For the first time in Russia: delivery of twins in patient with premature ovarian insufficiency after a onestage surgical procedure for activation of ovarian function
Premature ovarian insufficiency (POI) is a multifactorial disease with a significant contribution of genetic factors; one of the leading socially significant complaints in this disease is persistent infertility with a high resistance to standard treatment methods. The method for activating follicular growth, which was first described by K. Kawamura, A. Hsueh and co-authors, turned out to be effective and it was confirmed clinically and by molecular genetic research data. Currently, it has been used in various modifications in more than 6 countries around the world. In Russia, the first operation based on surgical activation of ovarian function was performed by academician of the Russian Academy of Sciences L.V. Adamyan on March 06, 2019. For the first time in Russia, a 32-year-old patient suffering from premature ovarian insufficiency with dichorionic diamniotic twins underwent planned operative delivery by caesarean section at 37 weeks and 4 days of gestation. The operation was performed at the V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Moscow, Russia, on October 01, 2020. The patient became pregnant spontaneously 1.5 months after undergoing surgical treatment aimed at restoring reproductive potential. A one-stage surgical procedure for activation of ovarian function was performed by academician L.V. Adamyan on December 13, 2019. Conclusion. This clinical case of a spontaneous pregnancy and delivery in the patient with POI demonstrates that this operation is appropriate to be performed in patients with a noticeable decrease in the ovarian reserve, and it can be considered as an alternative to oocyte donation.Adamyan L.V., Dementyeva V.O., Asaturova A.V., Stepanian A.A., Smolnikova V.Yu., Arakelyan A.S., Gus A.I., Nikolaeva A.V.
Keywords
Premature ovarian insufficiency (POI) is a multifactorial disease with a significant contribution of genetic factors; one of the leading socially significant complaints in this disease is persistent infertility with a high resistance to standard treatment methods. POI refers to hypogonadism in women under 40 years who previously had normal menstrual cycle. The diagnosis of POI is confirmed by the combination of two serial measurements of elevated FSH level > 25 IU/L taken > 4 weeks apart [1]. POI prevalence ranges from 1 to 13% [2].
The method for activating follicular growth which was first described by K. Kawamura, A. Hsueh and co-authors, turned out to be effective and it was confirmed clinically and by molecular genetic research data. Currently, it has been used in various modifications in more than 6 countries around the world [3, 4]. One of the basic explanations why surgical procedure was effective in this method was the influence of the ovarian tissue fragmentation on actin polymerization, termination of signal transmission in Hippo pathway, increase in the concentration of growth factor CCN and apoptosis inhibitors BIRC 1.7 [5]. The Japanese researchers initially proposed performing unilateral ovariectomy which was followed by demedullation with histological evaluation, cryopreservation of ovarian cortical strips, their fragmentation and a two-day in vitro activation (addition to the medium of PTN inhibitor and PI3K signaling pathways activator). Then, ipsilateral transplantation of the thawed fragmented tissue in the subserous mucosa of the fallopian tube was performed laparoscopically [6].
Further study of the fundamental mechanisms of surgical activation of ovarian tissue made it possible to improve the technique to a one-stage method. In the Russian Federation, the first operation on surgical activation of ovarian tissue was performed by academician L.V. Adamyan on 6 March, 2019 [6]. Moreover, appropriate approaches to management tactics were developed, including patient selection criteria, clinical and laboratory examination, preoperative preparation, surgical treatment and postoperative management.
Clinical observation
A 32-year-old patient A. with confirmed diagnosis of POI presented to the Academician V.I. Kulakov National Medical Research Centre for Obstetrics, Gynecology and Perinatology for the treatment aimed at achieving pregnancy using the patient’s own oocytes. Her medical history included the following: she was born spontaneously by vaginal delivery at term to a 27-year-old mother; she is the second child in the family and has an older sister. Her mother’s menopausal age is 52 years.
 Her menarche was at the age of 14, and her cycle lasting 28 days became regular at the same period; her menstruation was 4–5 days, moderate and painless. Over the past two years, there has been a change in the rhythm of menstruation: the cycle shortened to 24–25 days, and the volume of menstrual blood loss decreased. Hormonal examination showed some periods of elevated serum FSH levels to 33 IU/L which were associated with episodes of oligomenorrhea; therefore, hormone replacement therapy (estradiol valerate 2 mg + didrogesterone 10 mg) was administered during two menstrual cycles before surgery to improve the effectiveness of the surgical stage of treatment. The patient was examined, and due to the critical decrease in the ovarian reserve and the unreasonable ovarian function stimulation, oocyte donation was recommended to the patient as the only possible option to achieve pregnancy.
Her menarche was at the age of 14, and her cycle lasting 28 days became regular at the same period; her menstruation was 4–5 days, moderate and painless. Over the past two years, there has been a change in the rhythm of menstruation: the cycle shortened to 24–25 days, and the volume of menstrual blood loss decreased. Hormonal examination showed some periods of elevated serum FSH levels to 33 IU/L which were associated with episodes of oligomenorrhea; therefore, hormone replacement therapy (estradiol valerate 2 mg + didrogesterone 10 mg) was administered during two menstrual cycles before surgery to improve the effectiveness of the surgical stage of treatment. The patient was examined, and due to the critical decrease in the ovarian reserve and the unreasonable ovarian function stimulation, oocyte donation was recommended to the patient as the only possible option to achieve pregnancy.
At the preoperative stage, a complete clinical and laboratory study was performed. The basal levels of gonadotropins were the following: FSH – 33 IU/L, LH – 9.7 IU/L, estradiol – 73.4 pmol/L, AMH < 0.13 ng/ml. According to the examination, clinical and laboratory studies, including 3D ultrasound imaging, the patient was diagnosed with infertility, decreased ovarian reserve.
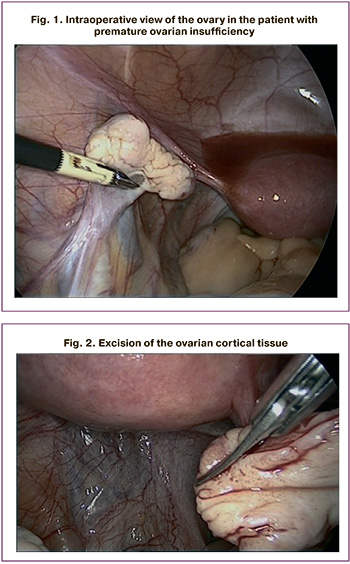
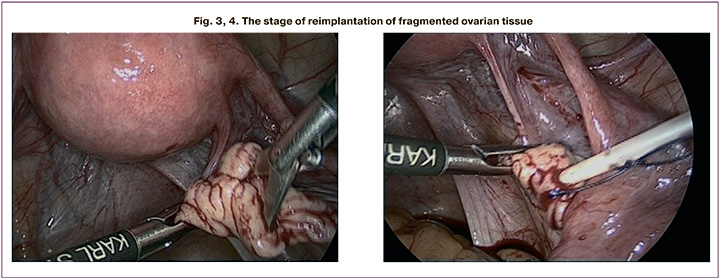
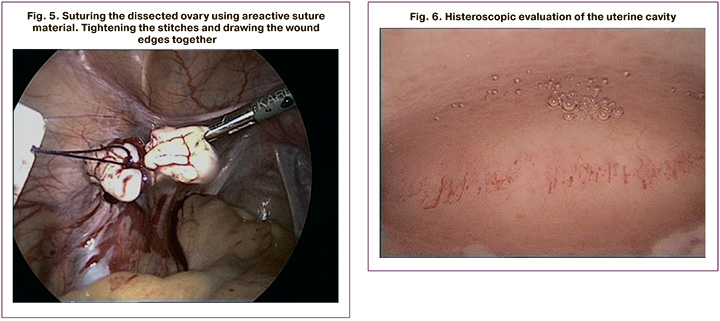
Given the presence of infertility for two years, the absence of the effect from the previous treatment, a marked decrease in the ovarian reserve, as well as the patient’s insistent desire to achieve pregnancy using her own oocytes, it was decided to perform an operation, namely a one-stage surgery for activating ovarian function: laparoscopy, exploration of the abdominal and pelvic cavity, chromohydrotubation, ovarian cortical biopsy followed by its fragmentation and one-stage reimplantation, hysteroscopy, endometrial biopsy (Fig. 1–6) [6]. After obtaining the patient’s informed consent, surgical intervention was performed as planned at the preoperative stage. Intraoperatively, the ovaries were found to be reduced in size (27x18x22 mm), they were whitish-yellow and had deep grooves on their surfaces; they had a dense consistency and no functionally active stigmas (without visible follicles, yellow and white bodies) (Fig. 1); the incision revealed the signs of minimal vascularization and thickened tunica albuginea. Hysteroscopy revealed that the endometrium had equal thickness, the vascular pattern was not accentuated, and the glandular tissue was not changed. The abdominal organs did not show any visible pathological changes. The appendix was previously removed.
Endometrial samples and 10% of the volume of each ovarian fragment were sent for histological examination. Histological examination revealed ovarian tissue with cortical fibrosis without visualization of the follicular apparatus. The endometrium was at the stage of early proliferation.
The surgical intervention lasted 1 hour and 5 minutes without complications, the blood loss was 10 ml. The postoperative period was uneventful. The patient was discharged on third day after surgery.
On the third day after surgery, a repeated hormonal study was performed to determine the level of gonadotropins and estradiol. The estradiol level was 335 pmol/L, which was 4.5 times higher than the preoperative concentration. There were no significant changes in gonadotropin levels.
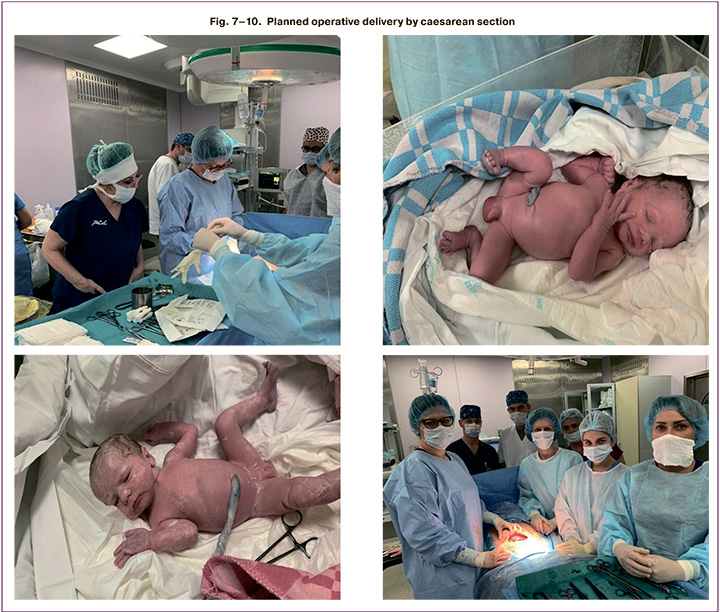
After undergoing surgery 1.5 months later, the patient was found to have a serum β-hCG level 800 mIU/ml due to delayed menstruation. Ultrasound examination revealed the presence of multiple pregnancy, namely, dichorionic diamniotic twins. The pregnancy was uneventful during the entire gestation period. According to screening studies, no abnormalities were detected. On October 01, 2020, the woman had a planned operative delivery by caesarean section at 37 weeks and 4 days of gestation (surgeon A.V. Nikolaeva). The operation lasted 33 minutes without complications. On the 2nd minute, a live full-term girl weighing 2620 g and 49 cm long was delivered for the inguinal folds. The condition was assessed 8/9 points on the Apgar scale. On the 3rd minute, a live full-term boy weighing 2332 g and 47 cm long was delivered for the armpits. The condition was assessed 8/8 on the Apgar scale (Fig. 7–10).
The postpartum period was uneventful.
In the future, it is planned to monitor the patient’s condition dynamically with a full clinical and laboratory examination.
Conclusion
Our management tactics, including clinical, laboratory and instrumental examinations, hormonal regulation, and the surgical stage, namely, a one-stage surgical method for activating ovarian function, resulted in the improvement of general condition, psychological and emotional state in some patients, as well as changes in ovarian reserve indicators. Positive dynamics of the hormonal status associated with activation of follicular growth according to ultrasound data was observed; a number of patients had a response to stimulation of ovarian function in IVF cycles followed by obtaining their own cellular material and achieving pregnancy.
This clinical case of a spontaneous pregnancy and delivery in the patient with POI demonstrates that this operation is appropriate to be performed in patients with a noticeable decrease in the ovarian reserve, and it can be considered as an alternative to oocyte donation.
References
1. Baber R.J., Panay N., Fenton A.; IMS Writing Group. 2016 IMS Recommendations on women’s midlife health and menopause hormone therapy. Climacteric. 2016; 19(2): 109-50. https://dx.doi.org/10.3109/136971 37.2015.1129166.
2. Panay N., Kalu E. Management of premature ovarian failure. Best Pract. Res. Clin. Obstet. Gynaecol. 2009; 23(1): 129-40. https://dx.doi.org/10.1016/j. bpobgyn.2008.10.008.
3. Kawamura K., Kawamura N., Hsueh A.J. Activation of dormant follicles: a new treatment for premature ovarian failure? Curr. Opin. Obstet. Gynecol. 2016; 28(3): 217-22. https://dx.doi.org/10.1097/GCO.0000000000000268.
4. Kawamura K., Cheng Y., Suzuki N., Deguchi M., Sato Y., Takae S. et al. Hippo signaling disruption and Akt stimulation of ovarian follicles for infertility treatment. Proc. Natl. Acad. Sci. USA. 2013; 110(43): 17474-9. https://dx.doi. org/10.1073/pnas.1312830110.
5. Cheng Y., Feng Y., Jansson L., Sato Y., Deguchi M., Kawamura K. et al. Actin polymerization-enhancing drugs promote ovarian follicle growth mediated by the Hippo signaling effector YAP. FASEB J. 2015; 29(6): 2423-30. https:// dx.doi.org/10.1096/fj.14-267856.
6. Адамян Л.В., Дементьева В.О., Асатурова А.В., Назаренко Т.А. Одноэтапный хирургический метод активации функции яичников (первое клиническое наблюдение). Проблемы репродукции. 2019; 25(1): 97-9. https:/ dx.doi.org/10.17116/repro20192501197. [Adamyan L.V., Dementieva V.O., Asaturova A.V., Nazarenko T.A. One-stage surgical method of ovarian function activation (first clinical observation). Russian Journal of Human Reproduction. 2019;25(1):97-9. (in Russian)]. https://dx.doi.org/10.17116/repro20192501197.
Received 03.10.2020
Accepted 06.10.2020
About the Authors
Leyla V. Adamyan, Academician of RAS, MD, PhD, Professor RAS, Honored Master of Science of the Russian Federation, Head Specialist in Obstetrics and Gynecology of Ministry of Health of Russia, Vice-Director of Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Head of Gynecologic Surgery Department of Academician V.I. Kulakov National Medical Research Center of Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia.Tel.: +7(495)438-40-68. E-mail: adamyanleila@gmail.com. 117997, Russia, Moscow, Ac. Oparina str., 4.
Victoria O. Dementyeva, PhD student, Academician V.I. Kulakov National Medical Research Center of Obstetrics, Gynecology and Perinatology. E-mail: victoriadementyeva93@gmail.com. 117997, Russia, Moscow, Ac. Oparina str., 4.
Alexanda V. Asaturova, PhD, pathologist, Head of the Pathomorphological Department, Academician V.I. Kulakov National Medical Research Center of Obstetrics, Gynecology and Perinatology. E-mail: a_asaturova@oparina4.ru. 117997, Russia, Moscow, Ac. Oparina str., 4.
Assia A. Stepanian, Academia of Women’s Health and Endoscopic Surgery, SurgeryU Founder. Tel.: 404.549.3224. E-mail: astep@migsurgery.com, Atlanta, USA. Veronika Yu. Smolnikova, PhD, Leading Researcher in the Department of Assistive Technologies in the Treatment of Infertility named after B.V. Leonov, Academician V.I. Kulakov National Medical Research Center of Obstetrics, Gynecology and Perinatology.
E-mail: veronika.smolnikova@mail.ru. 117997, Russia, Moscow, Ac. Oparina str., 4.
Alek S. Arakelyan, Ph.D., Senior Researcher of the Gynecological Department, Academician V.I. Kulakov National Medical Research Center of Obstetrics, Gynecology and Perinatology. E-mail: a_arakelyan@oparina4.ru. 117997, Russia, Moscow, Ac. Oparina str., 4.
Aleksandr I. Gus, PhD, professor, Head of the Department of Ultrasound and Functional Diagnostics, Academician V.I. Kulakov National Medical Research Center of Obstetrics, Gynecology and Perinatology. E-mail: a_gus@oparina4.ru.
Anastasia V. Nikolaeva, PhD, Chief Physician, Academician V.I. Kulakov National Medical Research Center of Obstetrics, Gynecology and Perinatology. E-mail: a_nikolaeva@oparina4.ru. 117997, Russia, Moscow, Ac. Oparina str., 4.
For citation: Adamyan L.V., Dementyeva V.O., Asaturova A.V., Stepanian A.A., Smolnikova V.Yu., Arakelyan A.S., Gus A.I., Nikolaeva A.V. For the first time in Russia: delivery of twins in patient with premature ovarian insufficiency after a one-stage surgical procedure for activation of ovarian function. Akusherstvo i Ginekologiya / Obstetrics and gynecology. 2020; 10: 42-47 (in Russian)
https://dx.doi.org/10.18565/aig.2020.10.42-47