The effectiveness of programs of embryo cryo-transfer into the uterine cavity in women with overweight and obesity
Kraevaya Е.Е., Makarova N.P., Kalinina E.A., Nazarenko T.A.
Relevance: Overweight and obesity is a medical and social issue, which has a tendency to progress. It is known about the negative impact of obesity on the cardiovascular system, musculoskeletal system, and increased risk of developing diabetes. The incidence of gynecological diseases and the risk of developing obstetric complications is higher in patients with obesity. The patients with obesity have high prevalence of gynecological diseases and the risk of developing obstetric complications. There is data on reduced effectiveness of assisted reproductive technology (ART) programs in women of this category.
Objective: The purpose of the study was to make a comparative analysis of the effectiveness of the programs of thawed embryo transfer into the uterine cavity in women with overweight and obesity.
Materials and methods: The study included 186 patients. Among them, 76 women had overweight and obesity, and 110 women had normal weight. All patients underwent infertility treatment using the program of thawed embryo transfer into the uterine cavity. The comparison was made between clinical pregnancy rate (CPR) and the rate of early reproductive losses before 12 weeks’ gestation depending on the body mass index (BMI).
Results: In both groups the patients were comparable in menstrual function, the frequency of comorbidities and gynecological diseases, infertility duration and the number of previous ART attempts in history. The age of patients in the group with BMI≥25 kg/м2 was higher, but the difference in age had no statistically significant influence on pregnancy rate (PR) and miscarriage rate, as well as preimplantation genetic testing for aneuploidy (PGT-A), that was used to test some embryos, which were transferred to patients in both groups. It was found that in patients with BMI≥25 kg/м2 the chances of getting pregnant reduced by 2 times, and the chances of early reproductive losses before 12 weeks’ gestation increased by 3.6 times.
Conclusion: Overweight and obesity reduce the effectiveness of the programs of thawed embryo transfer into the uterine cavity, most likely due to reduction of embryo implantation potential, including euploid embryos.
Authors' contributions: Kraevaya Е.Е. – the concept and design of the study, material collection and processing, manuscript writing; Makarova N.P., Kalinina E.A. – text editing; Nazarenko T.A. – the concept and design of the study, editing.
Conflicts of interest: The authors confirm that they have no conflict of interest to declare.
Funding: The study was conducted without any sponsorship.
Ethical Approval: The study was approved by the local Bioethics Commission of the Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia, protocol No. 1 of February 22, 2023.
Patient Consent for Publication: The patients have signed informed consent for publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available on request from the corresponding author after approval from the principal investigator.
For citation: Kraevaya Е.Е., Makarova N.P., Kalinina E.A., Nazarenko T.A.
The effectiveness of programs of embryo cryo-transfer into the uterine cavity in women with overweight and obesity.
Akusherstvo i Gynecologia/Obstetrics and Gynecologу. 2024; (8): 114-120 (in Russian)
https://dx.doi.org/10.18565/aig.2024.92
Keywords
The issue of overweight is becoming more relevant. Currently, about 60% of population in the developed countries is overweight, and 25–30% is obese, and this indicator is growing from year to year [1, 2]. Obesity is associated with increased risk of cardiovascular diseases, endocrine disorders and musculoskeletal diseases [2]. In women of reproductive age, overweight is associated with menstrual irregularities, polycystic ovary syndrome (PCOS), lower chance of conception, and hyperplastic diseases of the reproductive system [3].
Obesity may have negative influence on all steps of assisted reproductive technology (ART) programs, the course of pregnancy and delivery outcomes. According to available data, ovarian stimulation phase in patients with overweight requires higher doses of gonadotropins. The number of oocytes and zygotes is lower compared to patients with normal body weight. Embryos are characterized by slower cleavage speed. Blastocyst formation rate on day 6 of culture is higher. Embryo implantation rate may be decreased, and the likelihood of obstetric complications increases [4–7]. In contrast to these data, a large number of studies demonstrate that there is no any relationship between overweight and adverse outcomes of ART programs. Moreover, one large study presents data on possible protective effect of excess lipids in embryonic cells during cryopreservation, and as a result, a greater implantation potential when embryos are thawed. Although in their study, the authors reported higher rate of miscarriages in patients with overweight and obesity [8].
The purpose of our study was to compare pregnancy rate (PR) and the rate of early reproductive losses before 12 weeks’ gestation in patients with normal body weight, and in women with overweight and obesity, who underwent thawed embryo transfer into the uterine cavity.
Cryo-embryo transfer (CET) protocol enables to rule out adverse factors of IVF programs and embryo transfer (ET) in stimulated cycle, such as blastocyst and endometrial development asynchrony and displacement of the “implantation window” [9], as well as hypercoagulable changes in the blood accompanying ovarian stimulation, which are more pronounced in patients with obesity [10, 11].
Material and methods
The study included 186 female patients with infertility, who underwent thawed embryo transfer into the uterine cavity in 2022–2023 at Prof. B.V. Leonov Department of Assisted Technologies in Infertility Treatment of the Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia (the Center). The study was approved by the local Bioethics Commission of the Center, protocol No. 1 of February 22, 2023.
Based on the body mass index (BMI) value, the patients were divided into 2 groups: 110 patients with normal body weight (BMI <25 kg/м2), and 76 patients with overweight (BMI ≥25 kg/м2) and obesity (BMI ≥ 30 kg/м2). Inclusion criteria were the patients aged 18–38 years, BMI ≥18 kg/м2; tubal-peritoneal factor of infertility; normal karyotype; the use of patient’s own oocytes. Exclusion criteria were contraindications to undergo infertility treatment using ART techniques; external genital endometriosis and adenomyosis stage 3–4; the use of donor gametes or surrogacy; and secondary and symptomatic obesity in patients with BMI ≥25 kg/м2. Before enrollment in the study all participants underwent medical examination according to the clinical recommendations of the MH of the RF (2021) “Female infertility” [12]. In addition, BMI was calculated. The patients in both groups received infertility treatment using thawed embryo transfer into the uterine cavity.
All patients underwent equally endometrial preparation with estrogen-gestagen therapy. Starting from the 3rd day of the menstrual cycle, the women were administered estradiol hemihydrate. When endometrial thickness reached at least 8 mm, but not earlier than on the 13th day of the menstrual cycle, micronized progesterone was added to hormone therapy. All transferred embryos were of similar morphological quality 3–6 A–B according to Gardner grading system [13]. Cryopreservation and subsequent thawing of all obtained embryos was performed using Kitazato media (Japan). A part of embryos, obtained during previous performance of IVF/ICSI program, underwent preimplantation genetic testing for aneuploidy (PGT-A), for which the indications were the age of patients over 35 years and implantation losses in ART programs in history. Pregnancy was diagnosed based on the increase in serum concentration of the β-subunit of human chorionic gonadotropin (β-hCG) and visualization of the fertilized egg in the uterine cavity during ultrasound examination 21 days after the day of ET into the uterine cavity. Miscarriage was diagnosed when there was dynamic decrease in hCG level, according to ultrasound diagnosis and clinical signs of miscarriage.
Statistical analysis
Software program SPSS, version 27 was used for statistical data processing. Mann-Whitney U test was used to assess quantitative data considering non-normal distribution. The data are represented as Me (Q1; Q3), where Me is median, and (Q1; Q3) is interquartile range. Pearson’s chi-squared (χ2) test was used to assess frequency indicators. The data are represented as absolute values and the percentage. The differences between the values we considered to be statistically significant at р<0.05.
Results
Depending of BMI, the patients were divided into groups. The main group (n=76) included the patients with BMI ≥25 kg/m2. Among them, 12 patients were with BMI from 30 to 34.9 kg/m2, and 4 patients were with BMI ≥35 kg/m2. The comparison group (n=110) included the patients with BMI <25 kg/m2. BMI≥25 kg/m2 was considered as threshold with regard to clinical recommendations “Obesity” of the MH of the RF (2020) [14], and the greater likelihood of developing various pathological conditions in exceeding this value.
The first step was assessment of clinical and laboratory data of the patients in both groups (Table 1). The mean age of women in the group with BMI≥25 kg/m2 was significantly higher – 33.5 years (31; 36) versus 31 years (29; 34) in the comparison group (р<0.001). However, the difference had no statistically significant influence on PR (р=0.07) and miscarriage rate (р=0.61). There were no statistically significant differences in characteristics of menstrual cycle, the frequency of comorbidities and gynecological diseases between the study groups. This fact enabled to carry out the second step of the study and to compare the clinical effectiveness of thawed embryo transfer protocols.
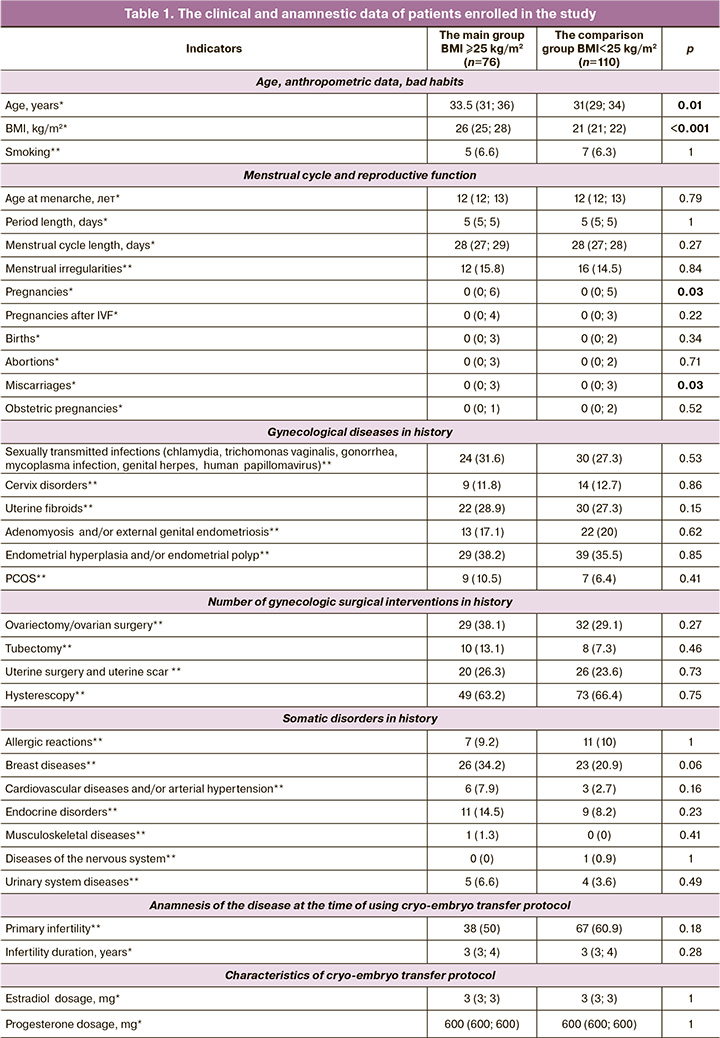
During endometrial preparation therapy with estrogens and gestagens in both groups, the frequency of clinically insignificant side effects and clinical effectiveness of treatment, which was assessed by M-mode ultrasound measurement of the endometrial thickness on the day of ET into the uterine cavity, were comparable. In the main group (BMI≥25 kg/м2), ET procedure was performed in patients a little later, due to longer menstrual cycle and longer time to achieve the optimal endometrial thickness and structure. Some women underwent euploid embryo transfer (according to the results of PGT-A) – 66 patients in the comparison group, 50 in the main group. The difference between them was not statistically significant (р=0.44) and had no influence on PR (р=0.61) and miscarriage rate (р=0.16). In the comparison group, 76 patients became pregnant (69,1%), and 40 patients (52,6%) in the main group. The differences between the groups were statistically significant (р=0.023). The association found in our study was weak (V=0.167). The obtained data are presented in Table 2. Comparison of early miscarriage rates showed that in the comparison group, 8/76 (10,5%) pregnant women (10,5%) with normal body weight and 12/40 (30%) in the main group had miscarriage. The difference was also statistically significant (р=0.008). Moderate association was found (V=0.245).
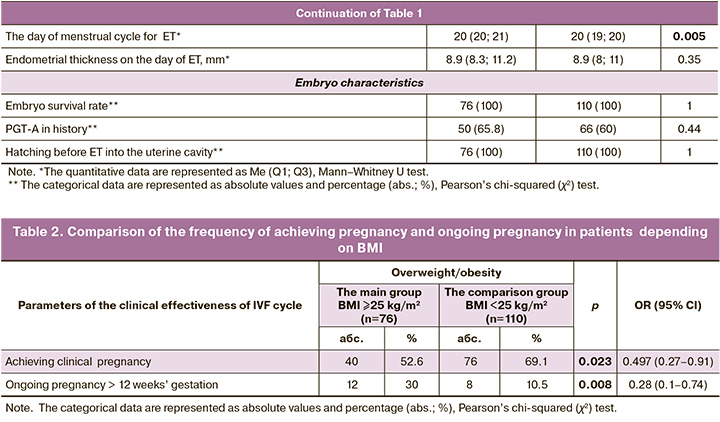
In patients with BMI ≥25 kg/m2 the chances of getting pregnant reduced by 2 times compared to patient with normal body weight. Odds ratio of pregnancy onset was 0.49 (95% CI 0.27–0.91), р=0.023. In addition, in women with overweight and obesity miscarriage probability before 12 week's gestation increased by 3.6 times. Odds ratio of ongoing pregnancy was 0.28 (95% CI 0.1–0.74), р=0.008.
Discussion
Overweight and obesity can have an adverse effect on all steps of ART program. In women of this category, embryos are characterized by slower cleavage speed and reduced implantation potential [15, 16].
Additional factors reducing embryo implantation potential in stimulated cycles can be asynchrony of endometrial and blastocyst development, which is more likely to be in patients with overweight and obesity, as well as hypercoagulable changes in the blood, and probably higher levels of anti-inflammatory markers in the uterine microenvironment. These factors can be eliminated by carrying out cryo-embryo protocol [17].
It is known that overweight and obesity has no influence on embryo ploidy, but according to some studies, even morphologically appropriate euploid embryo transfer is less likely to result in pregnancy [16]. It can be suggested, that implantation losses are most likely due to changes in embryonic functional activity, either by decline of endometrial receptivity or the influence of maternal proinflammatory markers on the implanted embryo.
Endometrial receptivity in patients with obesity is also a subject of debate, but the studies on embryo transfer, where embryos obtained from oocytes of donors with normal weight were transferred to obese and non-obese women, indicate comparable PR and, accordingly, the absence of uterine factor of implantation losses in patients of this category [18].
Our study compared pregnancy rate and miscarriage rate before 12 weeks’ gestation in patients with normal body weight and overweight/obesity, who underwent thawed embryo transfer into the uterine cavity. It was found that in patients with BMI ≥25 kg/m2, the chances of getting pregnant reduced by 2 times compared to patients with BMI 18–25 kg/m2 (OR=0.49 (95% CI 0.27–0.91), and the frequency of miscarriages increased by 3.6 times (OR of ongoing pregnancy=0.28 (95% CI 0.1–0.74), р=0.008). This trend was maintained, when euploid embryos were transferred.
Given 100% embryo survival after thawing in both groups, comparable morphological quality of thawed embryos, absence of implantation advantages in euploid blastocysts, similar endometrial thickness and structure on the day of thawed embryo transfer into the uterine cavity, it can be assumed that the decline in the embryo implantation potential in patients with overweight and obesity is due impaired functional activity of embryos, possibly due to altered metabolic characteristics and epigenetic changes [19, 20], that requires further research in this area. Komarova E.M. et al. (2023) showed that metabolomics impairments, such as decreased mitochondrial function in cumulus cells lead to significant reduction of infertility treatment effectiveness using ART techniques, especially in women with obesity [21].
Considering the results obtained in our study on significantly reduced PR in carrying out cryo-transfer protocols, as well as increased risk of miscarriage at early pregnancy, including euploid embryo transfer in patients with overweight and obesity, it is advisable to recommend the patients of this category to reach healthy weight before undergoing ART program and obtaining embryos, given the significant impact of overweight on embryo implantation potential.
Conclusion
The study showed that worse prognoses of infertility treatment using thawed embryo transfer into the uterine cavity, including euploid embryos according to the results of PGT-A, are in patients with overweight and obesity, that requires further research and development of therapeutic strategies to optimize infertility treatment using ART techniques in patients of this category.
References
- Всемирная организация здравоохранения. Ожирение и избыточная масса тела. 1 марта 2024. Доступно по: https://www.who.int/ru/news-room/fact-sheets/detail/obesity-and-overweight [WHO. Obesity and overweight. March 1, 2024. Available at: https://www.who.int/ru/news-room/fact-sheets/detail/obesity-and-overweight (in Russian)].
- World Obesity. Global Obesity Observatory. Data tables. Prevalence of adult overweight and obesity (%). Available at: https://data.worldobesity.org/tables/prevalence-of-adult-overweight-obesity-2/
- Андреева Е.Н., Шереметьева Е.В., Фурсенко В.А. Ожирение - угроза репродуктивного потенциала России. Ожирение и метаболизм. 2019; 16(3): 20-8. [Andreeva E.N., Sheremet'eva E.V., Fursenko V.A. Obesity - threat to the reproductive potential of Russia. Obesity and Metabolism. 2019; 16(3): 20-8. (in Russian)]. https://dx.doi.org/10.14341/omet10340.
- Горелова И.В., Рулев М.В., Попова П.В. Влияние ожирения на результаты программ вспомогательных репродуктивных технологий (обзор литературы). Проблемы репродукции. 2018; 24(6): 39-45. [Gorelova I.V., Rulev M.V., Popova P.V. The effect of obesity on the results of assisted reproductive technologies (a review). Russian Journal of Human Reproduction. 2018; 24(6): 39-45. (in Russian)]. https://dx.doi.org/10.17116/repro20182406139.
- Махмадалиева М.Р., Коган И.Ю., Ниаури Д.А., Мекина И.Д., Гзгзян А.М. Влияние избытка массы тела и ожирения на эффективность программ вспомогательных репродуктивных технологий. Журнал акушерства и женских болезней. 2018; 67(2): 32-9. [Makhmadalieva M.R., Kogan I.Yu., Niauri D.A., Mekina I.D., Gzgzyan A.M. The effect of excess body weight and obesity on the effectiveness of assisted reproductive technologies programs. Journal of Obstetrics and Women's Diseases. 2018; 67(2): 32-9. (in Russian)]. https://dx.doi.org/10.17816/JOWD67232-39.
- Долгушина Н.В., Десяткова Н.В., Донников А.Е., Высоких М.Ю., Суханова Ю.А., Долгушин О.А., Пархоменко А.А. Роль адипокинов и генов-регуляторов адипокинов в эффективности программ вспомогательных репродуктивных технологий у пациенток с избыточной массой тела. Акушерство и гинекология. 2017; 2: 71-8. [Dolgushina N.V., Desyatkova N.V., Donnikov A.E., Vysokikh M.Yu., Sukhanova Yu.A., Dolgushin O.A., Parkhomenko A.A. The role of adipokines and their regulatory genes in the effectiveness of ART programs in overweight patients. Obstetrics and Gynecology. 2017; (2): 71-8. (in Russian)]. https://dx.doi.org/10.18565/aig.2017.2.71-8.
- Tang J., Xu Y., Wang Z., Ji X., Qui Q., Mai Z. et al. Association between metabolic healthy obesity and female infertility: the national health and nutrition examination survey. 2013-2020. BMC Public Health. 2023; 23(1):1524. https://dx.doi.org/10.1186/s12889-023-16397-x.
- Zeng Z., Li J., Wang X., Yi S., Bi Y., Mo D. et al. Influence of maternal obesity on embryonic vitrification injury and subsequent pregnancy outcomes: a retrospective cohort study. Heliyon. 2023; 9(9): e20095. https://dx.doi.org/10.1016/j.heliyon.2023.e20095.
- Краснопольская К.В., Бекетова А.Н., Сесина Н.И., Чинченко Н.К., Конеева Ц.О., Бочарова Т.В. Сравнение результативности переносов эмбрионов на 5-е и 6-е сутки развития в свежих циклах или криопротоколах экстракорпорального оплодотворения. Проблемы репродукции. 2019; 25(5): 86-91. [Krasnopol'skaya K.V., Beketova A.N., Sesina N.I., Chinchenko N.K., Koneeva Ts.O., Bocharova T.V. A comparison of the effectiveness of fresh or frozen embryo transfer on day 5 or day 6. Russian Journal of Human Reproduction. 2019; 25(5): 86-91. (in Russian)]. https://dx.doi.org/10.17116/repro20192505186.
- Вдовиченко Ю.П., Фирсова Н.А., Алипова Н.Ф. Гемостазиологические аспекты неудачных попыток экстракорпорального оплодотворения у женщин с метаболическим синдромом. Репродуктивное здоровье. Восточная Европа. 2019; 9(6): 755-63. [Vdovichenko Yu.P., Firsova N.A., Alipova N.F. Hemostasiological aspects of unsuccessful attempts at in vitro fertilization in women with metabolic syndrome. Reproductive Health. Eastern Europe. 2019; 9(6): 755-63. (in Russian)].
- Хромылев А.В., Макацария А.Д. Ожирение, метаболический синдром и тромбофилия. Акушерство и гинекология. 2017; 10: 27-33. [Khromylev A.V., Makatsariya A.D. Obesity, metabolic syndrome, and thrombophilia. Obstetrics and Gynecology. 2017; (10): 27-33. (in Russian)]. https://dx.doi.org/10.18565/aig.2017.10.27-33.
- Министерство здравоохранения Российской Федерации. Клинические рекомендации. Женское бесплодие. 2021. [Ministry of Health of the Russian Federation. Clinical guidelines. Female infertility. 2021. (in Russian)].
- Gardner D., Weissman A., Howles C.M., Shoham Z.E. Textbook of assisted reproductive technologies. 3rd ed. London: CRC Press; 2009. 952p.
- Министерство здравоохранения Российской Федерации. Клинические рекомендации. Ожирение. 2020. [Ministry of Health of the Russian Federation. Clinical guidelines. Obesity. 2020. (in Russian)].
- Bellver J., Brandão P., Alegre L., Meseguer M. Blastocyst formation is similar in obese and normal weight women: a morphokinetic study. Hum. Reprod. 2021; 36(12): 3062-73. https://dx.doi.org/10.1093/humrep/deab212.
- Cozzolino M., García-Velasco J.A., Meseguer M., Pellicer А., Bellver J. Female obesity increases the risk of miscarriage of euploid embryos. Fertil. Steril. 2021; 115(6): 1495-502. https://dx.doi.org/10.1016/j.fertnstert.2020.09.139.
- Bellver J., Marin C., Lathi R.B., Murrugapan G., Labarta E., Vidal C. et al. Obesity affects endometrial receptivity by displacing the window of implantation. Reprod. Sci. 2021; 28(11): 3171-80. https://dx.doi.org/10.1007/s43032-021-00631-1.
- Moreta L.E., Hanley W., Lee J.A., Copperman A.B., Stein D. Elevated body mass index in donor oocyte recipients does not affect implantation of euploid embryos. J. Womens Health (Larchmt). 2022; 31(9): 1364-8. https://dx.doi.org/10.1089/jwh.2021.0433.
- Rohde K., Keller M. , la Cour Poulsen L., Blüher M. , Kovacs P., Böttcher Y. Genetics and epigenetics in obesity. Metabolism. 2019; 92: 37-50. https://dx.doi.org/10.1016/j.metabol.2018.10.007.
- Драпкина О.М., Ким О.Т. Эпигенетика ожирения. Кардиоваскулярная терапия и профилактика. 2020; 19(6): 2632. [Drapkina O.M., Kim O.T. Epigenetics of obesity. Cardiovascular Therapy and Prevention. 2020; 19(6): 2632. (in Russian)]. https://dx.doi.org/10.15829/1728-8800-2020-2632.
- Комарова Е.М., Лесик Е.А., Объедкова К.В., Рыжов Ю.Р., Гзгзян А.М., Тапильская Н.И. Прогностическое значение маркеров митохондриальной дисфункции клеток кумулюса в получении эмбрионов оптимального качества в протоколах вспомогательных репродуктивных технологий. Проблемы репродукции. 2023; 29(6): 57-64. [Komarova E.M., Lesik E.A., Ob’edkova K.V., Ryzhov Yu.R., Gzgzyan A.M., Tapil’skaya N.I. Prognostic significance of cumulus cells mitochondrial dysfunction markers in obtaining optimal quality embryos in assisted reproductive technologies protocols. Russian Journal of Human Reproduction. 2023; 29(6): 57-64. (in Russian)]. https://dx.doi.org/10.17116/repro20232906157.
Received 16.04.2024
Accepted 12.07.2024
About the Authors
Elizaveta E. Kraevaya, PhD, Researcher at the Department of Assisted Technologies for the Treatment of Infertility, Academician V.I. Kulakov National Medical Research Center of Obstetrics, Gynecology, and Perinatology, Ministry of Health of Russia, 117997, Russia, Moscow, Ac. Oparin str., 4, +7(495)531-44-44, e_kraevaya@oparina4.ru, https://orcid.org/0000-0002-8140-0035Natalya P. Makarova, Dr. Bio. Sci., Leading Researcher at the Department of Assisted Technologies for the Treatment of Infertility, Academician V.I. Kulakov National Medical Research Center of Obstetrics, Gynecology, and Perinatology, Ministry of Health of Russia, 117997, Russia, Moscow, Ac. Oparin str., 4, +7(495)531-44-44,
np_makarova@oparina4.ru, https://orcid.org/0000-0003-1396-7272
Elena A. Kalinina, Dr. Med. Sci., Professor, Head of the Department of Assisted Technologies for the Treatment of Infertility, Academician V.I. Kulakov National Medical Research Center of Obstetrics, Gynecology, and Perinatology, Ministry of Health of Russia, 117997, Russia, Moscow, Ac. Oparin str., 4, +7(495)531-44-44,
e_kalinina@oparina4.ru, https://orcid.org/0000-0002-8922-2878
Tatyana A. Nazarenko, Dr. Med. Sci., Professor, Director of the Institute of Reproductive Medicine, Head of the F. Paulsen Scientific and Clinical Department of IVF, Academician V.I. Kulakov National Medical Research Center of Obstetrics, Gynecology, and Perinatology, Ministry of Health of Russia, 117997, Russia, Moscow,
Ac. Oparin str., 4, +7(495)531-44-44, t_nazarenko@ oparina4.ru, https://orcid.org/0000-0002-5823-1667