinical maternity hospital of the Mink region in the Republic of Belarus during 2021 with the diagnosis of “threatened abortion” (ICD-10 code O20.0).
Inclusion criteria in the study for the patients with TA were based on definitions in the Queensland Guidelines [8] and the Clinical Protocol No. 17 of the Ministry of Health of the Republic of Belarus [9]: the clinical signs of chorionic separation (vaginal bleeding); and/or ultrasound signs (retrochorial hematoma).
Inclusion criteria in the cohort of women were the following: age from 18 to 49 years; singleton pregnancy; pregnancy before 21 weeks; threatened abortion. Inclusion criterium in the exposed group was SA history. Inclusion criterium in the unexposed group was absence of SA history.
Exclusion criteria were the following: multiple pregnancy; embryonic death; hydatidiform mole; ectopic pregnancy; heterotopic pregnancy (ectopic and intrauterine pregnancy); pregnancy of unknown location; prenatal diagnosis of congenital malformations; induced abortion history; artificial termination of pregnancy for medical indications; habitual abortion; refusal to answer the questions and undergo medical or instrumental examination; the presence of factors that increased the risk for a woman or prevented fulfilment of the conditions of the study, or prevented its completion.
Time at Risk (TaR) for each patient began from the start date of inclusion in the study and diagnosing TA, and ended with occurrence of spontaneous abortion, successful prolongation of pregnancy, or when patient observation was stopped due to achieving the 22nd week of gestation.
The primary outcome explored in the study was the incidence of SA and prolongation of pregnancy in patients with TA in singleton pregnancy. The secondary outcome included the differences between obstetric and gynecological, and general somatic anamnesis, as well as the clinical and laboratory data on the first day of hospitalization due to TA in patients with and without SA history. All women (n=520) were evaluated for their compliance with inclusion criteria in the study: singleton pregnancy, gestational age before 21 weeks inclusively; women’s age from 18 to 45 years. The women were divided into groups based on the presence of absence of SA history. The exposed group included women with SA history (n=97), and the unexposed group comprised women without SA history (n=145). Based on the obstetric outcomes – prolongation of pregnancy or SA, both groups were divided into two subgroups. During observation of the cohort, 278 patients were excluded from the study (Figure).

The ethical principles recommended by the Declaration of Helsinki on ethical principles for medical research involving human participants of the World Medical Association (1964, revised in October 2013 in Brazil) were observed during the study. The study was approved by the Ethics Committee of Belarusian Medical Academy of Postgraduate Education" (Protocol No. 1 of February 06, 2020) in the frames of scientific research work on the topic “To develop the method of preventive healthcare for spontaneous abortions and preterm births in pregnant women with connective tissue dysplasia”
The clinical and instrumental research methods were used, including anamnesis collection and investigation of complaints, general medical and gynecological examination.
Menstrual function was evaluated according to the FIGO recommendations (2011, revised in 2018) [10, 11]. The criteria for normal parameters were: menstrual cycle length – 24–38 days; the length of a period – 3–8 days; menstrual blood loss per 1 menstrual cycle – 5–80 mL.
On the first day of hospital stay, venous blood was collected for biochemical and general clinical blood tests. Serum samples were obtained from venous blood collected from patients’median cubital veins by venipuncture in the morning on an empty stomach in accordance with the guidelines for collecting venous blood samples [12, 13], and were immediately analyzed after obtaining. Cytological examination of the scrapings from the cervical surface and cervical canal was performed to detect the presence of atypia.
Statistical analysis
The following data were used for measuring the cohort size: the significance level (1-α) – 95%; power of the study – 80%; the ratio of the size of the unexposed group to the size of the exposed group in the cohort – 1; the rates of outcomes in the unexposed group – 15%; relative risk – 2. Kelsey’s formula was used to calculate the sample size. The sizes of the exposed and unexposed groups were 97 and 145 women, respectively, a total of 242 women. The sampling was done using continuous method.
Statistical data processing was performed on PC with Windows 8.1 using software programs Microsoft Excel, Statistica 10 (Version 6-Index, StatSoft Inc., USA, licence No. AXXR012E829129FA), MedCalc 15.8 (MedCalc Software, Belgium). The sample size was calculated using software program Epi InfoTM (Version 7.2, Web site: https://www.cdc.gov/epiinfo/index.html).
The Shapiro–Wilk test (W-test) was used to test the normality of distribution of the obtained data. were described as The arithmetic mean (M) and standard deviation (SD) were used to describe the quantitative data in the normal distribution The median and interquartile range – Me (Q1; Q3) were used to describe the quantitative data when distribution was non-normal. Fisher's exact test was used to test the equality of variances before using the parametric statistical methods. The quantitative data with the normal distribution in the groups were compared with assumption of equal variances using Student's t-test. In the absence of normal distribution, the Mann–Whitney U test was used to assess the statistical significance between two independent samples Absolute values and percentage were used to describe the categorical data. The qualitative parameters were presented as absolute values and %. Pearson’s chi-square test (χ2) was used to assess statistical significance of the differences. Fisher's exact test (the two-tailed test) was used when the expected number of observations in any cell in the 2×2 contingency table was less than 5. The odds ratio (OR) and statistical significance were estimated with the 95% confidence interval. The Wilson method was used to calculate the confidence interval for a proportion.
Based on the OR the conclusion was made, whether there is relationship between the explored outcome and the risk factor. When OR was equal to 1, this indicated that the risk factor did not influence the development of the disease. When OR was greater than 1, the explored risk factor increased the probability of developing the disease. With greater value of OR the risk was higher. When OR was less than 1, the risk factor conversely reduced the probability of developing the disease. Relative risk was calculated with 95% confidence interval to assess relationship between the risk factor (SA history) and pregnancy outcome (SA). In hypotheses testing, the differences were considered statistically significant at р<0.05.
Results and discussion
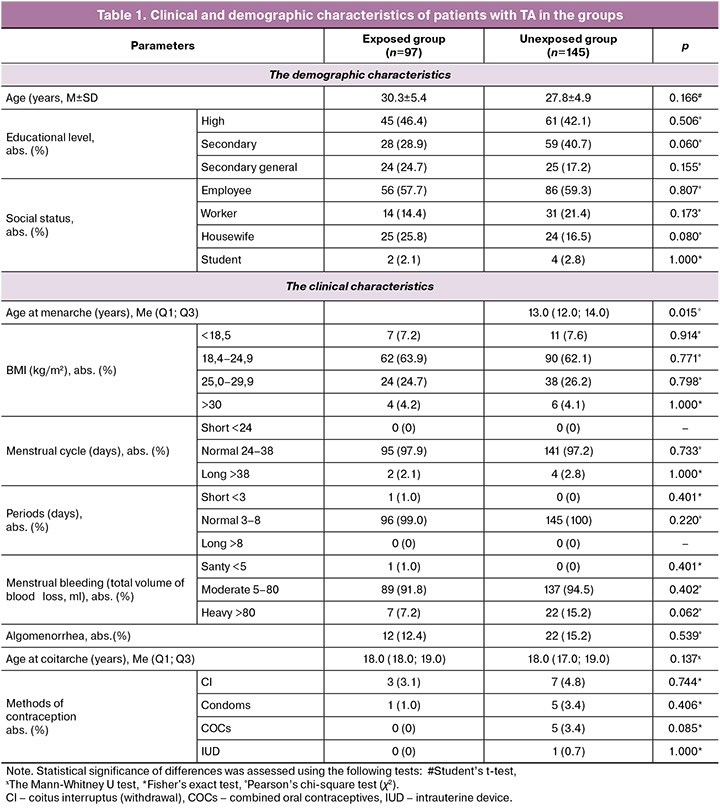
The mean age of patients with TA enrolled in the study (n=242) was 28.8 (5.3) years. The minimum age was 18.0 years, and the maximum age was 45 years. In the cohort of women, who were hospitalized due to TA, most patients were of early reproductive age (18–35 years) – 85.1% (206/242), and 14.9% (36/242) of women were of late reproductive age (>35–49 years). After completion of observation all patients with threatened abortion (n=242) were divided into 2 groups: the exposed group included the patients with SA history (n=97), the unexposed group comprised women without SA history (n=145). The clinical and demographic characteristics are presented in Table 1.
The clinical and anamnestic characteristics of the groups with gynecological and somatic diseases is represented in Table 2.

Comparative analysis found no statistically significant differences in the key indicators between the groups in assessment of balance in the baseline clinical and demographic characteristics. Thus, the age and social status of patients were comparable between the groups in the study. No relationship was found between gynecological or somatic anamnesis in women with TA and without SA history. At the same time, in this study, the probability of hypothyroidism (ICD-10 code E03) detection in patients with previous SA was two times higher than in women without SA history (OR 2.0; 95% CI 0.9–4.3; р=0.073). However, the difference was not statistically significant. According to scientific publications, the prevalence of hypothyroidism among women who experienced miscarriage may reach 48.4% [14]. Hypothyroidism can increase the risk of miscarriage (OR 4.96; 95% CI 2.76–8.90; р<0.001) [15]. Timely medical interventions help reduce the frequency of miscarriages [16], that should be taken into account in pregravid preparation in patients with SA history.
On the first day of hospitalization, all women in the observed cohort underwent the general clinical blood tests. The results are presented in Table 3.

In the exposed group, white blood cells (WBC) was significantly lower versus the unexposed group. The median WBC count in both groups was within the reference range. Analysis of other hematological parameters of the general blood test in patients with TA in the exposed and unexposed groups showed that the median values of the studied parameters were also within the reference intervals, and no statistically significant differences were found between them in the groups (p>0,05).
The results of intergroup comparison of biochemical parameters of blood serum in patients with TA in the exposed and unexposed groups are presented in Table 4.
AST concentrations in patients with SA history were significantly lower than in patients without SA history. It should be noted that the median values in both groups were within the normal range. Analysis of other biochemical parameters of blood serum in patients with TA showed that all parameters were within the reference ranges, and no statistically significant differences were found between the patients with and without SA history (p>0.05). At the same time, in all women hospitalized due to TA, the medians of ferritin concentrations were within the lower reference limit – 20.1 (17.2; 27.8) µg/L in patients in the exposed group and 21.0 (16.8; 22.4) µg/L in the unexposed group. According to the WHO, timely identification of iron deficiency in early pregnancy is extremely important for a favorable outcome of pregnancy. Ferritin level <15 µg/L may indicate iron deficiency in future mothers [17]. According to the Resolution No. 23 of April 01, 2022 of the Ministry of Health of the Republic of Belarus, one of the diagnostic signs of latent iron deficiency (ICD-10 Е61.1) is reduced serum ferritin levels (<30 µg/L). This normative act established serum ferritin thresholds of less than 30 µg/L as a significant indicator of latent iron deficiency in patients [18]. Our study found that all women who experienced threatened miscarriage had iron deficiency. This fact is of particular significance in the context of physiological demands of the body during pregnancy. The obtained data are consistent with the results of the study by Radzinsky V.E. et al. (2016), who reported that iron deficiency was associated with threatened miscarriage in every third woman, and was a cause of placental insufficiency and perinatal complications [19].
The results of cytological examination of the scrapings from the cervical surface and cervical canal for the presence of atypical cells found no statistically significant differences between the patients in the exposed and unexposed groups.
Normal cytology results were in 83.5% (81/97) and 77.2% (112/145) of women. The inflammatory type of smear was in 16.5% (16/97) and 22.8% (33/145) of women, respectively (р=0.234, χ2=1.41).
After completion of the cohort observation, the patients in both groups were divided into the subgroups based on the outcome of treatment for TA. The subgroup with SA history and prolonged pregnancy after treatment comprised 86/97 women (88.7%). The subgroup with SA history and spontaneous abortion comprised 11/97 patients (11.3%). The subgroup without SA history and prolonged pregnancy after treatment was formed of 140/145 (96.6%) women, and the subgroup without SA history and spontaneous abortion included 5/145 (3,4%) patients.
Adverse pregnancy outcomes were most often in women who had previous SA history (р=0.018).
The incidence rate of spontaneous abortions in the studied cohort was calculated by formula:

The results of the cohort observation are represented in the 2×2 contingency table (Table 5).
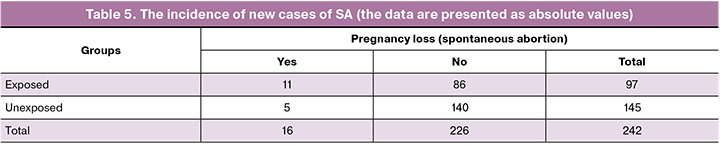
The relative risk was calculated to identify relationship between previous spontaneous abortion and subsequent miscarriage in the presence of threatened abortion. It was found that in patients diagnosed with TA and the burdened history of SA, the probability of adverse pregnancy outcome, namely, pregnancy loss increases by 3.3 times (95% CI 1.2–9.2), р=0.018.
Conclusion
This study identified relationship between SA history and relative risk of miscarriages in women with threatened abortion. In women with TA, who had previous SA history, risk ratio of adverse pregnancy outcome, namely, pregnancy loss was 3.3 (95% CI 1.2–9.2), р=0.018, that contributed to the occurrence of habitual miscarriages. During the study the incidence rate of new cases of SA was 6.6%.
It should be noted that all women enrolled in the study, who experienced threatened miscarriage, had low ferritin levels (<30 µg/L), that indicated latent iron deficiency.
The study found that the probability of hypothyroidism detection in women with previous SA history was 2 times higher compared with those, who had no SA history – 17.5% (17/97) and 9.7% (14/145), respectively. Nevertheless, this difference was not statistically confirmed (OR 2.0; 95% CI 0.9–4.3; р=0.073).
The obtained results indicate the importance of an in-depth analysis of these conditions at the stage of pregnancy planning. Timely prevention strategies and therapy are necessary to improve pregnancy outcomes.
References
- Quenby S., Gallos I.D., Dhillon-Smith R.K., Podesek M., Stephenson M.D., Fisher J. et al. Miscarriage matters: the epidemiological, physical, psychological, and economic costs of early pregnancy loss. Lancet. 2021; 397(10285): 1658-67. https://dx.doi.org/10.1016/S0140-6736(21)00682-6
- Magnus M.C., Wilcox A.J., Morken N.H., Weinberg C.R., Håberg S.E. Role of maternal age and pregnancy history in risk of miscarriage: prospective register based study. BMJ. 2019; 364: l869. https://dx.doi.org/10.1136/bmj.l869
- Deryabin P., Griukova A., Nikolsky N., Borodkina A. The link between endometrial stromal cell senescence and decidualization in female fertility: the art of balance. Cell. Mol. Life Sci. 2020; 77(7): 1357-70. https://dx.doi.org/10.1007/s00018-019-03374-0
- Bearak J., Popinchalk A., Ganatra B., Moller A.B., Tunçalp Ö., Beavin C. et al. Unintended pregnancy and abortion by income, region, and the legal status of abortion: estimates from a comprehensive model for 1990-2019. Lancet Glob. Health. 2020; 8(9): e1152-61. https://dx.doi.org/10.1016/S2214-109X(20)30315-6
- Sun H., Mao J., Su X., Du Q. Impact of spontaneous abortion history and induced abortion history on perinatal outcomes of singleton pregnancies. BMC Public Health. 2023; 23(1): 2360. https://dx.doi.org/10.1186/s12889-023-17264-5
- Studnicki J., Longbons T., Reardon D.C., Fisher J.W., Harrison D.J., Skop I. et al. The enduring association of a first pregnancy abortion with subsequent pregnancy outcomes: a longitudinal cohort study. Health Serv. Res. Manag. Epidemiol. 2022; 9: 23333928221130942. https://dx.doi.org/10.1177/23333928221130942
- Wu C.Q., Nichols K., Carwana M., Cormier N., Maratta C. Preterm birth after recurrent pregnancy loss: a systematic review and meta-analysis. Fertil. Steril. 2022; 117(4): 811-19. https://dx.doi.org/10.1016/j.fertnstert.2022.01.004
- Queensland Clinical Guidelines. Early pregnancy loss. Guideline No. MN22.29-V7-R27. Queensland Health. 2022. Available at: https://www.health.qld.gov.au/qcg
- Постановление Министерства здравоохранения Республики Беларусь от 19.02.2018 № 17 «Об утверждении клинического протокола ʺМедицинское наблюдение и оказание медицинской помощи женщинам в акушерстве и гинекологииʺ». Доступно по: https://pravo.by/document/?guid=12551&p0=W21833049p [Resolution No. 17 of the Ministry of Health of the Republic of Belarus dated February 19, 2018, "On approval of the clinical protocol 'Medical supervision and medical care for women in obstetrics and gynecology'". Available at: https://pravo.by/document/?guid=12551&p0=W21833049p (in Russian)].
- Munro M.G., Critchley H.O., Broder M.S., Fraser I.S.; FIGO Working Group on Menstrual Disorders. FIGO classification system (PALM-COEIN) for causes of abnormal uterine bleeding in nongravid women of reproductive age. Int. J. Gynaecol. Obstet. 2011; 113(1): 3-13. https://dx.doi.org/10.1016/j.ijgo.2010.11.011
- Munro M.G., Critchley H.O.D., Fraser I.S.; FIGO Menstrual Disorders Committee. The two FIGO systems for normal and abnormal uterine bleeding symptoms and classification of causes of abnormal uterine bleeding in the reproductive years: 2018 revisions. Int. J. Gynaecol. Obstet. 2018; 143(3): 393-408. https://dx.doi.org/10.1002/ijgo.12666
- Приложение к приказу Министерства здравоохранения Республики Беларусь от 10.11.2015 № 1123 «Об утверждении Инструкции о порядке организации преаналитического этапа лабораторных исследований». Доступно по: https://minzdrav.gov.by/upload/lcfiles/000128_336854_1123.pdf [Appendix to order No. 1123 of the Ministry of health of the Republic of Belarus dated 10.11.2015 "On approval of the instructions on the procedure for organizing the pre-analytical stage of laboratory research". Available at: https://minzdrav.gov.by/upload/lcfiles/000128_336854_1123.pdf (in Russian)].
- Simundic A., Bolenius K., Cadamuro J., Church S., Cornes M.P., van Dongen-Lases E.C. et al., on behalf of the Working Group for Preanalytical Phase (WG-PRE), of the European Federation of Clinical Chemistry and Laboratory Medicine (EFLM) and Latin American Working Group for Preanalytical Phase (WG-PRE-LATAM) of the Latin America Confederation of Clinical Biochemistry (COLABIOCLI). Joint EFLM-COLABIOCLI Recommendation for venous blood sampling, v 1.1. Clin. Chem. Lab. Med. June 2018. https://dx.doi.org/10.1515/cclm-2018-0602
- Олина А.А. Гипотиреоз и неразвивающаяся беременность. Журнал акушерства и женских болезней. 2018; 67(3): 49-54. [Olina A.A. Hypothyroidism and early fetal demise. Journal of Obstetrics and Women’s Diseases. 2018; 67(3): 49-54 (in Russian)]. https://dx.doi.org/10.17816/JOWD67349-54
- Liu H., Shan Z., Li C., Mao J., Xie X., Wang W. et al. Maternal subclinical hypothyroidism, thyroid autoimmunity, and the risk of miscarriage: a prospective cohort study. Thyroid. 2014; 24(11): 1642-9. https://dx.doi.org/10.1089/thy.2014.0029
- Rao M., Zeng Z., Zhao S., Tang L. Effect of levothyroxine supplementation on pregnancy outcomes in women with subclinical hypothyroidism and thyroid autoimmuneity undergoing in vitro fertilization/intracytoplasmic sperm injection: an updated meta-analysis of randomized controlled trials. Reprod. Biol. Endocrinol. 2018; 16(1): 92. https://dx.doi.org/10.1186/s12958-018-0410-6
- WHO guideline on use of ferritin concentrations to assess iron status in individuals and populations. Geneva: World Health Organization, 2020. Available at: https://www.who.int/publications/i/item/9789240000124
- Постановление Министерства здравоохранения Республики Беларусь от 01.04.2022 № 23 «Об утверждении клинического протокола «Диагностика и лечение пациентов (взрослое население) с железодефицитной анемией». Доступно по: https://minzdrav.gov.by/upload/dadvfiles/CProtokol/КП_Диагностика_и_лечение_пациентов_(взрослое_население)_с_железодефицитной_анемией_пост_МЗ_01_04_2022_№23.pdf [Resolution No. 23 of the Ministry of Health of the Republic of Belarus dated April 1, 2022 "On Approval of the clinical protocol 'Diagnosis and treatment of patients (adult population) with iron deficiency anemia'". Available at: https://minzdrav.gov.by/upload/dadvfiles/CProtokol/КП_Диагностика_и_лечение_пациентов_(взрослое_население)_с_железодефицитной_анемией_пост_МЗ_01_04_2022_№23.pdf (in Russian)].
- Радзинский В.Е., Ордиянц И.М., Побединская О.С. Железодефицитная анемия как фактор риска плацентарной недостаточности и перинатальных осложнений. Акушерство и гинекология. 2016; 12: 125-30. [Radzinsky V.E., Ordiyants I.M., Pobedinskaya O.S. Iron deficiency anemia as a risk factor for placental insufficiency and perinatal complications. Obstetrics and Gynecology. 2016; (12): 125-30 (in Russian)]. https://dx.doi.org/10.18565/aig.2016.12.125-30
Received 28.07.2025
Accepted 05.11.2025
About the Authors
Elena N. Grudnitskaya, PhD, Associate Professor, Associate Professor of the Department of Obstetrics and Gynecology, Institute of Advanced Training and Retraining of Healthcare Personnel, Belarusian State Medical University, 220013, Republic of Belarus, Minsk, P. Brovki str., 3, bldg. 3, +37529560-53-61, grudnickaja@mail.ru,https://orcid.org/0009-0003-5268-4029