Chronic pelvic pain syndrome in gynecological practice
Teterina T.A., Apolikhina I.A.
Keywords
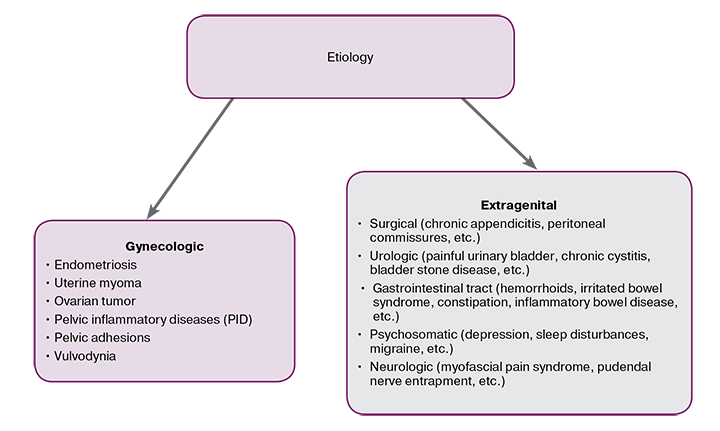
Chronic Pelvic Pain (CPP) is a permanent or repetitive benign pain, occurring in the pelvic area during the period of more than 6 months (IASP – International Association for the Study of Pain). It is a general term which covers a wide range of diagnoses that characterized by permanent pain in the pelvic area lasting for more than 6 months and resulting in a significant worsening of general condition and the quality of woman’s life. CPP syndrome is the diagnosis of exclusion!
ICD – 10 code
N94 Pain and other conditions associated with female genital organs and menstrual cycle.
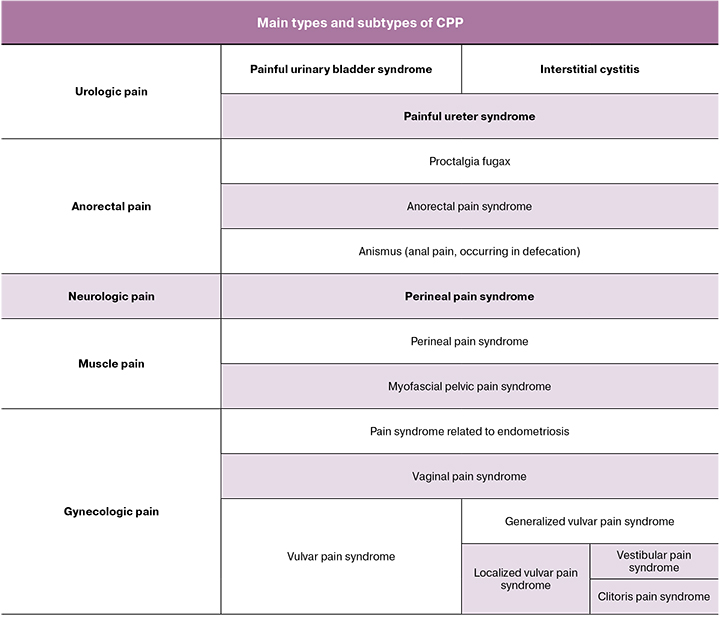
Gynecologic pain terminology
Vulvodynia is the pain located in vulva, clitoris (clitorodynia) and vaginal vestibule (vestibulodynia), of more than 3 months’ duration, occurring usually all at once, without any certain reason:
- localized / generalized / mixed;
- precipitated / spontaneous;
- primary / secondary;
- permanent / persisting, etc.
Dyspareunia is a painful sexual intercourse.
Vaginismus is a spontaneous contraction of pelvic muscles, surrounding the lower third of the vagina.
- Vaginismus morbidity is unknown, and the rates indicated in the literature are widely variable.
- Vaginismus can be primary / secondary, complete / partial and/or situational According to DSM-5 (Diagnostic and statistical manual of mental disorders) dyspareunia and vaginismus are joined into one diagnostic category: genito-pelvic pain / penetration disorder (GPPPD).
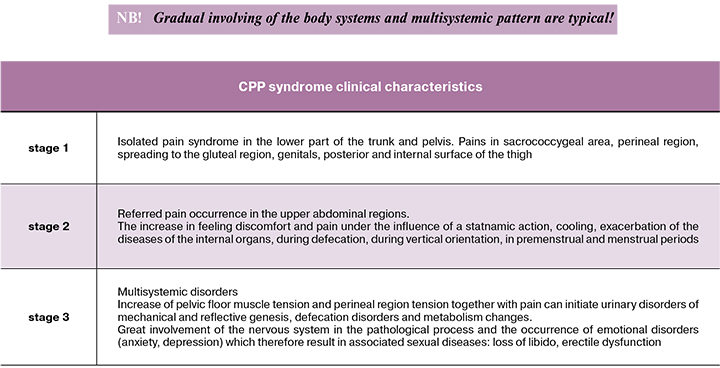
CPP obligatory features are:
- pain syndrome duration more than 6 months;
- low efficiency of the therapy;
- incompatibility of the patient’s pain sense with the tissue damage;
- symptoms of depression;
- developing limitation of the physical activity;
- behavioral disorders.
Diagnosis
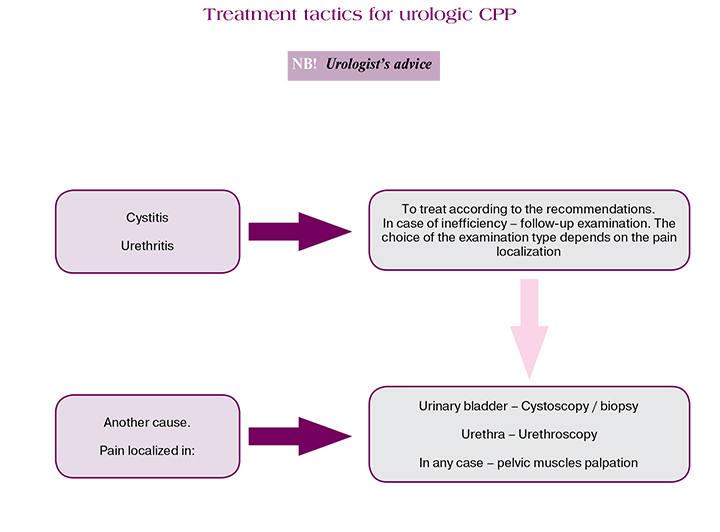
Standard examination of the patients with CPP should involve:
- clinical examination: clarification of the complaints and patient’s history (it is necessary to find out the possibility of prior inflammatory and infectious diseases and to exclude the accompanying pathology);
- laboratory assessment: analyses of blood and urine, biochemical blood count, tumor markers, microbiology investigation (urine, vaginal, urethra and cervical secretion);
- pelvic and urinary tract ultrasound, transrectal ultrasound, duplex and Doppler pelvic vessels ultrasound ;
- X-ray examination of the lumbar spine and pelvic bones;
- lumbosacral and pelvic MRI;
- densitometry for excluding osteoporosis;
- X-ray (irrigoscopy) and endoscopic (proctosigmoidoscopy, colonoscopy, cystoscopy) examination of gastrointestinal tract and urinary bladder;
- diagnostic laparoscopy.
However, the biggest difficulty occurs during the treatment of the patients with idiopathic pain, who comprise 30% of the total number of patients. This is unexplained CPP syndrome.
Invasive treatments for resistant pain
Pudendal nerve block is performed by a specially trained team – an anesthesiologist or an algologist under the control of computer tomography or ultrasound.
Transcutaneous electrical nerve stimulation (TENS).
Sacral neuromodulation - neuropathic pain and complex syndromes of regional pain are successfully treated using spinal and peripheral nerves neurostimulation.
CPP syndrome is a socially significant disabling condition, which involves a large number of clinical symptoms and which is characterized by multisystemic pattern. Its etiology and pathogenesis are often unspecified. For successful treatment, a detailed anamnesis and thorough physical examination with adequate laboratory assessment and careful attitude to the therapy are required, starting from less dangerous methods and finishing with invasive procedure according to the stated algorithms. In this respect surgical methods can be performed only if other methods appeared to be ineffective. A multidisciplinary approach together with the involvement of the specialized professionals are recommended, as well as psychotherapist’s supervision in almost every case.
References
- Шмидт А.А., Безменко А.А., Гаворонских Д.И. Клинические протоколы (гинекология). 3-е изд., доп. С.-Пб.: СпецЛит, 2019. 160 с.[Schmidt A.A., Bezmenko A.A., Gavoronskikh D.I. Clinical protocols (gynecology). 3rd ed., Ext. S.-Pb .: SpetsLit, 2019.160 s. in Russ.)]
- Барулин А.Е., Курушина О.В., Думцев В.В. Современные подходы к терапии хронической тазовой боли. РМЖ. 2016; 13: 847–1.[Barulin A.E., Kurushina O.V., Dumtsev V.V. Current approaches to management of chronic pelvic pain. RMJ. 2016; 13: 847–851.(in Russ.)] https://www.rmj.ru/articles/nevrologiya/Sovremennye_podhody_k_terapii_hronicheskoy_tazovoy_boli/#ixzz6B5D5XOSJ
- Письмо Минздрава России от 22.11.2013 N 15-4/10/2-8710 (вместе с "Клиническими рекомендациями (протоколом лечения)...", утв. Российским обществом акушеров-гинекологов 30.10.2013).[ Pis'mo Minzdrava Rossii ot 22.11.2013 N 15-4/10/2-8710
(vmeste s "Klinicheskimi rekomendatsiyami (protokolom lecheniya)...", utv. Rossiyskim obshchestvom akusherov-ginekologov 30.10.2013).(in Russ.). http://www.consultant.ru/document/cons_doc_LAW_320513/ - Грудкин А.А., Константинова О.Д., Доброхотова Ю.Э. Сложности и ошибки диагностики причин хронической тазовой боли. Медицинский альманах. 2010; 4 (13). 184–8. [ Grudkin A.A., Dobrohotova J.E., Konstantinova O.D. The complexities and error diagnosis of the causes of chronic pelvic pain. Medicinskij al'manah. 2010; 4 (13). 184–8. (in Russ.)]
- Яроцкая Е.Л., Адамян Л.В. Особенности тактики ведения гинекологических больных, страдающих тазовыми болями. Проблемы репродукции. 2003; 3:17–26. [Yarockaja E.L., Adamjan L.V. Osobennosti taktiki vedenija ginekologicheskih bol'nyh, stradajushhih tazovymi boljami. Problemy reprodukcii. 2003; 3: 17–26. (in Russ.)].
- Зайцев А.В., Шаров М.Н., Кан Я.Д. Хроническая тазовая боль. Современное мультимодальное представление о проблеме. Перспективы диагностики и лечения. Российский журнал боли. 2015; 2: 3-8. [Zajcev A.V., Sharov M.N., Kan Ja.D. Hronicheskaja tazovaja bol’. Sovremennoe mul’timodal’noe predstavlenie o probleme. Perspektivy diagnostiki i lechenija. Rossijskij zhurnal boli. 2015; 2: 3-8. (in Russian)].
- Bornstein J., Goldstein A.T., Stockdale C.K., Bergeron S., Pukall C., Zolnoun D., Coady D. 2015 ISSVD, ISSWSH, and IPPS Consensus Terminology and Classification of Persistent Vulvar Pain and Vulvodynia J Lower Gen Tract Dis. 2016; 20: 126-30.
- Goldstein A.T., Pukall C.F. Provoked vestibulodynia. In: Goldstein AT, Pukall CF, Goldstein I, eds. Female Sexual Pain Disorders: Evaluation and Management. Oxford, England: Wiley-Blackwell; 2009: 43-8.



