New approaches to the treatment of post-cesarean endometritis
Barinov S.V., Tirskaya Yu.I., Kan N.E., Tyutyunnik V.L., Lazareva O.V., Kadtsyna T.V., Khoroshkin E.A., Blauman E.S., Shkabarnya L.L., Pyanova L.G.
Objective: To enhance treatment outcomes for patients with postpartum endometritis using molded carbon polyvinylpyrrolidone-modified sorbent VNIITU-1 PVP, in conjunction with irrigation of the uterine cavity using antiseptic solutions cavitated by low-frequency ultrasound.
Materials and methods: This retrospective, randomized controlled study included 124 patients with postpartum endometritis. Patients in group A (n=48) received injections of molded carbon polyvinylpyrrolidone-modified sorbent (VNIITU-1 PVP) into the uterine cavity. The patients in group B (n=61) received traditional antibacterial therapy. Patients in group C (n=15) underwent combined irrigation of the uterine cavity with an antiseptic solution cavitated using low-frequency ultrasound, followed by intrauterine administration of the modified sorbent.
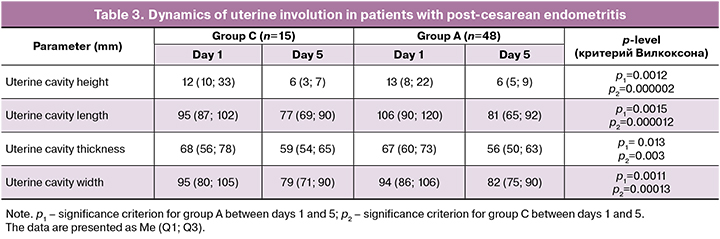
Results: A comprehensive approach using the modified sorbent VNIITU-1 PVP resulted in a 5.9-fold reduction in TNF-α levels and a 5.6-fold reduction in IL-1β levels in the endometrial aspirate (p<0.05) in group A, which was more effective than that in group B. In group A, hysterectomy was performed in 1 case compared to 14 cases in group B (χ2 =3.904, p<0.05). In group C, ultrasound results indicated that by the 5th day, the involutional processes of the uterus were more pronounced than those in group A.
Conclusion: Solutions cavitated with low-frequency ultrasound enhanced the contractile ability of the uterus and created optimal conditions for the effective sorption of pathogenic microorganisms, toxins, and their decay products by the modified molded sorbent VNIITU-1 PVP.
Authors' contributions: Barinov S.V. – conception and design of the study; Blauman E.S. – material collection and processing, statistical analysis; Shkabarnya L.L., Khoroshkin E.A. – clinical work; Blauman E.S., Barinov S.V. – drafting of the manuscript; Tirskaya Yu.I. – drafting of the manuscript, editing of the manuscript; Barinov S.V., Lazareva O.V., Pyanova L.G., Kadtsyna T.V., Kan N.E., Tyutyunnik V.L. — data interpretation, editing of the manuscript.
Conflicts of interest: The authors have no conflicts of interest to declare.
Funding: There was no funding for this study.
Ethical Approval: The study was reviewed and approved by the Research Ethics Committee of the Omsk State Medical University, Ministry of Health of the Russian Federation (protocol No. 140, dated October 13, 2021).
Patient Consent for Publication: All patients provided informed consent for the publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available upon request from the corresponding author after approval from the principal investigator.
For citation: Barinov S.V., Tirskaya Yu.I., Kan N.E., Tyutyunnik V.L., Lazareva O.V., Kadtsyna T.V., Khoroshkin E.A., Blauman E.S., Shkabarnya L.L., Pyanova L.G. New approaches to the treatment of post-cesarean endometritis.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2025; (4): 52-60 (in Russian)
https://dx.doi.org/10.18565/aig.2024.315
Keywords
Infectious and inflammatory complications during the postpartum period account for a significant percentage of morbidity among postpartum women [1–3]. Specifically, the incidence of postpartum endometritis following natural childbirth ranges from 2% to 5%. As the number of operative deliveries increases from 20% to 30%, the risk of postpartum infectious and inflammatory diseases also increases.
Improvements in surgical techniques and early detection of postpartum complications have contributed to a decrease in severe forms of postpartum purulent-septic complications such as peritonitis and sepsis, which now occur in less than 2% of cases. However, these complications significantly affect maternal mortality statistics [4–9].
Infectious agents are the leading cause of postpartum complications is attributed to infectious agents [10–12]. Currently, opportunistic microflora that possess antibiotic resistance play a critical role in these infections [4, 13–15]. These so-called "superbugs" are increasingly significant in the context of postpartum infectious complications.
However, Russian statistics do not accurately reflect the extent of antibiotic resistance in the country. In contrast, European data indicate an annual mortality of 23,000–25,000 patients due to infections caused by resistant bacteria, which is comparable to the scale of a pandemic, underscoring the importance of this issue in medicine. Furthermore, the evolution of microorganisms in the development and transmission of resistance mechanisms has drastically reduced the availability of effective drugs. Alarmingly, no new antibacterial drug has been developed over the past 30 years.
Modern obstetrics faces the critical challenge of preserving reproductive function and maintaining the uterus as an organ. The increasing resistance of pathogenic and opportunistic microflora to antibacterial drugs, coupled with the rising frequency of operative deliveries, necessitates the enhancement of treatment strategies and exploration of additional methods to combat resistant microorganisms.
Direct drug delivery to the inflammation site is of particular interest. The technique of vulnerosorption and irrigation of the uterine cavity with antiseptic solutions (such as chlorhexidine, betadine, and furacilin) treated with low-frequency ultrasound has shown promise and has been integrated into clinical obstetric and gynecological practice [16, 17].
In light of the above, improving the management of women in labor with postpartum infectious and inflammatory diseases is essential for enhancing treatment outcomes for postpartum endometritis.
This study aimed to refine the treatment method for patients with post-cesarean endometritis by employing a combined approach that includes irrigating the uterine cavity with antiseptic solutions cavitated by low-frequency ultrasound, followed by intrauterine administration of the molded carbon sorbent, VNIITU-1 PVP.
Materials and methods
The study was conducted at the Omsk Regional Clinical Hospital from 2017 to 2023 and involved 124 patients diagnosed with post-cesarean endometritis.
On admission, all postpartum women underwent uterine cavity aspiration for culture, pathogen identification, and drug susceptibility testing. Before receiving culture results, empirical antibacterial therapy was initiated with broad-spectrum drugs, specifically cefazolin (1 g), administered three times daily, in accordance with clinical recommendations. Following the receipt of culture results and the evaluation of therapeutic effectiveness, treatment was adjusted based on the sensitivity of the cultured pathogenic microflora.
Patients with post-cesarean endometritis (n=124) were divided into three groups based on the treatment method.
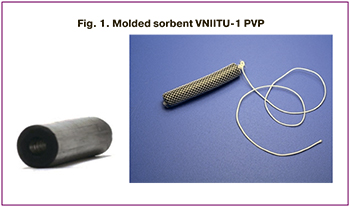
In group A (n=48), a molded carbon sorbent modified with polyvinylpyrrolidone (PVP), developed by the Center for New Chemical Technologies at the Institute of Catalysis, Siberian Branch of the Russian Academy of Sciences (patent No. 2646496 dated 10.01.2017), was administered intrauterine along with systemic antibacterial therapy. The sorbent, shaped like a hollow cylinder measuring 40×5 mm with rounded edges and one internal channel of circular cross-section (Fig. 1), was retained in the uterus for 24 h before replacement. Five sessions were conducted in total. The sorbent was registered for use in the Russian Federation under certificate No. RZN 2015/2969, dated 14.08.2015, with a toxicological report dated 14.08.2013 (No. 2099.013P).
Patients in group B (n=61) received antibacterial therapy only.
In addition to antibiotic therapy, patients in group C (n=15) underwent cavitation of the uterine cavity with a 0.02% furacilin solution for 3–5 min using a volume of 100–150 ml. The FOTEK device, ACTITON-A model (Fig. 2), was used for this procedure. After irrigating the uterine cavity with the cavitated antiseptic solution and removing the inflammatory substrate, the molded carbon sorbent VNIITU-1 PVP was introduced. This sorbent was retained for 24 h before its removal, and the total duration of therapy was five days.

The criteria for evaluating therapeutic effectiveness included improvements in laboratory parameters, ultrasound diagnostic data, and number of hysterectomies performed in the observed groups.
Clinical evaluations included cultures of aspirate from the uterine cavity; general blood tests; and measurements of tumor necrosis factor alpha (TNFα), interleukin (IL)-1β, and IL-10 levels in peripheral blood and aspirate from the uterine cavity (Vector-Best JSC, Russia). All patients underwent hysteroscopy and ultrasound examinations to assess the length, width, and thickness of the uterus as well as to calculate the cavity volume. Hysteroscopy facilitated timely diagnosis of the inflammatory process, necrotic changes, and suture failure, enabling prompt surgical correction. To assess the dynamics of laboratory and instrumental parameters, follow-up studies were conducted upon admission and on days 1, and five days after the initiation of therapy.
To prevent contamination from the vaginal and cervical flora during aspiration from the uterine cavity, a sterile aspiration device was used.
The study was reviewed and approved by the Research Ethics Committee of the Omsk State Medical University of the Ministry of Health of the Russian Federation (No. 140, dated October 13, 2021), in accordance with the biomedical ethics requirements outlined in the Helsinki Declaration of the World Medical Association (1964, amended in 2008).
Statistical analysis
Statistical analysis was performed using STATISTICA 10.0. The Shapiro-Wilk test assessed the normality assumption, revealing a predominantly non-normal distribution; thus, non-parametric methods were employed. Differences between the two groups were analyzed using the Mann–Whitney U test. Continuous variables are presented as median (Me) with interquartile range (Q1; Q3) in format Me (Q1; Q3). A comparative analysis of the dynamic changes between days 1 and 5 was conducted using the Wilcoxon test.
Results
The ages of the patients included in the study ranged from 15 to 47 years, with a mean age of 26 (6.3) years. The study groups were comparable in age, somatic disease, and laboratory and clinical manifestations [18].
The highest rate of postpartum endometritis (55/124 (44.4%)) was observed after delivery in level I hospitals. In 48/124 (38.7%) cases, endometritis developed in level III hospitals. The least frequent infectious complications after delivery were observed in level II maternity hospitals – 21/124 (16.9%).
In 53/124 (42.7%) cases, the disease manifested itself 10 days after delivery. The first symptoms of postpartum endometritis in 33/124 (26.6 %) patients appeared in the first five days. In the interval from 5 to 10 days postpartum, endometritis was diagnosed in 38/124 (30.6%) patients. This analysis showed that postpartum women were admitted to the hospital from home more often (73.3%).
The analysis of the main complaints on admission showed that the most common symptoms were febrile temperature (32/124, 54.8%), subfebrile temperature – 24/124 (19.5%), purulent lochia – 49/124 (39.5%), and lower abdominal pain – 11/124 (8.9%). A quarter of the patients (32/124 (25.8%)) had normal body temperature on admission, and 4.8% complained of abundant bloody discharge. Ultrasound examination of postpartum women with post-cesarean endometritis showed that 66/154 (54.8%) women had diffuse myometrial changes, 27/124 (22.6%) had the uterine cavity filled with heterogeneous contents, and 31/124 (25.8%) had a "niche" symptom in the area of the postoperative suture. Hysteroscopy revealed that in 29/124 (23.4%) cases, the uterine cavity was filled with blood clots; in 19/124 (15.3%) patients, an accumulation of small gas bubbles was observed in the suture area; in 14/124 (11.3%) cases, necrosis of the decidual tissue and the suture area was detected; in 8/124 (6.4%) women, the sutures hung freely in the uterine cavity; in 2.4%, a funnel-shaped defect was found in the suture area.
Analysis of the results of bacteriological cultures from the uterine cavity of patients with post-cesarean endometritis showed that, in terms of frequency of occurrence, E. coli colonies were found first in 43.1% of cases, followed by S. epidermidis (39.6%), E. faecalis (22.4%), and Acinetobacter baumannii (10.34%) (Fig. 3). The association of several microorganisms occurred in 53.2% of the cases. The most frequent (23.4% of cases) was the association of E. faecalis with Staphylococcus spp. microorganisms, which was slightly less frequent (18.5%) with the gram-negative bacillus E. coli.
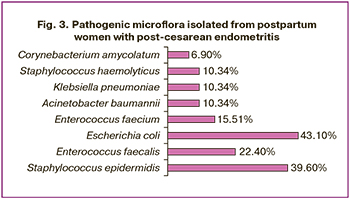
Analysis of the resistance of the sown pathogenic microflora showed that A. baumannii had the highest antibiotic resistance, being insensitive to carbapenems, fluoroquinolones, cephalosporins in 100% of cases, and aminoglycosides in 84.2%. E. coli showed resistance to the cephalosporin group in 65.9% of cases, to penicillins with a beta-lactamase inhibitor (amoxicillin clavulanate) in 40.9% of cases, to aminoglycosides in 27.2%, to penicillin antibiotics in 18.2%, and to fluoroquinolones in 15.9%. E. coli remained sensitive to carbapenems in 97.7% of cases. S. epidermidis was resistant to cephalosporins in 30.2% of cases, to clindamycin in 22.2%, while in 89% it was sensitive to aminopenicillins and carbapenems. Against the background of antibacterial therapy conducted in combination with intrauterine sorption with the carbon sorbent VNIITU-1 PVP in group A, 39/63 (62.5%) postpartum women showed an improvement in clinical symptoms. In 37.5% of the cases (23/63), there was a need for reconstructive plastic surgery due to uterine suture failure diagnosed according to hysteroscopy data. The scope of the surgical intervention included suture excision and secondary uterine sutures. One patient underwent organ removal surgery due to progression of the inflammatory process, while in group B, disease progression occurred in 14/61 (22.9%) women.
Analysis of the results of laboratory diagnostic tests showed that after 5 days of sorbent therapy in group A, leukocytosis decreased by 1.4 times, while band neutrophils decreased by 2 times (p<0.05) (Table 1).

To assess the effectiveness of the therapy, a study on uterine cavity contamination was conducted in the study groups. After using the sorbent in group A, microflora growth was not detected in 89% of the subjects; only 11% of the cases showed moderate growth of pathogens. While in group B, on the 5th day of treatment, massive microbial growth persisted in 36% of cases, and the average level of contamination was in 21.3% of patients.
Considering that after antibacterial and sorption therapy in group A, moderate microbial growth in the aspirate from the uterine cavity persisted in 11.1% of cases, we identified group C (n=15) to improve the results of post-cesarean endometritis treatment. Patients in this group underwent combined therapy: before the introduction of the molded sorbent VNIITU-1 PVP, the uterine cavity was irrigated with furacilin solution using cavitated low-frequency ultrasound.
The cultures taken on the 5th day of therapy showed a 100% absence of pathogens in the uterine cavity.
A significant decrease in the concentrations of IL-10, proinflammatory cytokines, and C-reactive protein was noted against the background of the treatment in all observed groups (Table 2). In groups A and C, the level of IL-1β decreased by 5.5 times. The TNFα level decreased by a maximum of 10 times in group C and 5.8 times in group A. At the same time, in group B, pro-inflammatory cytokines decreased to a lesser extent: IL-1β – 2.3 times (p=0.00036), and no significant decrease in TNFα was recorded (p=0.8107). The concentration of pro-inflammatory IL-10 also decreased against the background of the treatment in all groups: 2.8 times in group A, 6.5 times in group C, which can be associated with its partial sorption by the carbon sorbent. The maximum decrease in this indicator by 7.8 times was recorded in group B, where only antibacterial therapy was administered (Table 2). A marked decrease in the concentration of IL-10 and the absence of a clear tendency toward a decrease in pro-inflammatory cytokines against the background of persistent growth of microflora in the uterine cavity in 57.3% of patients in group B indicates the absence of a tendency for early recovery.
The results of the ultrasound examination on the 1st and 5th day of treatment showed significant positive dynamics of uterine involution in groups A and C (Table 3). All measured indicators of the external size of the uterus (length, width and thickness) decreased in both groups by 1.2 times, and the height of the uterine cavity – by 2–2.2 times. Thus, complex antibacterial treatment of postpartum endometritis, supplemented by the use of an intrauterine carbon sorbent in combination (or without) with cavitation of the uterine cavity with an antiseptic solution, increases the contractile capacity of the myometrium and promotes rapid and complete involution.
Discussion
The study revealed that one of the most common complications of operative delivery is endometritis, which can lead to generalized infection and the development of septic complications extending beyond the uterus, such as parametritis, pelvic peritonitis, and peritonitis [19]. Consequently, the search for new methods to treat postpartum endometritis is important. One notable characteristic of endometritis following cesarean section is delayed onset of clinical symptoms. According to our data, 73.3% of postpartum women were hospitalized after discharge from maternity hospitals.
Simultaneously, the issue of increasing antibiotic resistance among both pathogenic and opportunistic microorganisms is becoming increasingly urgent. This situation is complicated by pathogens developing resistance not only to one drug, but also to multiple agents, leading to absolute resistance in some cases. The term ‘superbugs’ has been coined to describe these pathogens, with the primary cause of their emergence attributed to the irrational use of antibacterial drugs in clinical practice [20, 21]. This necessitates a re-evaluation of existing treatment algorithms and encourages the exploration of new methods to address the primary focus of the inflammatory process [22, 23].
Data from our study indicate that E. coli cultured from the uterine cavity of patients with postpartum endometritis exhibited resistance to cephalosporins in 66% of cases, clavulanates in 41%, and aminoglycoside antibiotics in 27.2%. However, the sensitivity to penicillins remained at 82%, fluoroquinolones at 84%, and carbapenems at 98%. A. baumannii demonstrated 100% resistance to cephalosporins, fluoroquinolones, and carbapenems, with 84% resistance to aminoglycosides. Staphylococcus epidermidis was resistant to cephalosporins (30.2%), clindamycin (22.2%), and aminopenicillins and carbapenems (11%). Given the increasing resistance of pathogens to commonly used antibacterial drugs, there is a pressing need to develop alternative strategies and additional means to combat multidrug-resistant microbes. One such approach involves intrauterine application of the molded sorbent VNIITU-1 PVP, whose surface is impregnated with a solution of polyvinylpyrrolidone monomer [24]. This modifier, water-soluble polyvinylpyrrolidone, does not form a strong bond with the sorbent surface, allowing it to desorb in the biological environment and exert an independent antibacterial effect at the site of inflammation [25, 26].
Our study demonstrated the high efficacy of using a modified molded sorbent to treat patients with endometritis after a cesarean section. In group A, where the sorbent was employed, 89% of the cultures showed no growth of the microflora. In contrast, in group B, which received only antibiotic therapy, only 42.6% of cultures were clean; 36.1% of postpartum women exhibited high contamination of the uterine cavity, whereas 21.3% had moderate contamination. Thus, further progression of the inflammatory process may be expected in nearly half of the patients in group B. Despite the confirmed efficacy of combining antibiotic therapy with the use of vulnerosorption, moderate growth of pathogens was recorded in 11% of cases in group A. This finding justified the enhancement of this technique through additional irrigation of the uterine cavity with an antiseptic solution cavitated using low-frequency ultrasound. The antibacterial effect of low-frequency ultrasound is linked to the disruption of microbial cell membranes due to exposure to ultrasonic waves and active oxygen [27, 28]. Furthermore, ultrasound-induced destruction of the extracellular matrix of biofilms increases the sensitivity of microorganisms to antibiotic therapy [16]. Our study found that in patients with post-caesarean endometritis, the combined method effectively removed the pathological substrate from the uterine cavity, enhanced uterine involution processes, and thereby amplified the effect of the molded carbon sorbent.
In summary, combined treatment utilizing antiseptic solutions cavitated by low-frequency ultrasound along with intrauterine administration of the VNIITU-1 PVP sorbent may improve therapeutic outcomes in women with post-caesarean endometritis.
Prospects of the study: during this study, the need arose to identify a new modifier for the sorbent. Given the small number of patients observed across the groups, a multicenter study is warranted.
Conclusion
The following pathogens were identified in patients with postpartum endometritis: Gram-negative bacillus E. coli (43.1% of cases), S. epidermidis (39.6%), E. faecalis (22.4%), and Acinetobacter baumannii (10.34%). The use of antiseptic solutions cavitated by low-frequency ultrasound in treating women with post-caesarean endometritis effectively removes pathogenic contents from the uterine cavity, enhances uterine contractility, and creates favorable conditions for the action of the VNIITU-1 PVP sorbent, thereby improving the sorption of pathogenic microorganisms, toxins, and their decay products.
References
- Серов В.Н., Нестерова Л.А. Особенности современного акушерства. Акушерство и гинекология. 2022; 3: 5-11. [Serov V.N., Nesterova L.A. Features of modern obstetrics. Obstetrics and Gynecology. 2022; (3): 5-11 (in Russian)]. https://dx.doi.org/10.18565/aig.2022.3.5-11.
- Обоскалова Т.А., Глухов Е.Ю., Лаврентьева И.В., Плотко Е.Э., Судаков Е.Ю., Нефф Е.И. Лечение воспалительных заболеваний женских половых органов с использованием лекарственных растворов, кавитированных низкочастотным ультразвуком. Екатеринбург: Vip-Ural; 2012. 48 с. [Oboskalova T.A., Glukhov E.Yu., Lavrent’eva I.V., Plotko E.E., Sudakov E.Yu., Neff E.I. Treatment of inflammatory diseases of female genital organs using medicinal solutions cavitated by low-frequency ultrasound. Yekaterinburg: Vip-Ural; 2012. 48 р. (in Russian)].
- Савельева Г.М., Сухих Г.Т., Серов В.Н., Радзинский В.Е., ред. Акушерство: Национальное руководство. М.: ГЭОТАР-Медиа; 2022. 1080 с. [Savelyeva G.M., Sukhikh G.T., Serov V.N., Radzinsky V.E., ed. Obstetrics: National Guide. Moscow: GEOTAR-Media; 2022. 1080 p. (in Russian)].
- Conroy K., Koenig A.F., Yu Y.H., Courtney A., Lee H.J., Norwitz E.R. Infectious morbidity after cesarean delivery: 10 strategies to reduce risk. Rev. Obstet. Gynecol. 2012; 5(2): 69-77.
- Министерство здравоохранения Российской Федерации. Клинические рекомендации. Послеродовые инфекционные осложнения. М.; 2024. 86 с. [Ministry of Health of the Russian Federation. Postpartum infectious complications. Clinical guidelines. Moscow; 2024. 86 p. (in Russian)].
- Шишкова Ю.С., Киприянова И.И., Узлова Т.В., Липская А.Д. Антимикробный эффект низкочастотного ультразвука в профилактике послеродового эндометрита. Человек. Спорт. Медицина. 2013; 13(2): 102-4. [Shishkova Yu.S., Kipriyanova I.I., Uzlova T.V., Lipskaya A.D. The antimicrobial effect of low-frequency ultrasound in the prevention of postpartum endometritis. Human. Sport. Medicine. 2013; 13(2): 102-4. (in Russian)].
- Щукина Н.А., Благина Е.И., Баринова И.В. Причины формирования и методы профилактики несостоятельного рубца на матке после кесарева сечения. Альманах клинической медицины. 2015; 37: 85-92. [Shchukina N.A., Blagina E.I., Barinova I.V. Causes of inefficient uterine scarring after cesarean section and methods of its prevention. Almanac of Clinical Medicine. 2015; (37): 85-92. (in Russian)].
- Краснопольский В.И., Логутова Л.С., Буянова С.Н., Чечнева М.А., Ахвледиани К.Н. Результаты оперативной активности в современном акушерстве. Журнал акушерства и женских болезней. 2015; 64(2): 53-8. [Krasnopol’skiy V.I., Logutova L.S., Buyanova S.N., Chechneva M.A., Akhvlediani K.N. Results of operative obstetrical activity in modern obstetrics. Journal of Obstetrics and Women's Diseases. 2015; 64(2): 53-8. (in Russian)].
- Boushra M., Rahman O. Postpartum Infection. 2021 Jul 15. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-.
- Ананьевa Е.В., Французов В.Н., Подтетенев А.Д., Ордиянц И.М. Синдром системной воспалительной реакции у родильниц с осложненным течением пуэрперия. Вестник Российской военно-медицинской академии. 2011; 3(35): 49-52. [Ananyeva Е.V., Frantcuzov V.N., Podtetenyev A.D., Ordiyanc I.M. Systemic inflammation response syndrome in obstetric patients with complications in puerperal period. Bulletin of the Russian Military Medical Academy. 2011; 3(35): 49-52. (in Russian)].
- Антушева Т.И. Некоторые особенности влияния ультразвука на микроорганизмы. Живые и биокосные системы. 2013; 4: 11. [Antusheva T.I. Some features of the effect of ultrasound on microorganisms. Live and bio-abiotic systems. 2013; (4): 11. (in Russian)]. https://dx.doi.org/10.18522/2308-9709-2013-4-11.
- Серов В.Н., Баранов И.И., Пекарев О.Г., Пырегов А.В., Тютюнник В.Л., Шмаков Р.Г. Неотложная помощь в акушерстве и гинекологии. М.: ГЭОТАР-Медиа; 2017. 240 с. [Serov V.N., Sukhikh G.T., Baranov I.I., Pyregov A.V., Tyutyunnik V.L., Shmakov R.G. Emergency care in obstetrics and gynecology. Moscow: GEOTAR-Media; 2017: 240 p. (in Russian)].
- Голубкова А.А., Смирнова С.С., Большакова А.Н. Клинико-эпидемиологические характеристики факторов риска эндометрита у родильниц и современные технологии родоразрешения. Профилактическая и клиническая медицина. 2017; 2(63): 48-53. [Golubkova A.A., Smirnova S.S., Bolshakova A.N. Clinical and epidemiological characteristics of risk factors of endometritis in postpartum women and modern technology delivery. Preventive and Clinical Medicine. 2017; 2(63): 48-53. (in Russian)].
- Горин В.С., Матвеева И.В., Дремова И.В., Попова Ж.Ю., Чернякина О.Ф. Роль иммунной системы в патогенезе гнойно-воспалительных заболеваний пуэрперия. Сибирский медицинский журнал. 2012; 108(1): 5-10. [Gorin V.S., Matveeva I.V., Dremova I.V., Popova Zh.Yu., Chernyakina O.F. The role of immune system in pathogenesis of puerperium pyoinflammatory diseases. Siberian Medical Journal. 2012; 108(1): 5-10. (in Russian)].
- Обоскалова Т.А., Кононова И.Н., Ворошилина Е.С. Иммунокоррекция кавитированными ультразвуком растворами в комплексном лечении цервикальных интраэпителиальных неоплазий, ассоциированных с папилломавирусной инфекцией. Уральский медицинский журнал. 2013; 109(4): 46-51. [Oboskalova T.A., Kononova I.N., Voroshilina E.S. Immunocorrection solutions, processed by ultrasound in complex treatment of cervical neoplasia associated with human papillomavirus infection. Ural Medical Journal. 2013; 109(4): 46-51. (in Russian)].
- Глухов Е.Ю., Дикке Г.Б. Применение и клинические эффекты низкочастотной ультразвуковой кавитации в акушерстве и гинекологии. Акушерство и гинекология. 2016; 1: 109-16. [Glukhov E.Yu., Dikke G.B. The use and clinical effects of low-frequency ultrasound cavitation in obstetrics and gynecology. Obstetrics and Gynecology. 2016; (1): 109-16. (in Russian)]. https://dx.doi.org/10.18565/aig.2016.1.109-116.
- Глухов Е.Ю., Серова О.Ф., Обоскалова Т.А., Лаврентьева И.В., Чернигова И.В., Игнатова Ю.В. Профилактика и лечение послеродовых эндометритов с помощью кавитированных растворов. Доктор.Ру. Гинекология Эндокринология. 2014; 1(89): 13-7. [Glukhov E.Yu., Serova O.F., Oboskalova T.A., Lavrentieva I.V., Tchernigova I.V., Ignatova Yu.V. Ultrasonic cavitation in liquids: Use of ultrasonically-treated solutions to prevent and treat postpartum endometriosis. Doctor.Ru. Gynecology Endocrinology. 2014; 1(89): 13-7. (in Russian)].
- Баринов С.В., Лазарева О.В., Тирская Ю.И., Кадцына Т.В., Чуловский Ю.И., Орлицкая А.Д., Леонтьева Н.Н., Блауман Е.С. Опыт применения модифицированного формованного сорбента при лечении послеродового эндометрита. Акушерство и гинекология. 2023; 6: 89-98. [Barinov S.V., Lazareva O.V., Tirskaya Yu.I., Kadtsyna T.V., Chulovsky Yu.I., Orlitskaya A.D., Leont'eva N.N., Blauman E.S. Experience with a modified molded sorbent in the treatment of postpartum endometritis. Obstetrics and Gynecology. 2023; (6): 89-98 (in Russian)]. https://dx.doi.org/10.18565/aig.2023.37.
- Апресян С.В., Димитрова В.И., Слюсарева О.А. Диагностика и лечение послеродовых гнойно-септических заболеваний. Доктор.Ру. 2018; 6(150): 17-24. [Apresyan S.V., Dimitrova V.I., Slyusareva O.A. Diagnosis and treatment of postpartum purulent septic diseases. Doctor.Ru. 2018; 6(150): 17-24. (in Russian)]. https://dx.doi.org/10.31550/1727-2378-2018-150-6-17-24.
- Гельфанд Б.Р., Руднов В.А., Галстян Г.М., Гельфанд Е.Б., Заболотских И.Б., Золотухин К.Н., Кулабухов В.В., Лебединский К.М., Левит А.Л., Нехаев И.В., Николенко А.В., Проценко Д.Н., Щеголев А.В., Ярошецкий А.И. Сепсис: терминология, патогенез, клинико-диагностическая концепция. Вопросы гинекологии, акушерства и перинатологии. 2017; 16(1): 64-72. [Gelfand B.R., Rudnov V.A., Galstyan G.M., Gelfand E.B., Zabolotskikh I.B., Zolotukhin K.N., Kulabukhov V.V., Lebedinskiy K.M., Levit A.L., Nekhaev I.V., Nikolenko A.V., Protsenko D.N., Shchegolev A.V., Yaroshetskiy A.I. Sepsis: terminology, pathogenesis, clinical diagnostic conception. Gynecology, Obstetrics and Perinatology. 2017; 16(1): 64–72. (in Russian)]. https://dx.doi.org/10.20953/1726-1678-2017-1-64-72.
- Igwemadu G.T., Eleje G.U., Eno E.E., Akunaeziri U.A., Afolabi F.A., Alao A.I. et al. Single-dose versus multiple-dose antibiotics prophylaxis for preventing caesarean section postpartum infections: A randomized controlled trial. Womens Health (Lond.). 2022; 18: 17455057221101071. https://dx.doi.org/10.1177/17455057221101071.
- Жилинкова Н.Г. Современные представления о пуэрперальных инфекциях в связи с антибактериальной резистентностью и завершением эры антибиотиков. Акушерство и гинекология: новости, мнения, обучение. 2019; 7(3): 70-5. [Zhilinkova N.G. Modern ideas about puerperal infections due to antibacterial resistance and the end of the antibiotic era. Obstetrics and Gynecology: News, Opinions, Training. 2019; 7(3): 70-5. (in Russian)]. https://dx.doi.org/10.24411/2303-9698-2019-13010.
- Moulton L.J., Lachiewicz M., Liu X., Goje O. Endomyometritis after cesarean delivery in the era of antibiotic prophylaxis: incidence and risk factors. J. Matern. Fetal. Neonatal. Med. 2018; 31(9): 1214-9. https://dx.doi.org/10.1080/14767058.2017.1312330.
- Barinov S.V., Tirskaya Y.I., Borisova A.B., Pyanova L.G., Di Renzo G.C. The effectiveness of using a molded sorbent: Modified polyvinylpyrrolidone for the combined treatment of chronic endometritis. Int. J. Gynaecol. Obstet, 2021; 154 (2): 277-84. https://dx.doi.org/10.1002/ijgo.13609.
- Долгих В.Т., Долгих Т.И., Пьянова Л.Г., Лихолобов В.А., Баринов С.В., Баракина О.В., Гриценко Н.С., Толкач А.Б. Антимикробная активность гранулированных углеродных сорбентов. Российский иммунологический журнал. 2014; 8(3): 788-91. [Dolgikh V.T., Dolgikh T.I., P'yanova L.G., Likholobov V.A., Barinov S.V., Barakina O.V., Gritsenko N.S., Tolkach A.B. Antimicrobial activity of granular carbon sorbents. Russian Journal of Immunology. 2014; 8(3): 788-91. (in Russian)].
- Бакланова О.Н., Пьянова Л.Г., Талзи В.П., Княжева О.А., Седанова А.В., Долгих Т.И., Лихолобов В.А. Модифицирование поверхности углеродного сорбента поли-N-винилпирролидоном для аппликационной медицины. Физикохимия поверхности и защита материалов. 2012; 48(4): 363-9. [Baklanova O.N., P'yanova L.G., Talzi V.P., Knyazheva O.A., Sedanova A.V., Dolgikh T.I., Likholobov V.A. Modification of carbon sorbent surface by poly-N-vinylpyrrolidone in application medicine. Protection of Metals and Physical Chemistry of Surfaces. 2012; 48(4): 427-33. (in Russian)]. https://dx.doi.org/10.1134/S2070205112040041.
- Серов В.Н., Тютюнник В.Л., Кан Н.Е., Баранов И.И. Послеродовые гнойно-септические заболевания. Руководство для врачей. М.: ГЭОТАР-Медиа; 2022. 208 с. [Serov V.N., Tyutyunnik V.L., Kan N.E., Baranov I.I. Postpartum purulent-septic diseases. Guide for doctors. Moscow: GEOTAR-Media; 2022. 208 p. (in Russian)].
- Тютюнник В.Л., Кан Н.Е., Вересова А.А., Амирасланов Э.Ю. Иммуномодулирующие препараты в комплексной терапии послеродового эндометрита. Медицинский совет. 2016; (2): 55-9. [Tyutyunnik V.L., Kan N.E., Veresova A.A., Amiraslanov E.Y. Immunomodulatory drugs in the treatment of postpartum endometritis. Medical Council. 2016; (2): 55-9. (in Russian)]. https://dx.doi.org/10.21518/2079-701X-2016-2-55-59.
Received 06.12.2024
Accepted 29.01.2025
About the Authors
Sergey V. Barinov, Dr. Med. Sci., Professor, Head of the Department of Obstetrics and Gynecology No. 2, Omsk State Medical University, Ministry of Health of Russia, 644099, Russia, Omsk, Lenin str., 12, +7(913)633-80-48, barinov_omsk@mail.ru, https://orcid.org/0000-0002-0357-7097Yuliya I. Tirskaya, Dr. Med. Sci., Аssociate Рrofessor, Professor at the Department of Obstetrics and Gynecology No. 2, Omsk State Medical University, Ministry of Health
of Russia, 644099, Russia, Omsk, Lenin str., 12, +7(3812)24-06-58, yulia.tirskaya@yandex.ru, https://orcid.org/0000-0001-5365-7119
Natalia E. Kan, Dr. Med. Sci., Professor, Deputy Director of Science – Director of the Institute of Obstetrics, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia, 117997, Russia, Moscow, Ac. Oparin str., 4, kan-med@mail.ru, https://orcid.org/0000-0001-5087-5946
Victor L. Tyutyunnik, Dr. Med. Sci., Professor, Leading Researcher, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia, 117997, Russia, Moscow, Ac. Oparin str., 4, tioutiounnik@mail.ru, https://orcid.org/0000-0002-5830-5099
Oksana V. Lazareva, PhD, Аssociate Рrofessor, Department of Obstetrics and Gynecology No. 2, Omsk State Medical University, Ministry of Health of Russia,
644099, Russia, Omsk, Lenin str., 12, +7(3812)24-06-58, lazow@mail.ru, https://orcid.org/0000-0002-0895-4066
Tatiana V. Kadtsyna, PhD, Аssociate Рrofessor, Department of Obstetrics and Gynecology No. 2, Omsk State Medical University, Ministry of Health of Russia,
644099, Russia, Omsk, Lenin str., 12, +7(3812)24-06-58, tatianavlad@list.ru, https://orcid.org/0000-0002-0348-5985
Ekaterina S. Blauman, PhD student, Department of Obstetrics and Gynecology No. 2, Omsk State Medical University, Ministry of Health of Russia,
644099, Russia, Omsk, Lenin str., 12, +7(908)809-68-78, blauman-es@yandex.ru, https://orcid.org/0000-0002-1498-0578
Egor A. Khoroshkin, Teaching Assistant at the Department of Obstetrics and Gynecology № 2, Omsk State Medical University, +7(3812)24-06-58,
drrussian@mail.ru, https://orcid.org/0000-0002-0433-8960
Lyudmila L. Shkabarnya, Head of the Department of Gynecology of the Perinatal Center, Regional Clinical Hospital, 644012, Russia, Omsk, Berezovaya str., 3/1,
+7(913)966-10-48, l_shka@mail.ru
Lydia G. Pyanova, Dr. Bio. Sci., Associate Professor, Leading Researcher, Laboratory of Synthesis of Functional Carbon Materials, Center for New Chemical Technologies, Institute of Catalysis, Siberian Branch of the Russian Academy of Sciences, 644040, Russia, Omsk, Neftezavodskaya str., 54, +7(3812)67-04-50, medugli@ihcp.ru,
https://orcid.org/0000-0002-6207-0878
Corresponding author: Sergey V. Barinov, barinov_omsk@mail.ru