Hysterectomy for post‑cesarean peritoneal adhesions in obese patients
Musin I.I., Berg E.A., Yashchuk A.G., Kolodyazhnaya E.A., Nasyrova S.F., Popova E.M., Molokanova A.R., Khannanov A.R.
In this article, we discuss the experience and effectiveness of endoscopic hysterectomy using a vaginal natural orifice transluminal endoscopic surgery (vNOTES) in obese patients with post-cesarean peritoneal adhesions. Performing surgery through the vagina combines the advantages of transvaginal and laparoscopic surgery, making it a potentially preferred option for patients with somatic comorbidities and a complicated obstetric and gynecological history.
Objective: To describe and illustrate the experience of performing vNOTES in obese patients undergoing hysterectomy for post-caesarean peritoneal adhesions.
Materials and methods: The authors present their experience with vNOTES for hysterectomy in 19 patients aged 42–57 years with recurrent endometrial hyperplasia, concomitant obesity, and post-cesarean pelvic adhesions. This study was conducted at the clinical facilities of the Department of Obstetrics and Gynecology No. 2 of the Bashkir SMU, Ministry of Health of Russia.
Results: The advantages of vNOTES for hysterectomy in obese patients with post-cesarean peritoneal adhesions compared with traditional laparoscopic surgery include reduced risk of trocar-related complications (which increase with obesity and the presence of peritoneal adhesions), reduced risk of postoperative complications associated with an anterior abdominal wall incision, less blood loss, better cosmetic effect due to the absence of additional abdominal wall incisions, less pain, early activation, rapid recovery, and quicker return to daily activities.
Conclusion: The vNOTES technology for hysterectomy in obese patients with post-cesarean peritoneal adhesions proves to be a minimally invasive, effective, and practical approach to surgical management in this patient population. It combines the advantages of both vaginal and laparoscopic procedures, with low blood loss and minimal intra- and post-operative complications. The benefits associated with improved visualization, increased maneuverability during manipulation, and low conversion rate make it a compelling alternative to other minimally invasive surgical approaches. However, further large-scale, multicenter, prospective, randomized controlled trials are necessary to establish clear indications and contraindications and to evaluate the efficacy, safety, and long-term outcomes of this method.
Authors' contributions: Musin I.I. – conception and design of the study, material collection; Berg E.A. – drafting of the manuscript, statistical analysis, material collection; Yashchuk A.G. – conception of the study, drafting of the manuscript, final approval for submission; Kolodyazhnaya E.A., Khannanov A.R. – material collection; Nasyrova S.F. – drafting of the manuscript, editing of the manuscript; Popova E.M., Molokanova A.R. – statistical analysis.
Conflicts of interest: The authors have no conflicts of interest to declare.
Funding: There was no funding for this study.
Ethical Approval: The study was reviewed and approved by the Research Ethics Committee of the Bashkir SMU of Minzdrav of Russia.
Patient Consent for Publication: All patients provided informed consent for the publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available upon request from the corresponding author after approval from the principal investigator.
For citation: Musin I.I., Berg E.A., Yashchuk A.G., Kolodyazhnaya E.A., Nasyrova S.F., Popova E.M., Molokanova A.R., Khannanov A.R. Hysterectomy for post-cesarean peritoneal adhesions in obese patients.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2024; (9): 81-89 (in Russian)
https://dx.doi.org/10.18565/aig.2024.143
Keywords
The first removal of the uterus via a vaginal approach was performed by Langenbeck in 1813 [1]. This method has subsequently become a widely used surgical procedure owing to its logical rationale and ease of access for organ removal. Laparoscopic access has later emerged. In 1989, Harry Reich performed the first vaginal hysterectomy using laparoscopy, followed by the first total laparoscopic hysterectomy in 1993 [2]. Minimally invasive surgery offers numerous advantages over laparotomy, making it the preferred treatment for a range of gynecological conditions. Currently, the size of the uterus is not a limiting factor in surgical treatment of patients [3].
Current recommendations from the American College of Obstetricians and Gynecologists (ACOG) and the American Association of Gynecologic Laparoscopists (AAGL) state that vaginal hysterectomy should be performed when clinically appropriate and feasible [4]. However, despite these recommendations and supporting clinical data, the rate of vaginal hysterectomies has steadily declined, coinciding with a slight decrease in the overall number of hysterectomies for benign indications, as demonstrated by researchers in the USA. The authors reported that of all hysterectomies performed for benign indications, only 12% were performed vaginally, whereas 66% were performed laparoscopically or robotically [5, 6]. Some issues contributing to the less frequent use of vaginal access include poor visibility and limited access to the anatomical structures. The literature suggests that access to ovaries and tubes can be especially difficult, with failure rates reaching up to 36% [5]. Undoubtedly, laparoscopic access provides a better anatomical overview and easier access to adjacent organs; however, it is often associated with an increased frequency of intraoperative (injury to the ureters, bladder, rectum, and vessels) and postoperative complications and conversion to laparotomy compared to vaginal access [7, 8].
Opinions vary worldwide with respect to vaginal hysterectomy and the training methods for this surgical approach. Nevertheless, it is generally recognized that vaginal surgery is a cost-effective and minimally invasive method for treating a range of gynecological diseases [9]. According to Reich, laparoscopic hysterectomy is not indicated in cases where vaginal hysterectomy is possible [10].
The advantages of vaginal access include minimal invasiveness and good cosmetic outcomes, as there is no scar on the skin of the anterior abdominal wall [10]. Patients undergoing transvaginal pelvic surgery experience a shorter hospital stay, lower pain levels, reduced narcotic requirements after surgery, and earlier return to physical activity [11]. Given these benefits, gynecologic societies should work towards achieving a consensus on the importance of prioritizing vaginal hysterectomy in both practice and physician training [5].
A novel approach to minimally invasive gynecological surgery is vaginal natural orifice transluminal endoscopic surgery (vNOTES), which integrates the benefits of the transvaginal and laparoscopic techniques. Many limitations of vaginal access, including the presence of blind instrument passages and limited vaginal space, can be overcome using vNOTES, thereby avoiding the risk of abdominal incisions associated with traditional laparoscopy [6]. Compared to standard laparoscopy, vNOTES surgery in gynecology is associated with better surgical access, less blood loss, reduced operation time, lower risk of postoperative complications, decreased postoperative pain, early activation, and rapid recovery of patients [12, 13]. This technique is particularly advantageous for obese patients because of the potential complications associated with the laparoscopic approach [14].
Every year, the number of diseases requiring uterine removal increases, partially because of an increase in somatic pathology, leading to dysfunction of the reproductive system. Obesity is one such condition. Overweight and obesity, along with associated metabolic disorders, pose a significant challenge in modern healthcare as they contribute to the development of numerous serious conditions, including gynecological conditions. Specifically, android obesity is an independent risk factor for endometrial hyperplasia and cancer [14–16].
vNOTES surgery is preferred for obese patients requiring hysterectomy for benign gynecological diseases, as it circumvents the main issues related to abdominal access in traditional laparoscopy. These issues include poor visualization (increased abdominal fat limits visualization and instrument maneuverability), prolonged operative time, possible injury to large blood vessels and internal organs, the development of postoperative hernias, and an increased rate of conversion to laparotomy. Furthermore, due to the higher burden of omental fat in obese women, subdiaphragmatic air trapping during laparoscopy can potentially lead to a greater incidence of postoperative pain [14]. The presence of adhesions between the bladder and anterior wall of the uterus following previous cesarean sections, which remains a common occurrence, also complicates laparoscopic access [17]. Peritoneal adhesions alter the topography of the pelvic organs and increase the risk of bladder and ureter injuries during subsequent surgeries, particularly in obese patients.
This study aimed to demonstrate and illustrate the experience of vNOTES for hysterectomies in obese patients with peritoneal adhesions following cesarean sections.
Materials and methods
This study was conducted from November 2022 to November 2023 at the clinical affiliates of the Department of Obstetrics and Gynecology No. 2 of Bashkir SMU, including the Gynecological Department of the Clinic of Bashkir SMU, and G.G. Kuvatov RCH. The study included 19 obese patients, aged 47–52 years, who underwent vNOTES due to the presence of peritoneal adhesions between the posterior wall of the bladder and the anterior wall of the uterus following cesarean section. A preoperative examination was conducted in accordance with the order of the Ministry of Health of Russia dated October 20, 2020, No. 1130n "On approval of the Procedure for the provision of medical care in the profile of "obstetrics and gynecology"". The indication for hysterectomy in all women was recurrent endometrial hyperplasia. Exclusion criteria were a history of retrocervical endometriosis or suspected obliteration of the posterior vaginal fornix, vaginal stenosis, presence of decompensated somatic comorbidities, and refusal to undergo hysterectomy.
The operation was performed in 2 stages. The first (vaginal) stage included posterior colpotomy, transecting the cardinal and uterosacral ligaments, and installing a port. The second stage was the endoscopic transvaginal stage, which included retrograde uterolysis of the anterior uterine wall, transection of the round ligaments, uterine arteries, proper ovarian ligaments or infundibulopelvic ligaments, revision of the pelvic organs, and mobilization of the uterus.
The primary outcomes were mean operative time and mean blood loss. Operative time was defined as the interval between the initial incision and the closure of the skin incision. The intraoperative blood loss was estimated gravimetrically. Furthermore, postoperative hemoglobin and hematocrit levels on the first postoperative day were subtracted from the baseline preoperative measurements to estimate perioperative blood loss. The surgery was conducted by an experienced endoscopist, serving as the primary surgeon, who demonstrated proficiency in vaginal hysterectomy.
Statistical analysis
Statistical analysis was conducted using the GraphPad Prism software. Statistical significance was set at p<0.05. The quantitative variables in the series of values are reported as medians with the 25th and 75th quartiles and presented as Me [Q1; Q3].
Surgical technique
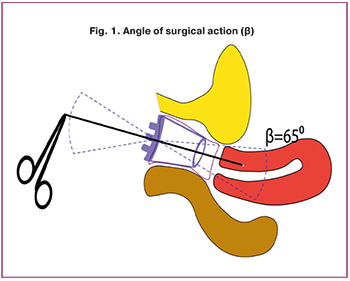
In the lithotomy position, the bladder was catheterized using the # 12 Foley catheter. Subsequently, a posterior colpotomy was performed. Then, the cardinal and uterosacral ligaments were then transected and ligated, after which a port was installed through the posterior colpotome opening. In 12 patients, the glove was fixed to the outer edge of the wound expander. A vaginal hysterectomy following a history of cesarean section presents a distinct set of characteristics: opening the peritoneum of the anterior vaginal fornix in such cases is technically difficult due to the presence of adhesions between the anterior uterine wall and posterior wall of the bladder. In this regard, a modification of the technique of the vaginal stage of vNOTES was proposed, where the port was inserted through the posterior colpotomy opening without performing anterior colpotomy and opening the vesicouterine fold. From this stage onward, the operation was performed using endovideosurgical instruments. In routine gynecological laparoscopic surgery, a laparoscope with an observation angle of 30° was used, which provided a viewing angle of 70°. The angle of operation of these devices will be equal to the viewing angle; however, because of the specific anatomy of the pelvic organs, the angle of operation may vary depending on the position of the instrument and side of the application site. The angle of the endovideosurgical surgical action for vNOTES access ensures compliance with the principles of layering of anatomical structures, which is one of the main factors for the success of this type of surgical intervention (Fig. 1) [18].
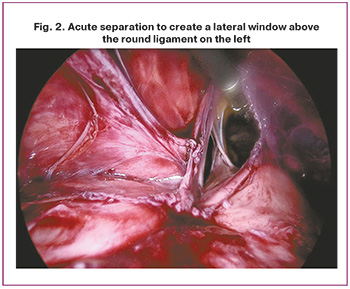
During the endoscopic transvaginal stage of the operation, the spread of the adhesion process in the small pelvis was assessed under endoscopic control. The posterior wall of the bladder and anterior wall of the uterus were determined, and adhesion dissection was commenced. Initially, our objective was to create a lateral window above the round ligament of the uterus on the left side (Fig. 2). Once this was accomplished, we separated the posterior wall of the bladder from the anterior wall of the uterus in an acute manner and freed the uterus from adhesions.
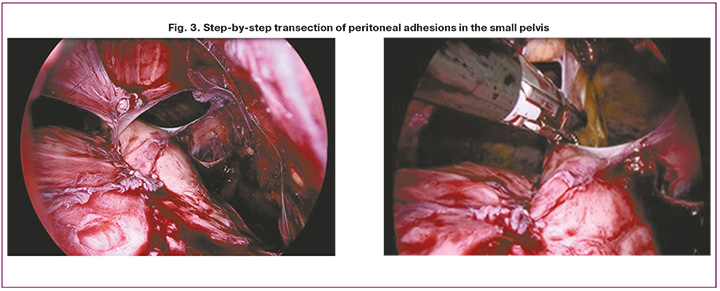
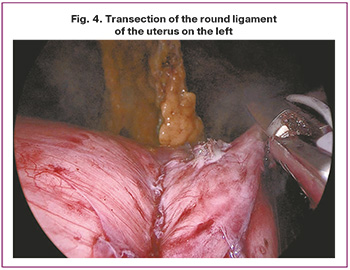
Subsequently, the anterior wall of the uterus was identified, tightness of the bladder was assessed, and peritoneal adhesions in the small pelvis were crossed gradually (Fig. 3). Subsequently, the paravesicular spaces on both sides were separated to the level of the anterior vaginal fornix, after which the round ligament of the uterus on the right, uterine arteries, proper ligaments of the ovary, or infundibulopelvic ligaments were transected. Subsequently, the pelvic organs and abdominal cavity were examined for hemostasis. The round ligament of the uterus on the left side was then transected to mobilize the uterus (Fig. 4).
Results and discussion
The average age of the patients who underwent surgery at the time of the study was 52.0 [47.0; 62.0] years, and the average parity was 2.0 [1.0; 3.0]. The body mass index in women was on average 33.8 [27.6; 35.2] kg/m2. Overweight was observed in 5/19 (26.3%) patients, grade I obesity was diagnosed in 6/19 (31.6%) women, and grades II and III obesity were observed in 4/19 (21.1%) study participants. Among extragenital comorbidities, hypertension was recorded in 15/19 (78.9%) women and type II diabetes mellitus was found in 10/19 (52.6%). The average age of menarche in patients included in the study was 12.0 [12.0; 13.0] years; in most women, menstruation in the past was regular (15/19, 78.9%), painless (16/19, 84.2%), and moderate (17/19, 89.5%). The average age of menopause was 50.0 [47.0; 52.0] years. At the time of surgery, 17/19 (89.5%) women were menopausal, and 2/19 (10.5%) were in perimenopause. Most postmenopausal women had no complaints; 2/19 (10.5%) patients had spotting bloody discharge from the genital tract, and 2/19 (10.5%) had abnormal uterine bleeding during the transitional period. All patients had a history of diagnosis of "N85.0 Glandular hyperplasia of the endometrium.” The indication for surgical treatment was the repeated detection of endometrial hyperplasia according to histological examination in accordance with the current clinical guidelines [16]. In all cases, hysterectomy was performed using vNOTES. Among the concomitant gynecological pathologies, uterine myoma was most often observed, in 12/19 (63.2%) patients, adenomyosis was recorded in 3/19 (15.7%), ovarian cyst in 2/19 (10.5%). Four of the 19 women (21.1%) had a history of abdominal surgery. All the patients had a history of cesarean section. Of the 19 women, 15 (78.9%) underwent a lower segment cesarean section, while 4 (21.1%) had a classic cesarean section. Anesthetic care for all women included endotracheal anesthesia. No instances of anesthetic complications were observed. The intraoperative blood loss was 147.0 ml (120.0; 180.0), with operation time of 85.0 minutes (64.0; 110.0). The average decrease in hemoglobin level was 12 g/l. The average weight of the removed uterus was 265.0 [155.0; 830.0] g (Fig. 5).
In 5/19 (26.3%) cases, the uterine weight was up to 200.0 g, in 11/19 (57.9%) women from 201.0 to 500.0 g, in 3/19 (15.8%) >501.0 g. In none of the cases was there a record of intraoperative complications, such as injury to the ureter, intestine, bladder, major branches of arteries, and veins; there were no cases of conversion to laparotomy.
No complications, including infectious complications, were observed in the postoperative period. The average length of hospital stay was 3.0 [3.0; 5.0] days, and scores of pain syndrome after surgery on the 1st, 2nd, 3rd day, according to the visual analog scale (VAS) of pain, were estimated at 3.0 [3.0, 5.0], 2.0 [1.0; 2.0], 1.0 [0.0; 1.0] points, respectively.
Histological examination of the removed uterus showed endometrial hyperplasia without atypia in 12/19 (63.2%) women, and atypical endometrial hyperplasia was detected in 7/19 (36.8%). All women were discharged in a satisfactory condition with full recovery. Clinical experience has demonstrated that vaginal access is preferable for hysterectomy in obese patients with peritoneal adhesions after cesarean section compared with other methods. This is due to the fact that vaginal access is safer, allows for the minimization of the scope of surgical access, reduces the time of hospital stay and operation time, and also accelerates recovery. Conventional laparoscopic hysterectomy can prove challenging in this patient population owing to restricted visualization, prolonged surgical time, elevated risk of organ and vessel injury, and other factors [8].
Transvaginal vNOTES operations can significantly expand the scope of gynecological operations with vaginal access, using the advantages of endoscopy owing to better visualization of the surgical field and manipulations that may be limited by vaginal access [7, 8]. In our case series, all hysterectomies were performed by using vNOTES.
A comparative analysis of the literature and our experience indicated that the average blood loss was lower with vNOTES than with traditional laparoscopy, whereas the operative time remained similar [20]. In staged vNOTES surgery, the vessels supplying the uterus are ligated vaginally before any manipulation, thereby reducing intraoperative blood loss. According to the available publications, vNOTES enables hysterectomies without conversion and is associated with less pain, fewer intra- and postoperative complications, and shorter hospital stays compared to laparoscopy [21, 22]. Additionally, recent studies have reported favorable outcomes for vNOTES regarding conversion and complication rates in patients with large uterine volumes (>280 g) [23]. In our study, we also removed the large uteri; in three cases, the weight of the removed organs exceeded 500 g. Furthermore, none of the patients who underwent vNOTES hysterectomy required conversion to a standard laparoscopy or laparotomy. Our results confirmed the advantages of minimally invasive vNOTES hysterectomy in the studied patient population: low blood loss during surgery, absence of trocar-associated and postoperative complications related to an incision on the anterior abdominal wall, reduced need for pain relief in the postoperative period, early patient mobilization, rapid recovery, and cosmetic benefits owing to the lack of additional incisions on the abdominal wall [13, 21]. It is well known that early mobilization enhances respiratory function, reduces muscle weakness, and decreases the risk of thromboembolic complications [24]. In our study, patients were verticalized one hour after surgery, which positively affected postoperative rehabilitation. For this purpose, we applied the principles of fast-track surgery [24]. Patients were discharged on an average on the 3rd day after surgery, following clinical, laboratory, and instrumental examinations. The absence of an abdominal wall incision alleviated the pain and facilitated early postoperative activation. In our patients who underwent vNOTES hysterectomy, the average postoperative pain score according to VAS was 3.0 points, which aligns with the literature [7, 20]. Other studies suggest that vNOTES technology allows the treatment of a large number of patients in a hospital or outpatient setting as early as the first day after surgery [20, 22]. However, considering our initial experience with the vNOTES procedure in women with peritoneal adhesions following cesarean sections, along with concomitant extragenital diseases such as obesity, diabetes mellitus, and hypertension, which are associated with a higher frequency of infectious postoperative complications, bleeding, and thromboembolic events, we opted to discharge the patients on the 3rd day.
Despite its numerous advantages, vNOTES surgery has limitations, including difficult access in patients with a narrow vagina, retrocervical endometriosis, or suspected obliteration of the posterior vaginal fornix [6]. Our experience highlights the need for careful patient selection when using vNOTES for hysterectomies considering the indications and contraindications for this procedure. In addition, the surgeon performing the operation using this technology must be proficient in both laparoscopy and vaginal surgery. vNOTES requires specialized skills, experience, knowledge, and training. Although vNOTES is gaining popularity as a minimally invasive procedure, its technical complexity limits its widespread use compared with traditional laparoscopy. According to the literature, a well-trained endoscopist can achieve surgical competence in performing vNOTES for hysterectomy after 20 or, according to earlier studies, after 100 cases [22, 25]. These results suggest the feasibility of incorporating vNOTES technology into the training of obstetricians and gynecologists, alongside traditional methods.
The use of vNOTES for hysterectomy in patients with obesity and adhesions is a relatively new minimally invasive "surgery without sutures. Large-scale studies comparing vNOTES with traditional laparoscopy are required to establish its effectiveness and safety.
Conclusion
vNOTES represents a new era of minimally invasive surgery that combines the advantages of both vaginal and laparoscopic techniques, while maintaining low blood loss and minimal intraoperative and postoperative complications. In the future, it may emerge as the most promising direction for surgical gynecology. One of the main factors influencing the performance of pelvic organ surgeries is adherence to the principles of layering anatomical structures, and the vNOTES approach allows for compliance monitoring. This method is preferred for hysterectomy in obese patients with peritoneal adhesions after cesarean section. The advantages associated with improved visualization, increased maneuverability during manipulations, and a low conversion rate make vNOTES a compelling alternative to other minimally invasive surgical methods. However, further large-scale, multicenter, prospective, randomized controlled trials are needed to address these limitations, standardize techniques, establish clear indications and contraindications, evaluate efficacy and safety, and most importantly, assess the long-term outcomes of this technique, which are critical for establishing vNOTES as a reliable and preferred surgical option for this complex patient population.
References
- Cohen S.L., Einarsson J.I. Total and supracervical hysterectomy. Obstet. Gynecol. Clin. North Am. 2011; 38(4): 651-61. https://dx.doi.org/10.1016/j.ogc.2011.09.002.
- Hawe J.A., Garry R. Laparoscopic hysterectomy. Semin. Laparosc. Surg. 1999; 6(2): 80-9. https://dx.doi.org/10.1053/SLAS00600080.
- Eltabbakh G.H., Gregoire S., Eltabbakh G.D. Minimally invasive hysterectomy for the large uterus using the LigaSure. J. Gynecol. Obstet. 2022; 10(4): 203-210. https://dx.doi.org/10.11648/j.jgo.20221004.17.
- Committee Opinion No. 701 Summary: Choosing the route of hysterectomy for benign disease. Obstet. Gynecol. 2017; 129(6): 1149-50. https://dx.doi.org/10.1097/AOG.0000000000002108.
- Moen M., Walter A., Harmanli O., Cornella J., Nihira M., Gala R. et al.; Society of Gynecologic Surgeons Education Committee. Considerations to improve the evidence-based use of vaginal hysterectomy in benign gynecology. Obstet. Gynecol. 2014; 124(3): 585-8. https://dx.doi.org/10.1097/AOG.0000000000000398.
- Halder G., Ferrando C., Kho R., Elhenawy C., Grimes C., Balgobin S. et al. The SAVVy study: SGS/AAGL survey of barriers for vaginal access surgery. Am. J. Obstet. Gynecol. 2024; 230(4): S1153-S1154.
- Мусин И.И., Ящук А.Г., Колодяжная Е.А., Насырова С.Ф., Галанова З.М., Молоканова А.Р., Имельбаева А.Г. Транслюминальная эндоскопия (vNOTES): тотальная гистерэктомия. Акушерство и гинекология. 2024; 4: 126-31. [Musin I.I., Yashchuk A.G., Kolodyazhnaya E.A., Nasyrova S.F., Galanova Z.M., Molokanova A.R., Imelbaeva A.G. Transluminal endoscopy (vNOTES): total hysterectomy. Obstetrics and Gynecology. 2024; (4): 126-31. (in Russian)]. https://dx.doi.org/10.18565/aig.2023.305.
- Волков О.А., Шрамко С.В., Ренге Л.В., Салтыкова П.Е., Сабанцев М.А., Шишея Е.Ю., Коваль Е.Ю., Власенко А.Е., Чубарь Е.А. Осложнения лапароскопической гистерэктомии: поиск факторов риска. Акушерство и гинекология. 2022; 9: 122-8. [Volkov O.A., Shramko S.V., Renge L.V., Saltykova P.E., Sabantsev M.A., Shisheya E.Yu., Koval E.Yu., Vlasenko A.E., Chubar E.A. Complications of laparoscopic hysterectomy: search for risk factors. Obstetrics and Gynecology. 2022; (9): 122-8. (in Russian)]. https://dx.doi.org/10.18565/aig.2022.9.122-128.
- Bangura M., Ganyaglo G., Kupualor D., Lawrence E., Rooney D., Schmidt P. Introduction of fundamentals of vaginal surgery to west african obstetrics and gynecology trainees. Am. J. Obstet. Gynecol. 2024; 230(4, Suppl.):S1208-S1209.
- Елисеев Д.Э., Холодова Ж.Л., Доброхотова Ю.Э., Овчаренко Д.В., Холодова Я.Г. Безопасная гистерэктомия. Кремлевская медицина. Клинический вестник. 2023; 1: 61-71. [Eliseev D.E., Kholodova Z.L., Dobrokhotova Y.E., Ovcharenko D.V., Kholodova Y.G. Safe hysterectomy. Kremlin Medicine Journal. 2023; (1): 61-71. (in Russian)].
- Ramaseshan A.S. Tunitsky-Bitton E., O'Sullivan D.M., Reagan K.M.L., Steinberg A.C. Predictive factors of postdischarge narcotic use after female pelvic reconstructive surgery. Female Pelvic Med. Reconstr. Surg. 2019; 25(2): e18-e22. https://dx.doi.org/10.1097/SPV.0000000000000686.
- Karakaş S., Kaya C., Yildiz Ş., Alay İ., Durmuş U., Aydiner İ.E. et al. Comparison of vNOTES technique with conventional laparoscopy in gynecological emergency cases. Minim. Invasive Ther. Allied Technol. 2022; 31(5): 803-9. https://dx.doi.org/10.1080/13645706.2021.2025111.
- Lerner V.T., May G., Iglesia C.B. Vaginal natural orifice transluminal endoscopic surgery revolution: the next frontier in gynecologic minimally invasive surgery. JSLS. 2023; 27(1): e2022.00082. https://dx.doi.org/10.4293/JSLS.2022.00082.
- Mohr-Sasson A., Hui M., Bonilla Moreno M., Bhalwal A., Montealegre A. Pain following vaginal natural orifice transluminal endoscopic surgery (vNOTES) in obese compared to non-obese women. Am. J. Obstet. Gynecol. 2024;230(4, Suppl.): S1182.
- Горбатов С.Ю., Нечаев О.И., Подчернина А.М., Швец Ю.Ю. Экономика ожирения. Экспертный обзор. М.: ГБУ «НИИОЗММ ДЗМ»; 2022. 34 с. [Gorbatov S.Yu., Nechaev O.I., Podchernina A.M., Shvets Yu.Yu. Economics of obesity. Peer review. Moscow; 2022. 34 p. (in Russian)].
- Министерство здравоохранения Российской Федерации. Клинические рекомендации. Гиперплазия эндометрия. 2021. 45 с. [Ministry of Health of the Russian Federation. Clinical guidelines. Endometrial hyperplasia. 2021. 45 p. (in Russian)].
- Аржаева И.А., Тяпкина Д.А., Тараскин А.Ф., Тараскин А.А. Частота встречаемости спаечного процесса брюшной полости после кесарева сечения (по результатам повторных оперативных вмешательств). Международный научно-исследовательский журнал. 2022; 3: 102-7. [Arzhaeva I.A., Tyapkina D.A., Taraskin A.F., Taraskin A.A. Frequency of occurrence of the adhesive process of the abdominal cavity after cesarean section (according to the results of repeated surgery). International Research Journal. 2022; (3): 102-7. (in Russian)]. https://dx.doi.org/10.23670/IRJ.2022.117.3.017.
- Прудков М.И. Основы минимально-инвазивной хирургии. Екатеринбург; 2007. 64 с. [Prudkov M.I. Fundamentals of minimally invasive surgery. Yekaterinburg; 2007. 64 p. (in Russian)].
- King L., Pan E., Hamid C., Balgobin S. Vaginal colpotomy for traditional and natural orifice transluminal endoscopic surgery (NOTES) vaginal procedures Am. J. Obstet. Gynecol. 2024; 230(4, Suppl.): S1291-S1292.
- Interdonato M.L., Scollo P., Bignardi T., Massimello F., Ferrara M., Donatiello G. et al. Hysterectomy by transvaginal natural orifice transluminal endoscopic surgery: An Italian initial experience. Front. Med. (Lausanne). 2022; 9: 1018232. https://dx.doi.org/10.3389/fmed.2022.1018232.
- Baekelandt J.F., De Mulder P.A., Le Roy I., Mathieu C., Laenen A., Enzlin P. et al. Hysterectomy by transvaginal natural orifice transluminal endoscopic surgery versus laparoscopy as a day-care procedure: A randomised controlled trial. BJOG. 2019; 126(1): 105-13. https://dx.doi.org/10.1111/1471-0528.15504.
- Kim J.C., Yim G.W., Kim Y.T. Clinical relevance of vaginal natural orifice transluminal endoscopic surgery (vNOTES) in gynecology. Obstet. Gynecol. Sci. 2024; 67(2): 199-211. https://dx.doi.org/10.5468/ogs.23205.
- Kheirbek N., Delporte V., El Hajj H., Martin C., Delplanque S., Kerbage Y. et al. Comparing vNOTES hysterectomy with laparoscopic hysterectomy for large uteri. J. Minim. Invasive Gynecol. 2023; 30(11): 877-83. https://dx.doi.org/10.1016/j.jmig.2023.06.019.
- Торубаров С.Ф., Духин А.О., Чмыр Е.Н. Fast Track в гинекологии: реалии сегодняшнего дня. Акушерство и гинекология. 2019; 10: 60-5. [Torubarov S.F., Dukhin A.O., Chmur E.N. Fast track in gynecology: today’s realities. Obstetrics and Gynecology. 2019; (10): 60-5. (in Russian)]. https://dx.doi.org/10.18565/aig.2019.10.60-65.
- Wang C.J., Go J., Huang H.Y., Wu K.Y., Huang Y.T., Liu Y.C. et al. Learning curve analysis of transvaginal natural orifice transluminal endoscopic hysterectomy. BMC Surg. 2019; 19(1): 88. https://dx.doi.org/10.1186/s12893-019-0554-0.
Received 19.06.2024
Accepted 02.08.2024
About the Authors
Ilnur I. Musin, Dr. Med. Sci., Professor at the Department of Obstetrics and Gynecology №2, Bashkir State Medical University, Ministry of Health of Russia,450008, Russia, Ufa, Lenin str., 3, +73472649650, ilnur-musin@yandex.ru, https://orcid.org/0000-0001-5520-5845
Alfiya G. Yashchuk, Dr. Med. Sci., Professor, Head of the Department of Obstetrics and Gynecology №2, Bashkir State Medical University, Ministry of Health of Russia, 450008, Russia, Ufa, Lenin str., 3, +73472649650, alfiya_galimovna@mail.ru, https://orcid.org/0000-0003-2645-1662
Elena A. Kolodyazhnaya, Clinical Resident at the Department of Obstetrics and Gynecology №2, Bashkir State Medical University, Ministry of Health of Russia,
450008, Russia, Ufa, Lenin st., 3, +79174218784, elena_l_a@list.ru, https://orcid.org/0000-0001-5133-7293
Edvard A. Berg, PhD, Associate Professor at the Department of Obstetrics and Gynecology №2, Bashkir State Medical University, Ministry of Health of Russia,
450008, Russia, Ufa, Lenin str., 3, +79273379003, nucleardeer@mail.com, https://orcid.org/0000-0002-2028-7796
Svetlana F. Nasyrova, PhD, Associate Professor at the Department of Obstetrics and Gynecology №2, Bashkir State Medical University, Ministry of Health of Russia,
450008, Russia, Ufa, Lenin str., 3, +73472649650, ufa863@mail.ru, https://orcid.org/0000-0002-2313-7232
Elena M. Popova, Teaching Assistant at the Department of Obstetrics and Gynecology №2, Bashkir State Medical University, Ministry of Health of Russia,
450008, Russia, Ufa, Lenin str., 3, +79871335969, kafedraagidpo2@mail.ru, https://orcid.org/0000-0001-7298-3489
Angela R. Molokanova, PhD student at the Department of Obstetrics and Gynecology №2, Bashkir State Medical University, Ministry of Health of Russia,
450008, Russia, Ufa, Lenin str., 3, +79297557755, angella1210@mail.ru, https://orcid.org/0000-0003-1115-6775
Arslan R. Khannanov, 4th year student of the Faculty of Dentistry, Bashkir State Medical University, Ministry of Health of Russia, 450008, Russia, Ufa, Lenin str., 3, +73472649650, arslan1804@yandex.ru, https://orcid.org/0009-0009-5974-8420



