Определение вульводинии, признанное еще в 2003 г. Международным обществом по изучению заболеваний влагалища и вульвы (ISSVD), звучит как дискомфорт в области вульвы, который чаще всего описывается, как жгучая боль, возникающая в отсутствии соответствующих видимых или специфических признаков, а также в качестве клинически идентифицируемого, неврологического расстройства. Была выделена вульводиния локализованная и генерализованная (распространенная), а также провоцируемая, не провоцируемая (спонтанная) и смешанная (как провоцируемая, так и не провоцируемая). В то время вульводинию определяли как идиопатическое расстройство с неясными причинами и патогенезом [1].
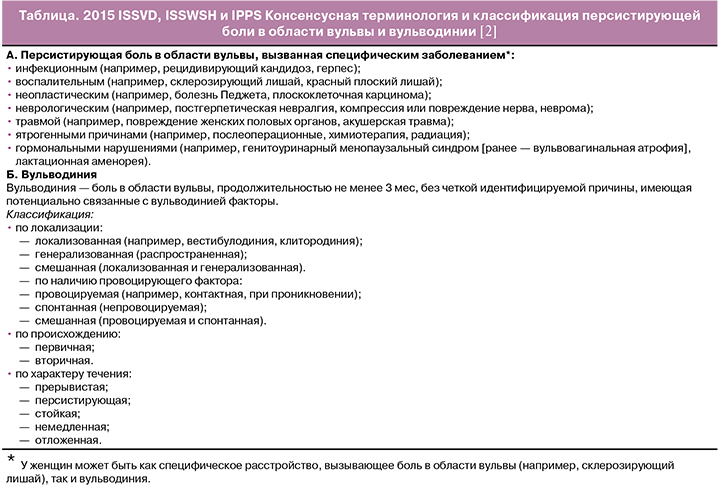
В течение последующих лет существенно расширилась категория идентифицируемых причин и факторов, потенциально связанных с вульводинией (например, воспалительные, генетические, костно-мышечные, нейросенсорные, нейропатические), что привело к необходимости разработки нового определения и системы классификации, а в дальнейшем — лучшей диагностики и лечения. Так, в 2015 г. Международное общество по изучению заболеваний влагалища и вульвы (ISSVD), Международное общество по изучению сексуального здоровья женщин (ISSWSH) и Международное общество по изучению тазовой боли (IPPS) совместно с Американским колледжем Акушерства и гинекологии, Американским обществом по изучению кольпоскопии и патологии шейки матки и Национальной ассоциацией по вульводинии разработали следующие определение и классификацию персистирующей боли в области вульвы и вульводинии, которые отражены в таблице [2]. Ключевым является разделение двух понятий: персистирующей боли в области вульвы, вызванной специфическим диагностируемым заболеванием, и вульводинии, не имеющей идентифицируемой причины, но имеющей потенциально ассоциированный с развитием болевого синдрома ряд факторов.
Вульводиния является хроническим заболеванием с сопутствующими болевыми ощущениями, которое, зачастую, сильно беспокоит женщин и трудно поддается лечению. По данным Harlow B. и соавт. [3], число женщин, страдающих вульводинией, достигло 16%, что равноценно 14 млн женщинам с вульводинией в США. В более позднем исследовании авторы выяснили, что 7—8% женщин двух регионов США в возрасте 40 лет сообщают о боли в области вульвы, характерной для вульводинии. Более того, многие женщины никогда не обращались за лечением, а более 50% при обращении за медицинской помощью не были диагностированы [4]. Локализованная провоцируемая вульводиния встречается чаще, особенно у женщин пременопаузального возраста [5], в то время как генерализованная вульводиния чаще выявляется у женщин в пери- и постменопаузе [6]. Также вульводиния встречается и в подростковом возрасте, но диагностируется и регистрируется гораздо реже в связи с нерегулярным обследованием таких пациенток. [7]
Как и большинство заболеваний с хроническим болевым синдромом, вульводиния сопряжена со снижением качества жизни пациенток, влияя на общее самочувствие, межличностные взаимоотношения, вызывая дискомфорт в повседневной и сексуальной жизни. Ponte M. и соавт. [8] провели опрос среди 280 пациенток Университетской клиники заболеваний вульвы. С помощью шкалы дерматологического индекса Skindex-29, применяемой для кожи вульвы, измерялось качество жизни пациенток с точки зрения кожных поражений. У 101 (36%) пациенток была зарегистрирована вульводиния, у 179 (64%) — другие заболевания вульвы. У женщин с вульводинией было отмечено более низкое качество жизни, чем у пациенток со многими другими дерматологическими заболеваниями, а также выраженное снижение функции, по сравнению с женщинами с другими заболеваниями вульвы (средние баллы [±SD] пациентов с псориазом, другими состояниями вульвы и вульводинией были равны 23±27, 34±24 и 44±22 соответственно, p=0,05). Из изложенного выше следует, что вульводиния оказывает значительное негативное влияние на качество жизни.
Также «2015 ISSVD, ISSWSH и IPPS Консенсусная терминология и классификация персистирующей боли в области вульвы и вульводинии» включает в себя восемь потенциально связанных с вульводинией факторов [2]:
- коморбидность и наличие других болевых синдромов (например, синдром болезненного мочевого пузыря (СБМП), фибромиалгия, синдром раздраженного кишечника (СРК) и т.д.);
- генетические факторы;
- гормональные факторы (например прием фармпрепаратов);
- воспаление;
- скелетно-мышечные факторы (например, гипертонус мышц тазового дна, миофасциальные/биомеханические факторы):
- неврологические факторы: расстройство центральной нервной системы;
- расстройство периферической нервной системы (нейропролиферация).
- психосоциальные факторы (например, настроение, межличностное общение, сексуальная функция);
- структурные дефекты (например анатомические изменения промежности).
Стоит отметить, что чаще всего вульводиния возникает по причине воздействия сразу нескольких факторов, дополняющих друг друга и участвующих в патогенезе развития расстройства. Очевидно, что подход к лечению также должен быть комплексным и междисциплинарным.
Одним из ключевых факторов, потенциально ассоциированных с вульводинией, является коморбидность. Reed B. и соавт. [9] провели анкетирование со скрининговыми вопросами о 4 заболеваниях, сопровождаемых болью (вульводиния, фибромиалгия, интерстициальный цистит (ИЦ), СРК) среди 1940 женщин юго-восточного Мичигана с вульводинией и без нее. Распространенность диагнозов на основе скрининга варьировала от 7,5% (95% ДИ 1,8; 9,0) для ИЦ; 8,7% (95% ДИ 7,3; 10,4) для вульводинии; 9,4% (95% ДИ 8,1; 11,0) для СРК, до 11,8% (95% ДИ 10,1; 13,7) для фибромиалгии; при этом 27,1% анкет оказались положительными сразу для нескольких заболеваний. Наличие вульводинии было связано с наличием каждого из четырех заболеваний (p<0,001, OR = 2,3-3,3).
Часто вульводиния сочетается с заболеваниями мочевого пузыря, и бывает трудно определить истинный источник боли в области вульвы у пациента из-за совпадения симптомов между вульводинией и другими заболеваниями, например ИЦ, также известным как СБМП. В исследовании случай-контроль спонтанная или спровоцированная вульводиния была выявлена в 23,4% (11/47) или 74,5% (35/47) случаев ИЦ соответственно, и ни в одном из случаев группы контроля (p<0,001), что может свидетельствовать о том, что у женщин с ИЦ вульводиния фактически является болью в области мочевого пузыря. Оба заболевания также связаны со значительным снижением сексуальной функции, а именно 23,4% (11/47) пациенток с ИЦ по сравнению с 9% (17/188) женщин контрольной группы сообщили об отсутствии половой активности в течение года, предшествовавшего исследованию; основной причиной воздержания женщины называли невыносимую боль в области преддверия влагалища [10]. Hartmann E.H. и Nelson C. [11] в своем исследовании также указывают на снижение половой функции у женщин с вульводинией. Так, при проведении опроса перед лечением 92% пациенток сообщали о ведении активной половой жизни до появления болевого синдрома, а с момента возникновения боли только 42% могли вступать в половой акт. Проведение теста на чувствительность к калию (PST — potassium sensitivity test) позволяет выявить повреждение слизистой оболочки мочевого пузыря, нарушение ее целостности и проникновение какой-либо агрессивной среды (мочи или, в данном случае, калия) в толщу стенки с провоцированием болевого синдрома. По результатам одного исследования [12], из 122 пациенток с вульводинией 102 (84%) имели положительный результат теста PST, при этом 97 (80%) имели какие-либо урологические симптомы. Это указывает на связанное с мочевым пузырем происхождение боли у пациенток с вульводинией. СБМП заслуживает гораздо большего внимания при дифференциальной диагностике пациенток с вульводинией. Вместе с тем, вульводиния и СБМП тесно сопряжены ввиду общей этиологии. И вульва, и мочевой пузырь эмбрионально развиваются из урогенитального синуса и имеют общую иннервацию. Более того, и влагалище, и уретра, окружены мышцей, поднимающей задний проход, гиперактивность которой сужает вход во влагалище, что вызывает диспареунию. Повторная механическая травматизация слизистой оболочки преддверия влагалища, уретры и треугольника мочевого пузыря во время полового акта приводит к появлению боли в мочевом пузыре. И наоборот, патология мочевого пузыря может приводить к появлению болевых симптомов со стороны вульвы [13].
По некоторым данным, прием комбинированных оральных контрацептивов (КОК) в комбинации с генетическими особенностями женщин может привести к возникновению симптомов вульводинии. При исследовании генотипа женщин, развивших вестибулодинию на фоне приема КОК (содержащих дроспиренон), было выявлено бóльшее количество CAG (цитозин-аденин-гуанин) повторов, определяющих полиморфизм генов андрогеновых рецепторов, чем у женщин, которые принимали те же КОК, но не развивали вестибулодинию. Предполагается, что риск развития индуцированной КОК вестибулодинии может быть вызван снижением свободного тестостерона в сочетании с дисфункцией андрогеновых рецепторов [14].
Большинство воспалительных заболеваний ассоциировано с болевым синдромом, и, вероятно, при хронизации воспалительных процессов боль может приобрести персистирующий характер, что также относится и к боли в области вульвы на фоне хронического воспаления. Повреждение слизистой оболочки вульвы по причине развития воспалительных процессов приводит к периферической и центральной сенситизации. Гиперпролиферация нервных волокон способствует увеличенному восприятию системной боли [15]. S. Gerber и соавт. [16] выявили существование генетических полиморфизмов для генов, кодирующих цитокины, интерлейкиновые рецепторы, для гена лектина, связывающего маннозу (MBL). Эти полиморфизмы приводят к усилению воспалительного ответа, что является предрасполагающим фактором к развитию вульводинии. В работе Tympanidis P. и соавт. отмечено наличие явной связи между увеличением ваниллоидных рецепторов VR1 и вульводинией. Ваниллоидный рецептор VR1 (TRPV1) экспрессируется ноцицепторами, активирующимися капсаицином, протонами и химически-активными веществами, которые образуются при воспалении. Авторы выдвинули гипотезу, что увеличение экспрессии VR1 ноцицепторами способствует развитию вульводинии, поэтому адекватным лечением может служить терапия специфическими антагонистами VR1[17].
Одним из частых инфекционно-воспалительных заболеваний, склонных к рецидивированию, является вагинальный кандидоз, характеризующийся вульварной аллодинией (болезненная гиперчувствительность при прикосновении) и гипериннервацией. На животных моделях было протестировано, может ли повторное локализованное воздействие грибкового патогена на вульву привести к развитию хронической боли. У подмножества самок мышей, подвергнутых рецидивирующей инфекции Candida albicans, развилась провоцируемая механическим воздействием аллодиния, локализованная в вульве. Мыши с аллодинией также приобрели гипериннервацию с пептидергическим ноцицептором и симпатическими волокнами. Гиперчувствительность и гипериннервация присутствовали как минимум в течение 3-х недель после устранения инфекции и воспаления [18].
В настоящее время особое внимание уделяется скелетно-мышечным факторам развития вульводинии, боли в области вульвы, хронической тазовой боли. Мочеполовые инфекции, длительное сидение, персистирующая боль могут привести к гипертонусу мышц тазового дна, формируя порочный круг болевого синдрома. В исследованиях с использованием динамометрического зеркала в сочетании с поверхностной электромиографией было установлено повышение общего тонуса мышц тазового дна, их активацию во время растяжения, снижение силы, скорости, координации и выносливости мышц по сравнению с контрольной группой [19]. При трансперинеальном четырехмерном (4D) ультразвуковом исследовании у женщин с диагностированной провоцируемой вульводинией выявлены значительно меньшая площадь levator hiatus, меньший аноректальный угол и больший угол levator plate в состоянии покоя, по сравнению с бессимптомными женщинами, что указывает на увеличение тонуса мышц тазового дна при провоцируемой вульводинии. Во время максимального сокращения мышц тазового дна обнаружено минимальное сужение levator hiatus area, смещение шейки мочевого пузыря, изменение аноректального угла и угла levator plate у женщин с провоцируемой вульводинией, по сравнению с группой контроля, что указывает на снижение силы сокращения мышц [19].
К сожалению, в настоящее время оптимальное лечение вульводинии еще не разработано, так как существует лишь небольшое количество рандомизированных исследований о лечении вульводинии, а большинство доказательств основано на клиническом опыте, описательных/клинических исследованиях или докладах с комитета экспертов. И вместе с тем, на основании многофакторного патогенеза развития, следует рассматривать индивидуализированный к каждому пациенту междисциплинарный подход специалистов для лечения всех физических и эмоциональных проблем, вызванных болью при вульводинии. Специалистами, участвующими в лечении, могут быть гинекологи, дерматологи, урологи, неврологи, физиотерапевты, мануальные терапевты, сексологи, клинические психологи, специалисты по болевым синдромам.
Ранее опубликованный в 2005 г. алгоритм лечения вульводинии включает в себя уход за вульвой; местные, пероральные и инъекционные препараты; метод биологической обратной связи; физиотерапию; изменение рациона питания; когнитивно-поведенческую терапию; сексуальное консультирование; хирургию. Используемые препараты включают в себя местные и оральные препараты, средства, применяемые в области пораженного участка, а также блокаду пудендальных нервов, акупунктуру и гипнотерапию [20].
Также известно, что большинство используемых медикаментов взаимодействует с другими лекарственными средствами, и многие пациенты с вульводинией могут принимать множество лекарств. Врачей предостерегают наблюдать за потенциальными взаимодействиями лекарственных средств, чтобы предотвратить их до назначения любых новых препаратов [21].
В систематическом обзоре 2015 г. с анализом 391 научных работ о вульводинии отражены следующие варианты лечения [22]:
- местная терапия (как гели с анестетиком для местного применения, так и эстроген-содержащие крема для женщин перименопаузального возраста);
- пероральное лечение (нейромодуляторы: трициклические антидепрессанты — амитриптилин, нортриптилин); антиконвульсанты (габапентин) не рекомендуются авторами систематического обзора 2013 г. [23], а также Jeon Y. и соавт. [24] и Brown C. и соавт. [25]; для купирования острой боли допустимо кратковременное применение опиатов без перехода на постоянное применение; существуют данные о применении антивирусного иммуномодулирующего препарата Изоприназин, в комплексном лечении больных с вульводинией, обусловленной хроническими вульвовагинитами, сопровождающимися вульводинией [26];
- упражнения для мышц тазового дна/физиотерапия наряду с методом биологической обратной связи с целью достижения расслабления мускулатуры тазового дна;
- психотерапия, направленная на развитие способности управлять болью, развитие сексуальности; рекомендуется в качестве первоначальной терапии; в групповом, супружеском или индивидуальном формате консультаций;
- хирургические методы (вестибулэктомия) для пациенток с болевым синдромом более 6 мес, или с частичной/полной неспособностью к половому контакту, или при отсутствии эффективности от всех предыдущих терапевтических методов.
Очевидно, что большинство вышеуказанных методов лечения заключается в симптоматической терапии, способной избавить от болевых ощущений на краткий срок, воздействуя лишь на внешние проявления заболевания. В данном обзоре отражены специфические методы лечения, представляющие наибольший интерес в изучении лечения вульводинии, основанные на патогенезе ее развития.
Среди принципов лечения особую популярность приобретает использование ботулинического токсина. Механизм его действия заключается в ингибировании высвобождения ацетилхолина в холинергическом нервно-мышечном соединении, что приводит к хемоденервации, вызывающей временный вялый паралич. Сначала ботулинический токсин связывается с рецептором на поверхности клеточной мембраны пресинаптического нейрона. Затем он проникает в клетку через пресинаптическую мембрану и нарушает опосредованное кальцием высвобождение ацетилхолина, тем самым предотвращая деполяризацию волокон скелетной мышцы и вызывая паралич, при этом не влияя на постганглионарную холинергическую и симпатическую передачу. Восстановление импульсной передачи происходит постепенно в течение нескольких месяцев, по мере роста новых нервных окончаний и возобновления контакта с постсинаптическим двигательным окончанием. Ботулинический токсин может вводиться в разные мышцы тазового дна, а именно билатерально в участки луковично-губчатых мышц, лобково-прямокишечных и лобково-копчиковых мышц, мышцы, поднимающей задний проход, сухожильный центр промежности [27]. Так, локальное введение ботулинического токсина типа А приводит к длительной миорелаксации и, тем самым, разрывает патологический порочный круг болевого синдрома.
Abbott J. и соавт. [28] провели двойное слепое рандомизированное плацебо-контролируемое исследование с участием 60 женщин с минимум 2-летней историей хронической тазовой боли и объективными доказательствами спазма мышц тазового дна. 30 женщинам из группы провели инъекции 80 единиц ботулинического токсина типа А, и 30 женщин получили инъекции физиологического раствора. Инъекции вводили билатерально в два участка каждой из лобково-прямокишечных и лобково-копчиковых мышц. В результате женщины, которым проводилось лечение ботулиническим токсином типа А, отметили существенное снижение симптомов диспареунии (визуальная аналоговая шкала (ВАШ)= 66 против 12, p<0,001) и не менструальной тазовой боли (ВАШ=1 против 22, p=0,009). В то же время, в группе плацебо ощущение боли только при половом сношении по шкале ВАШ достоверно снизились (64 против 27, p=0,043). Так, устранение спазма мышц тазового дна способствует уменьшению разных видов боли в области таза. Ботулинический токсин типа А снижает давление в мышцах тазового дна, приводя к уменьшению симптомов диспареунии и хронической тазовой боли.
В работе Moga M. и соавт. также описан ряд проведенных исследований, которые подтверждают эффективность использования инъекций ботулинического токсина в гинекологии, в частности, в лечении вагинизма, вульводинии, хронической тазовой боли, нарушений в мочеполовой сфере. При лечении вульводинии применялось введение инъекций в луковично-губчатые мышцы [29]. Pelletier F. и соавт. [30] в исследовании, проведенном с участием 20 пациенток от 18 до 60 лет, указывают на статистически значимое уменьшение симптомов по шкале ВАШ через 3 и 6 мес лечения с использованием ботулинического токсина, вводимого билатерально в луковично-губчатые мышцы 80% пациенткам. При этом 13 пациенток по истечении 3 мес могли вступать в половой контакт без болевых ощущений. Jeon Y. и соавт. [24] провели сравнение эффективности ботулинического токсина и габапентина, применяемого при невралгиях различного генеза. Было показано, что ботулинический токсин более эффективно снижает симптомы вульводинии, по сравнению с габапентином (ВАШ до лечения = 8,1; после лечения = 2,5 против ВАШ до лечения = 8,6; после лечения = 3,2; p<0,001). Brown C. и соавт. [25] было проведено рандомизированное плацебо-контролируемое исследование с участием 230 пациенток, которое не выявило эффективности габапентина по сравнению с плацебо, в связи с чем авторы считают, что назначение габапентина в качестве монотерапии нецелесообразно.
Еще одним потенциальным методом лечения является проведение инъекций богатой тромбоцитами аутоплазмы крови (PRP — platelet-rich plasma). PRP активирует плюрипотентные стволовые клетки в области инъекций, что приводит к омоложению и даже улучшению функции поврежденной или неповрежденной ткани [31]. В одном исследовании о применении PRP авторами утверждается, что тромбоциты высвобождают ряд факторов, таких, как фактор роста тромбоцитов (platelet-derived growth factor), трансформирующий ростовой фактор бета (transforming growth factor-beta), тромбоцитарный фактор роста эндотелиальных клеток (platelet-derived endothelial cell growth factor), тромбоцитарный фактор ангиогенеза (platelet-derived angiogenesis factor) и инсулиноподобный фактор роста (insulin-like growth factor) [32]. Вероятно, именно эти факторы роста способствуют улучшению функции тканей вульвы при проведении инъекций PRP. Более того, медицинская литература демонстрирует безопасность PRP и отсутствие побочных эффектов в виде образования гранулем, инфицирования при использовании в приготовлении инъекционных препаратов одобренных FDA центрифуг [33, 34]. Поскольку PRP полностью аутологична, не существует известных противопоказаний к ее применению. Водная природа PRP позволяет осуществлять инъекцию, используя маленькие иглы, и равномерно распределять препарат по всей окружающей место инъекции ткани. И вместе с тем, проведение этой процедуры продолжает вызывать споры и разногласия, так как клитор и окружающая его область являются деликатной и чувствительной зоной; проведение любых инъекций может привести к повреждению проходящих в этой области многочисленных нервов и кровеносных сосудов. Так или иначе, в самом известном исследовании в этой области Runels C. и соавт. [35] отмечают эффективное использование интравагинальных (в переднюю стенку влагалища в участок между влагалищем и уретрой, наиболее удаленный от мочевого пузыря) и интраклиторальных инъекций PRP в лечении диспареунии или другой сексуальной дисфункции у 11 пациенток. Оценка проводилась методом анкетирования (FSFI — Female Sexual Function Index) и по шкале женских сексуальных расстройств (FSDS-R — Female Sexual Distress Scale Revised) до и после проведения инъекций. Показано значительное снижение показателей по шкале FSDS-R с 17 до 7 баллов (p=0,04), а также у 9 из 11 пациенток (82%) улучшились показатели по шкале FSFI с 1,6 до 14,3 баллов, разница между средним итоговым количеством баллов составила 5,5 (p=0,01). Результаты выявили достоверно значимое снижение сексуальной дисфункции, а именно повышение субъективной оценки в области сексуального желания, возбуждения, количества выделяемой смазки, оргазма у женщин после проведения интравагинальных и интраклиторальных инъекций PRP. Повышение сексуального удовлетворения и снижение боли также были отмечены, но не были статистически значимыми. Авторы предполагают, что при введении PRP активированные тромбоциты выделяют факторы роста и цитокины, оказывающие стимулирующее действие на стволовые клетки, которые дифференцируются в различные виды тканей. Результатом является неоангиогенез, рост фибробластов, гландулярная пролиферация (железы Скина - Skene’s glands) и рост новых нейронов, что способствует улучшению физиологических реакций и повышению чувствительности благодаря улучшению кровоснабжения исследуемой области. Ограниченное число участников этого экспериментального исследования не позволяет сделать смелых выводов в пользу данного метода лечения сексуальной дисфункции и диспареунии. И вместе с тем, необходимо дальнейшее изучение применения PRP у женщин с диспареунией, персистирующей болью в области вульвы или вульводинией, так как данный вид лечения показал высокую оценку среди исследуемых женщин.
Применение гиалуроновой кислоты также является перспективным методом лечения. Гиалуроновая кислота представляет собой полисахарид, состоящий из повторяющихся дисахаридных звеньев глюкуроновой кислоты и N-ацетилглюкозамина. В одном исследовании авторы [36] выявили улучшение сексуальной функции, а также снижение выраженности симптомов ИЦ/СБМП, резистентных к лечению, при внутрипузырном введении раствора гиалуроновой кислоты, благодаря встраиванию гликозаминогликанов в дефекты уротелия мочевого пузыря. Раствор вводили еженедельно 4-кратно через уретральный катетер, после каждого введения пациенткам следовало удерживать раствор в мочевом пузыре в течение 60 мин. Сексуальная функция была оценена у 87 сексуально активных женщин путем сравнения результатов опросника PISQ-9 до и после лечения. Общий результат PISQ-9 и изменение трех отдельных показателей, таких как «диспареуния» (отмечался у 69,0% (n= 60) до лечения, у 44.8% (n=39) через 6 мес после лечения, p<0,001), «отрицательные эмоциональные реакции» (у 36.8% (n=32) до лечения, у 20,7% (n=18) через 6 мес после лечения, p=0,015) и «снижение интенсивности оргазма» (у 52,9% (n=46) до лечения, у 31,0% (n=27) через 6 мес после лечения, p<0,001), указали на тенденцию к улучшению сексуальной функции в течение 6 мес после проведенного лечения. Также, применение вагинальных гелей с гиалуроновой кислотой для уменьшения сухости влагалища в постменопаузе было подробно рассмотрено в многоцентровом рандомизированном контролируемом клиническом исследовании. Результаты показали уменьшение симптомов сухости на 84,44% после 10 процедур применения гиалуронового геля в сравнении с 89,42% после 10 применений крема, содержащего эстриол. Также, после 1 мес лечения гиалуроновой кислотой 56,96±41,47% пациентов сообщили о снижении боли во время полового акта, что связано с увеличением объема вагинального секрета при возбуждении и повышением эластичности тканей влагалища. Вагинальный гель с гиалуроновой кислотой можно рассматривать, как эффективную альтернативу гормональному лечению для облегчения симптомов сухости влагалища, которое обычно сопряжено с диспареунией, зудом, неприятный запахом и дискомфортом даже при таких простых действиях, как ходьба [37]. Американскими учеными в 2015 г. запатентован следующий метод лечения заболеваний слизистой оболочки влагалища и вульвы: рекомендуется введение инъекций гиалуроновой кислоты и ее солей в мышцы влагалища или слизистую его задней стенки. Такой метод может быть использован для лечения атрофии влагалища, синдрома вульварного вестибулита (вестибулодинии), хронических воспалительных патологий, которые привели к дизурии, а также для облегчения диспареунии [38]. Выше изложенная литература о применении гиалуроновой кислоты при заболеваниях вульвы, влагалища, мочевого пузыря, в том числе болевого синдрома в области вульвы, предполагает возможность ее успешного применения в различных лекарственных формах.
В качестве дополнительных методик лечения рассматривается применение физиотерапии. Особенно этот метод рекомендуется при гипертонусе мышц тазового дна [39]. Также ряд клинических рекомендаций предлагает использование физиотерапевтических методик в качестве начальной терапии [40]. В исследовании Andrew T. Goldstein и соавт. [41] использование различных физиотерапевтических методик имеет уровень доказательности B, что означает существование ряда доказательств в пользу их применения. Физиотерапевтические методики лечения могут включать в себя мануальную терапию, технологию биологической обратной связи, вагинальные расширители, чрескожную стимуляцию нервов, различные домашние физические упражнения по укреплению мышц тазового дна. Физиотерапия с применением аппарата с биологической обратной связью заключается в обучении пациенток отслеживать активность мышц тазового дна при помощи вагинального датчика и эффективно расслаблять их, устраняя гипертонус. Наряду с этим, проводится психотерапия и модификация поведенческой активности, направленные на снижение страха боли. Особо отмечается, что применение физиотерапии не всегда возможно и может быть ограничено сильной болевой реакцией пациентки [42]. Согласно исследованию Hartmann D. и соавт., наиболее эффективными физиотерапевтическими методами являются упражнения для мышц тазового дна с биологической обратной связью или без нее, мануальная терапия, обучение пациенток, основанное на исключении раздражителей, приучение к правильной работе кишечника и мочевого пузыря, половым функциям, электротерапия, применение расширителей и других методов проникновения во влагалище. При этом физиотерапевтическое лечение может включать, как один выше представленный метод, так и быть комплексом применяемых методик. Следует подчеркнуть, что такое лечение не используется исключительно физиотерапевтами, а может быть интегрировано в принципы терапии другими специалистами [43]. Физиотерапевтические методы направлены на реабилитацию работы мышц тазового дна: повышение осознанности о функционировании мышц и проприоцепции, улучшение расслабления мышц, нормализацию мышечного тонуса, повышение эластичности мышц и тканей влагалища, снижение чувствительности в болезненной области, снижение боязни проникновения во влагалища [44]. Недавний обзор физиотерапевтических методик, проведенный Morin M. и соавт. [45], показал, что эти методы наиболее эффективны для снижения боли при половом акте и ведут к улучшению сексуальной функции. Аполихина И.А. и соавт. [46] также провели обзор литературы относительно диагностики и лечения дисфункции тазового дна, включающей пролапс тазовых органов, недержание мочи, тазовую боль, сексуальные нарушения. Авторы подчеркивают эффективность тренировок мышц тазового дна в режиме биологической обратной связи, возможности современного оборудования и появление тренажеров, подключающихся к смартфонам (Magic Kegel Master, G-balls), электромиостимуляторов для домашнего использования.
В данный момент обсуждается применение плацентарных препаратов для лечения боли. В основе метода лежит использование стволовых клеток, выделенных из плаценты человека [47]. Предполагается, что введение стволовых клеток способствует запуску механизма пролиферации, аналогично механизму действия PRP.
Заключение
Таким образом, на развитие вульводинии и формирование хронического болевого синдрома влияет множество различных факторов у каждой конкретной пациентки, из чего можно сделать вывод: лечение женщин с вульводинией должно быть индивидуализированным и междисциплинарным. Основными факторами, способствующими развитию заболевания, является коморбидность, другие болевые синдромы в анамнезе, хроническое воспаление, гипертонус мышц тазового дна, генетические, неврологические факторы, психосоциальные проблемы. Лечение вульводинии является комплексным, влияющим на разные структуры, потенциально пораженные при развитии расстройства. Базовая терапия включает в себя местные и пероральные препараты, физиотерапию, основанную на расслаблении мышц тазового дна, психотерапию, хирургические методы. Актуальной сферой изучения является специфическая терапия вульводинии, включающая применение ботулинического токсина типа А, препаратов PRP, плацентарных препаратов. Не остается сомнений, что тема персистирующей боли в области вульвы и вульводинии, механизмов развития этого расстройства, своевременной постановки диагноза, а также поиск и валидация современных методов лечения требуют дальнейшего изучения и клинических исследований.