Матка Кувелера (МК), или маточно-плацентарная апоплексия, впервые была описана в 1912 г. французским акушером-гинекологом Александром Кувелером. Он характеризовал такую матку как апоплексичную, пропитанную кровью, синюшную, неспособную к сокращениям, с точечными кровоизлияниями на серозной оболочке [1].
Преждевременная отслойка нормально расположенной плаценты (ПОНРП) с формированием ретроплацентарной гематомы наблюдается в 0,4–1,4% всех беременностей, приводит к развитию этого грозного осложнения под названием «матка Кувелера» и может быть причиной крайне неблагоприятных последствий для матери и плода, вплоть до летального исхода [2]. Материнская смертность при данном осложнении достигает 5%. Плод чаще всего погибает внутриутробно [3]. В развитых странах примерно 10% всех преждевременных родов и 10–20% перинатальных потерь вызваны ПОНРП [4].
Факторы риска ПОНРП, в том числе приводящие к развитию матки Кувелера, хорошо известны; к ним следует относить предшествующую отслойку плаценты, курение, травму, употребление кокаина, многоплодную беременность, многоводие, гипертоническую болезнь, преэклампсию, тромбофилию, поздний репродуктивный возраст матери, внутриутробные инфекции [5–7].
Преэклампсия в сочетании с длительным течением заболевания и донной или роговичной локализацией плаценты являются факторами риска развития маточно-плацентарной апоплексии [8]. По данным Y. Li et al., преэклампсия как основной фактор риска отслойки плаценты отмечалась в 39% случаев [6]. В то же время такие осложнения, как преэклампсия, задержка внутриутробного роста плода и преждевременная отслойка плаценты, являются составляющими синдрома «ишемической болезни плаценты», в основе которого лежат общие патофизиологические механизмы [9–11].
Решающее значение в возникновении матки Кувелера, по данным исследования A. Brăila et al., принадлежало наличию сочетания факторов: генетические нарушения, осложненный гинекологический анамнез (аборты, кюретаж), многоплодная беременность (89,5%), возраст матери старше 30 лет (68,5%), гипертоническая болезнь (100%), миома матки (10,5%) [2].
В то же время, по данным другого исследования, ПОНРП может произойти в любом возрасте, возникать при первой беременности, не иметь прямого отношения к паритету, количеству предыдущих абортов, артериальной гипертонии, врожденным аномалиям развития матки и механическим причинам, приводящим к разрыву матки [12].
Нарушение физиологической трансформации спиральных артерий является одним из основных факторов, способствующих развитию ПОНРП. При разрыве сосудов в decidua basalis образуется гематома, которая отслаивает плаценту от мышечной оболочки матки. Если отслойка прогрессирует, то в случае формирования ретроплацентарной гематомы происходит внутреннее кровотечение. Накопившаяся между стенкой матки и плацентой кровь пропитывается в плаценту и в мышечную стенку матки, что приводит к ее перерастяжению. В мышечном слое матки образуются трещины, вся стенка, вплоть до серозной оболочки, пропитывается кровью [13].
Развитие синдрома диссеминированного внутрисосудистого свертывания (ДВС) крови вследствие отслойки плаценты и внутриутробной гибели плода не является редкостью. Это может привести к увеличению материнской смертности и необходимости проведения гистерэктомии, а также к увеличению объема переливаемой крови, если родоразрешение не будет произведено в течение ближайшего времени [14, 15]. Серьезные нарушения в системе гемостаза являются частыми, отягощающими прогноз осложнениями при матке Кувелера. Нарастающая ретроплацентарная гематома быстро потребляет материнские факторы свертывания, что может вызвать дефицит фибриногена от вторичного фибринолиза до афибриногенемии [2]. Нарушение свертывания крови вследствие чрезмерного потребления фибриногена считается основным патогенетическим фактором развития ДВС-синдрома у женщин с ПОНРП [16]. Кроме того, в месте отслойки плаценты при наличии ретроплацентарной гематомы образуется большое количество тромбопластина, который проникает в системный кровоток и также способствует развитию ДВС-синдрома.
Основным регламентированным видом оперативного лечения при наличии матки Кувелера в нашей стране является гистерэктомия. Консервативная терапия или выжидательная тактика при тяжелой отслойке плаценты, приводящей к возникновению матки Кувелера, не применяется [17].
В то же время в странах западной Европы и США матка Кувелера не считается абсолютным показанием для радикальной операции. В последние годы разработаны и успешно используются органосохраняющие методики, которые получают все большее распространение [18]. Основное условие для их применения – это отсутствие ДВС-синдрома и наличие стабильных гемодинамических показателей у матери.
В последнее время стали появляться зарубежные публикации, описывающие случаи оставления матки Кувелера даже при наличии большой кровопотери [19–21]. Собственный опыт проведения органосохраняющей тактики при данной патологии мы хотим представить в данной статье.
За последние пять лет в нашей клинике – Красноярском краевом клиническом центре охраны материнства и детства (ККК ЦОМД) успешно была осуществлена органосохраняющая оперативная тактика у 6 пациенток с ПОНРП и маткой Кувелера, диагностированной в ходе выполнения экстренного оперативного вмешательства.
В большинстве случаев (83,3%) ПОНРП с развитием матки Кувелера отмечалась в III триместре беременности при гестационном сроке от 34 до 38+6 недель. Ровно в половине случаев (50%) при этом осложнении площадь отслойки плаценты составляла 1/2 от ее поверхности, а в 33% случаев имела место тотальная отслойка плаценты (табл. 1).

Объем кровопотери у пациенток с маткой Кувелера не только непосредственно влияет на тяжесть их состояния и показатели гемостаза, но и во многом определяет объем оперативного вмешательства, а также арсенал применяемых способов остановки кровотечения (от органосберегающих до гистерэктомии). У 4 пациенток с маткой Кувелера общий объем кровопотери находился в пределах от 1500 до 2500 мл, что составило 66,6%, а в 2 случаях – несущественно превышал допустимую при операции кесарева сечения норму (от 1300 до 1400 мл).
Способы минимизации кровопотери при выполнении оперативного вмешательства у пациенток с диагностированной маткой Кувелера в зависимости от клинической ситуации включали в себя комплекс различных мероприятий: аутореинфузия эритроцитов (Cell-Saver), восполнение объема циркулирующей крови (достаточная по объему и сбалансированная инфузионная терапия), рациональное использование утеротоников (включая окситоцин, карбетоцин и мизопростол), компрессионные швы на матку, медикаментозная коррекция гемостаза (транексамовая кислота, коагил, протромплекс), местное использование вазопрессорных препаратов (ремистип), деваскуляризация матки с применением перевязки маточных артерий или дистального гемостаза.
Органосберегающий подход в нашем перинатальном центре (ККК ЦОМД), основанный на применении современных высокотехнологичных методик хирургического и медикаментозного гемостаза и кровосбережения, даже в случаях массивной акушерской кровопотери, позволяет в большинстве случаев не прибегать к гистерэктомии. Самой частой причиной массивных акушерских кровотечений в нашем центре, как и в подавляющем большинстве перинатальных центров нашей страны, являются ситуации, связанные с врастанием плаценты. Второе место среди причин массивных акушерских кровопотерь занимает ПОНРП. За последние пять лет кровопотеря свыше 1500 мл при ПОНРП встречалась с частотой от 23,8% до 45,1%. При этом только в одном из этих случаев, закончившихся относительно благополучно, была произведена гистерэктомия (табл. 2).
В качестве наглядных примеров органосберегающей тактики у пациенток с маткой Кувелера мы решили привести 2 клинических наблюдения из собственной практики.
Клиническое наблюдение № 1
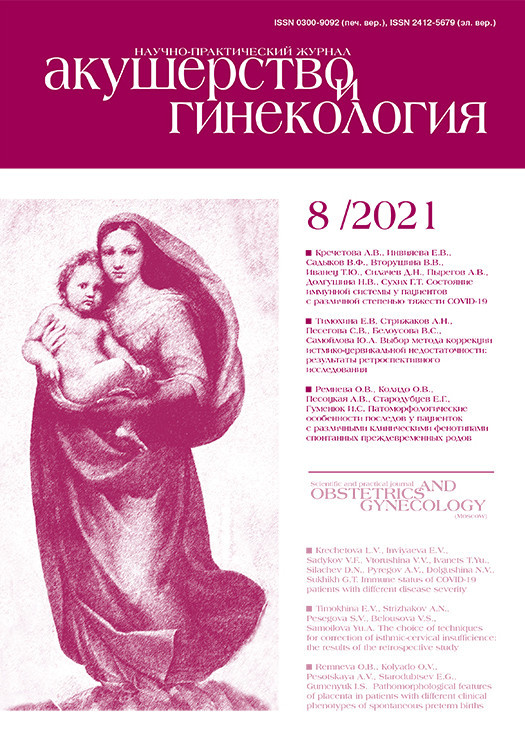
Пациентка ДАВ, 26 лет, жительница села. В анамнезе: 1 срочные роды, 1 медицинский аборт, 1 самопроизвольный выкидыш в 12 недель. Настоящая беременность 4-я, протекала без осложнений. При сроке 35–36 недель с утра перестала ощущать шевеление плода, к вечеру появились тянущие боли внизу живота и обильные кровянистые выделения из половых путей. С вышеописанными жалобами поступила в приемный покой центральной районной больницы. Диагноз при поступлении: Беременность 35–36 недель, ПОНРП, антенатальная гибель плода, постгеморрагическая анемия. Произведена операция кесарева сечения в экстренном порядке. Интраоперационно: тотальная отслойка плаценты, в полости матки жидкая кровь и сгустки общим объемом до 1500 мл, матка синюшно-черного цвета с массивными участками кровоизлияний под серозой – диагностирована матка Кувелера (рис. 1). Пациентка поставлена на учет в ККК ЦОМД, вызвана выездная бригада АРКЦ (санитарная авиация).
С учетом того, что операцию выполнял молодой врач акушер-гинеколог со стажем самостоятельной работы менее одного года, единственный на тот момент в районе, было принято совместное решение, что для проведения гистерэктомии следует дождаться врачей АРКЦ. В это время проводилась инфузионная терапия, включая введение эритроцитарной массы, сухой плазмы и утеротоников. На фоне проводимой терапии отмечалась нормализация показателей гемодинамики, матка сократилась, продолжающегося кровотечения не было. Общая кровопотеря составила 2500 мл. На момент приезда врачей АРКЦ (через 3 ч) гемодинамические и лабораторные показатели пациентки были удовлетворительными, матка хорошо сократилась, плотная, розового цвета (рис. 2).
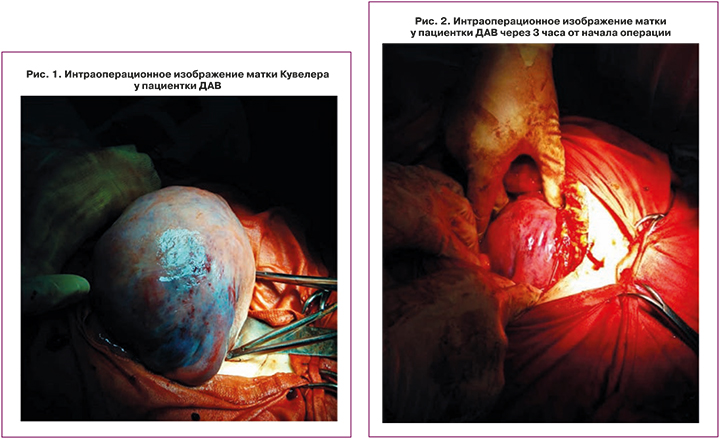
Было принято решение отказаться от проведения гистерэктомии. В первые сутки послеоперационного периода в условиях аппаратной вентиляции легких пациентка была транспортирована в отделение реанимации и интенсивной терапии ККК ЦОМД. Через 12 ч больная была экстубирована. В дальнейшем послеоперационный период протекал без осложнений, на 6-е сутки в удовлетворительном состоянии была выписана домой. Через два года у женщины наступила спонтанная беременность, успешно завершившаяся в нашем центре рождением живого доношенного ребенка путем операции кесарева сечения.
Клиническое наблюдение № 2
Пациентка ЗНВ, 38 лет. В анамнезе трое срочных родов. Настоящая беременность 4-я – спонтанная дихориальная, диамниотическая двойня. Соматический анамнез: ожирение 1–2 степени, гипертоническая болезнь 1, риск 2. Доставлена в ККК ЦОМД бригадой скорой медицинской помощи с диагнозом: Беременность 27–28 недель. Угрожающие преждевременные роды (кровянистые выделения в течение 2 ч). Объективно: матка в повышенном тонусе, умеренно болезненная при пальпации, во влагалище до 250 мл сгустков и алой крови. Диагностирована ПОНРП, что явилось показанием для экстренной операции кесарева сечения (операция начата через 18 минут от момента поступления). Интраоперационно: плацента первого плода по задней стенке, с участком отслойки и ретроплацентарной гематомой, размерами 110×60 мм; плацента второго плода по передней стенке – без особенностей; новорожденные: мальчик 1300 г, рост 42 см, оценка по шкале Апгар 3–6 баллов, и мальчик – 1100 г, рост 37 см, оценка по шкале по Апгар 3–5 баллов; оба ребенка находились на искусственной вентиляции легких. С целью профилактики кровотечения после извлечения плодов внутривенно введено 100 мг карбетоцина.
 Из протокола операции: «Матка плотная, кровотечения нет, участки багрово-синюшного цвета на передней и задней поверхности матки» (рис. 3). Интраоперационно: уровень гемоглобина – 96 г/л, фибриногена – 3,2 г/л, тромбоцитов – 140 тыс/мкл. Взята операционная пауза на 20 минут. Проводилась инфузионная терапия. Синюшность матки уменьшилась. Через 20 минут матка стала более розового цвета. При контрольном осмотре установлено, что во влагалище алая кровь до 15 мл, кровотечения из матки нет». Общая кровопотеря 1500 мл.
Из протокола операции: «Матка плотная, кровотечения нет, участки багрово-синюшного цвета на передней и задней поверхности матки» (рис. 3). Интраоперационно: уровень гемоглобина – 96 г/л, фибриногена – 3,2 г/л, тромбоцитов – 140 тыс/мкл. Взята операционная пауза на 20 минут. Проводилась инфузионная терапия. Синюшность матки уменьшилась. Через 20 минут матка стала более розового цвета. При контрольном осмотре установлено, что во влагалище алая кровь до 15 мл, кровотечения из матки нет». Общая кровопотеря 1500 мл.
Обсуждение
Согласно официальным российским рекомендациям, сохранение матки при акушерских кровотечениях допустимо только в тех случаях, когда пациентка гемодинамически стабильна и не имеет опасного для жизни кровотечения. Но даже при отсутствии эффекта от ранее проводимой терапии решение о выполнении гистерэктомии должно быть принято своевременно и коллегиально. Произвести гистерэктомию – неотложное оперативное вмешательство, направленное на спасение жизни родильницы при неконтролируемом кровотечении, врач обязан только при неэффективности предшествующих мероприятий [17].
За последние годы, благодаря научно-техническому прогрессу и внедрению в медицинскую практику, в том числе и в акушерскую, современных высокотехнологичных методов лечения, стало возможным проводить органосберегающие оперативные вмешательства даже в тех случаях, при которых ранее выполнение гистерэктомии считалось неизбежным по абсолютным показаниям [5, 13, 14, 18, 20, 21]. Так, при врастании плаценты с целью сохранения матки применяют эндоваскулярные методы гемостаза, временный дистальный гемостаз, аппаратную аутогемотрансфузию эритроцитов, компрессионные швы и метропластику; при атонии матки – современные утеротоники, различные способы деваскуляризации матки, баллонную тампонаду матки, компрессионные швы, аппаратную аутогемотрансфузию эритроцитов, рекомбинантные факторы свертывания и транексамовую кислоту; при разрывах матки основным методом оперативного вмешательства стало ушивание разрыва, а не удаление органа [22].
Когда А. Кувелер более ста лет назад впервые описал апоплексичную матку при отслойке плаценты, единственно оправданным методом спасения жизни женщины являлась гистерэктомия. Вполне естественно, что, когда появились новые технические, технологические и фармакологические возможности в арсенале современного врача-акушера, тактический подход к проведению оперативного лечения при матке Кувелера не может оставаться таким же, как сто лет тому назад.
Еще в 1997 г. Т. Eskes заявлял, что быстрое восстановление внутрисосудистого объема даже при большой кровопотере у пациенток с маткой Кувелера позволяет избежать гистерэктомии [23]. Позднее D.R. Hall (2009) показал, что быстрое оперативное родоразрешение с последующим восстановлением циркулирующего объема крови и параметров гемостаза при матке Кувелера не требует проведения гистерэктомии [24].
В последнем издании руководства по акушерству и гинекологии Williams Оbstetrics от 2018 г. говорится, что решение о тактике ведения пациентки принимается с учетом ее клинического состояния, и матка Кувелера не является абсолютным показанием к выполнению гистерэктомии [18].
Заключение
На наш взгляд, тактика врача-акушера при диагностированной во время операции кесарева сечения матке Кувелера должна быть индивидуальной и зависеть от степени тяжести состояния женщины, присоединения осложнений в виде ДВС-синдрома или геморрагического шока, а также сократительной способности матки в ответ на применение утеротонических препаратов.
Также наряду с учетом общего состояния женщины и ее желания сохранить матку являются необходимыми условиями высокий уровень оснащенности учреждения и технические возможности хирурга, что позволяет обеспечить успех оперативного вмешательства и благополучное течение послеоперационного периода.