В настоящее время отмечается выраженная тенденция к увеличению частоты врастания плаценты. С 1990-х гг. частота встречаемости заболевания увеличилась более чем в 10 раз. При этом рост частоты кесарева сечения значительно ниже. [1]. Вероятно, увеличение частоты встречаемости врастания плаценты связано с особенностями техники кесарева сечения (отсепаровка и низведение мочевого пузыря, разрез в нижнем маточном сегменте ближе к шейке матки).
По данным Калифорнийского университета (США) ежегодное увеличение числа кесарева сечения, как первого, так и повторного, будет способствовать пропорциональному росту беременных с патологической плацентацией – 6236 новых случаев предлежания плаценты, 4504 случаев врастания плаценты. Такой рост приведет к повышению уровня материнской смертности на 130 случаев ежегодно [2, 3].
Врастание плаценты значительно чаще встречается у женщин, перенесших кесарево сечение, по сравнению с женщинами, имеющими самопроизвольные роды в анамнезе [4–6]. Увеличение числа оперативного родоразрешения повышает риск врастания плаценты, но не коррелирует с глубиной инвазии [5, 7–9].
Также, встречается врастание плаценты и при отсутствии рубца на матке после кесарева сечения. Такое врастание является наиболее тяжелым типом врастания плаценты, так как очень сложно диагностируется и в основном является интраоперационной находкой. Оно связано с высоким риском массивной кровопотери, гистерэктомией и материнской смертностью. Причиной такого врастания является травматизация эндометрия (кюретаж матки, ручное обследование послеродовой матки и др.), приводящая к нарушению его васкуляризации и хроническому воспалению [5, 10–13]. При этом гиперинвазия ворсин хориона происходит не локально – в область рубца, а по всей поверхности миометрия, что значительно повышает риск кровопотери и гистерэктомии.
Одной из проблем, связанных с родоразрешением пациенток с врастанием плаценты, является отсутствие четкой классификации врастания. В настоящее время клиницисты используют гистологическую градацию степени врастания плаценты. На основании глубины инвазии выделяют placenta accreta (приращение плаценты к мышечному слою), placenta increta (врастание плаценты в мышечный слой) и placenta percreta (прорастание плацентой всех слоев матки). Однако, гистологический диагноз выставляется ретроспективно и на его основании уже нельзя определить тактику ведения беременной, срок родоразрешения и объем оперативного вмешательства.
Обобщая данные мировой литературы, можно отметить, что тяжесть степени врастания плаценты и риск осложнений связан не столько с наличием и суммарным количеством в анамнезе факторов, повреждающих миометрий, и глубиной инвазии, сколько с топографией инвазии плаценты. При этом наиболее опасными являются случаи инвазии плаценты в заднюю стенку мочевого пузыря, параметрий, верхнюю 1/3 шейки матки. При подобном топографическом варианте врастания плаценты, возможность органосохраняющей операции стремится к нулю. Чаще всего подобная топография отмечается при истинном врастании. Возможно, это связано с дегенерацией тканей матки не локально, как при наличии рубца после кесарева сечения, а на всем участке, как результат многократных инвазивных вмешательств [7, 9, 12, 14].
При этом между плацентой и подлежащими тканями развивается разветвленная система сосудистых анастомозов [5, 12, 15, 16].
Клиническое наблюдение № 1
В ноябре 2019 г. в плановом порядке поступила пациентка К., 44 лет. Диагноз при поступлении: Беременность 33 недели 4 дня. Полное предлежание плаценты. Подозрение на врастание плаценты.
Данная беременность являлась 6-й, в анамнезе 3 своевременных самопроизвольных родов (2005, 2010, 2016 гг.), последние из которых осложнились плотным прикреплением плаценты, ручным обследованием послеродовой матки, отделением плаценты и выделением последа. Поздний послеродовый период осложнился гематометрой, причем в связи с развитием повторной картины гематометры выскабливание стенок послеродовой матки производилось четырехкратно. Стоит также отметить, что у пациентки в анамнезе два инструментальных аборта на сроках 10 недель беременности.
 Кроме того, в 2017 г. пациентке была произведена гистероскопия и раздельное диагностическое выскабливание в количестве 5 раз по поводу гиперплазии эндометрия. По результатам патоморфологического исследования данным за малигнизацию не обнаружено. Таким образом, данной пациентке произведено 11 внутриматочных манипуляций с травматизацией эндометрия, обоснованность которых вызывает сомнение.
Кроме того, в 2017 г. пациентке была произведена гистероскопия и раздельное диагностическое выскабливание в количестве 5 раз по поводу гиперплазии эндометрия. По результатам патоморфологического исследования данным за малигнизацию не обнаружено. Таким образом, данной пациентке произведено 11 внутриматочных манипуляций с травматизацией эндометрия, обоснованность которых вызывает сомнение.
Соматический анамнез не отягощен.
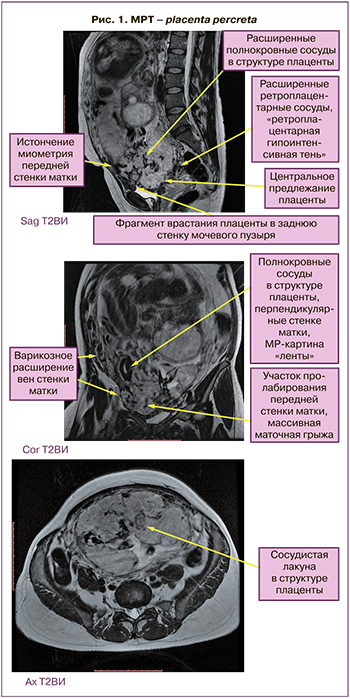
Данная беременность наступила самопроизвольно и протекала с ранних сроков на фоне низкой плацентации по данным эхографического исследования. В 19 недель беременности по данным эхографии впервые было заподозрено врастание плаценты в переднюю и боковые стенки матки на фоне полного предлежания плаценты. Диагноз был подтвержден в 22 недели при контрольном УЗИ и в 26 недель по данным МРТ. Плацента располагалась по передней стенке матки, полностью перекрывала область внутреннего зева, по передней стенке матки визуализировалась маточная грыжа размерами 6×7 см, расширенные вены плацентарной площадки, лакуны маточной части плаценты, задняя стенка мочевого пузыря четко не дифференцировалась. Предварительный диагноз – placenta percreta (рис. 1).
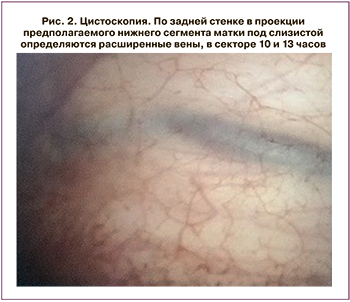
В качестве дополнительных диагностических мер с учетом данных МРТ и для выбора объема оперативного вмешательства, проведена цистоскопия.
По результатам цистоскопии выявлены неососуды истонченной задней стенки мочевого пузыря (рис. 2).
На сроке 35 недель произведена срединная лапаротомия, донное кесарево сечение. Извлечена живая недоношенная девочка. Оценка по шкале Апгар 7/8 баллов. Масса тела 2580 г, длина 45 см. Затем без тракций пуповина погружена в полость матки и разрез ушит двурядным викриловым швом [17].
 Интраоперационно в нижнем маточном сегменте визуализировалась маточная грыжа с деформированными контурами размерами 7×8 см, оплетенная сетью сосудистых извитых анастомозов с задней стенкой мочевого пузыря. При попытке отделения пузырно-маточной складки и низведении мочевого пузыря отмечалось кровотечение из патологической сети неососудов. Для остановки кровотечения использовались гемостатические швы и прицельная коагуляция сосудов биполяром [18].
Интраоперационно в нижнем маточном сегменте визуализировалась маточная грыжа с деформированными контурами размерами 7×8 см, оплетенная сетью сосудистых извитых анастомозов с задней стенкой мочевого пузыря. При попытке отделения пузырно-маточной складки и низведении мочевого пузыря отмечалось кровотечение из патологической сети неососудов. Для остановки кровотечения использовались гемостатические швы и прицельная коагуляция сосудов биполяром [18].
Низведение мочевого пузыря, предварительно наполненного стерильным раствором метиленового синего с целью лучшей визуализации контуров. В связи с врастанием плаценты в мочевой пузырь, произведена резекция участка передней стенки размерами 2×3 см. Дефект ушит.
Следующим этапом операции являлось осуществление комплексного компрессионного гемостаза. На момент осуществления турникетного гемостаза кровопотеря составляла 1500 мл. По краю грыжи в пределах здоровых тканей произведен разрез матки. Плацента полностью перекрывала область внутреннего зева, отмечались участки врастания плаценты в нижней 1/3 передней стенки матки, шейки матки и параметрий, верхней 1/3 задней стенки мочевого пузыря. Метропластика сопровождалась кровотечением из истонченной задней стенки матки, параметрия. Кровопотеря на данном этапе 3000 мл. Учитывая объем кровопотери, врастание плаценты в шейку матки, параметрий и отсутствие условий для органосохраняющей операции, произведена гистерэктомия.
Общая кровопотеря составила 3800 мл (1/3 от ОЦК), произведена реинфузия аутоэритроцитов в объеме 1500 мл с гематокритом 60, трансфузия свежезамороженной плазмы – в объеме 1800 мл, трансфузия эритроцитарной массы – 590 мл.
Длительность операции составила 3 часа 8 минут. Уровень гемоглобина до операции составлял 122 г/л, на 1-е сутки после – 83 г/л, на 5-е сутки – 95 г/л. По данным патоморфологического заключения выявлена placenta percreta на преобладающем участке исследуемой ткани и на ограниченном участке размером 0,7 см – placenta increta. Пациентка выписана на 10-е сутки в удовлетворительном состоянии.
Клиническое наблюдение № 2
Пациентка П., 37 лет. Диагноз при поступлении: Беременность 34 недели. Полное предлежание плаценты, подозрение на врастание плаценты. Отягощенный акушерско-гинекологический анамнез.
В анамнезе у пациентки 2 своевременных самопроизвольных родов (2005, 2010 гг.) и 3 инструментальных аборта (2015, 2016, 2018 гг.).
 Пациентке дважды проводилась гистероскопия и раздельное диагностическое выскабливанием по поводу полипов эндометрия. Данных за патологический рост эндометрия по результатам патоморфологического исследования не выявлено. Таким образом, данной пациентке произведено 5 внутриматочных манипуляций.
Пациентке дважды проводилась гистероскопия и раздельное диагностическое выскабливанием по поводу полипов эндометрия. Данных за патологический рост эндометрия по результатам патоморфологического исследования не выявлено. Таким образом, данной пациентке произведено 5 внутриматочных манипуляций.
Соматический анамнез не отягощен.
Беременность 6-я, наступила самопроизвольно. С ранних сроков по данным УЗИ диагностирована низкая плацентация. Беременная находилась на стационарном лечении в связи с угрозой прерывания беременности на фоне ретроплацентарной гематомы.
Диагноз врастания плаценты впервые был выставлен на основании данных ультразвукового исследования в 20 недель беременности. Врастание в переднюю стенку матки, заднюю стенку мочевого пузыря было подтверждено в 24 недели на контрольном УЗИ.
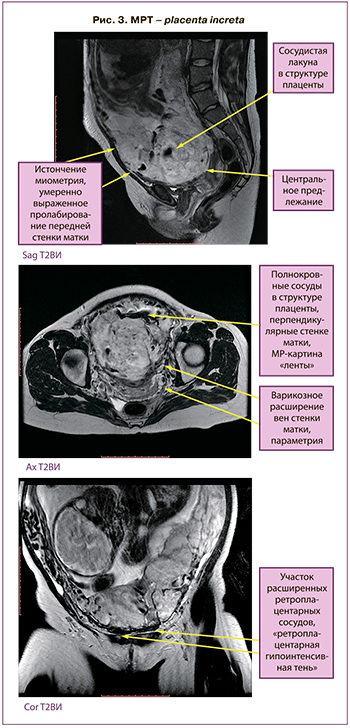
По данным МРТ, плацента располагалась по передней стенке матки, полностью перекрывала область внутреннего зева, по передней стенке матки визуализировалась маточная грыжа размерами 5×4 см, расширенные вены плацентарной площадки, лакуны маточной части плаценты, задняя стенка мочевого пузыря дифференцировалась. Предварительный диагноз – placenta increta (рис. 3).
При сроке беременности 35 недель 4 дня произведено оперативное родоразрешение: срединная лапаротомия, донное кесарево сечение. Операция производилась в условиях реинфузии аутоэритроцитов. Извлечен живой недоношенный мальчик. Оценка состояния по шкале Апгар 7/8 баллов. Масса тела 2478 г, длина 43 см.
Интраоперационно в нижнем маточном сегменте в месте врастания плаценты визуализировался участок с расширенными изветвленными сосудами размерами 5×5 см. Произведено рассечение брюшины пузырно-маточной складки, низведение мочевого пузыря по аналогии с предыдущем случаем.
Затем произведен турникетный гемостаз. Жгуты наложены билатерально и на шеечно-перешеечную области за счет сформированных искусственных «окон» в широких связках матки. После чего осуществлено иссечение участка передней стенки матки с вросшей плацентой. Определялся участок врастания плаценты в переднюю стенку матки, верхнюю 1/3 задней стенки мочевого пузыря, шейку матки и параметрий. Этап метропластики потребовал наложения дополнительных гемостатических швов на переднюю стенку матки и компрессионных на истонченную заднюю стенку матки. Также в связи с объемом кровопотери (1500 мл) и профилактикой отсроченного кровотечения произведена перевязка внутренних подвздошных артерий.
Общая кровопотеря составила 1700 мл (1/4 ОЦК) с реинфузией 680 мл (Ht 60), произведена трансфузия свежезамороженной плазмы в объеме 730 мл. Продолжительность операции 2 ч. По результатам патоморфологического заключения выявлены участки placenta increta. Пациентка выписана домой в удовлетворительном состоянии на 9-е сутки.
Клиническое наблюдение № 3
Пациентка Г., 47 лет. Диагноз при поступлении: Беременность 37 недель. ЭКО. Головное предлежание. Резус-сенсибилизация (титр АТ 1:2048–1:4096).
У пациентки в анамнезе самопроизвольные роды от первого брака. Гинекологический анамнез осложнен вторичным бесплодием в течение 9 лет (2-й брак, бесплодие, мужской фактор), в связи с чем успешно произведено экстракорпоральное оплодотворение.
В сроке беременности 18 отмечен рост резус антител 1:1–1:4–1:256. На момент госпитализации УЗ-признаков гемолитической болезни у плода не выявлено, титр антител 1:2048–1:4096.
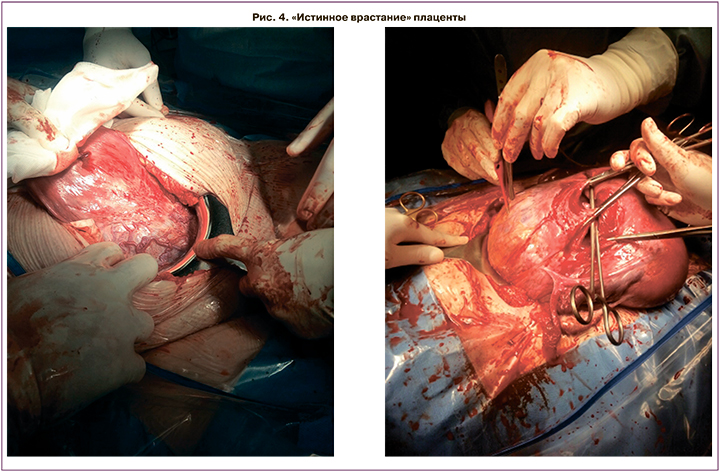
При сроке беременности 37 недель 2 дня в связи с нарастанием резус-сенсибилизации у пациентки с беременностью, наступившей в результате ЭКО и интергравидарным интервалом 22 года, произведено кесарево сечение. Извлечена живая девочка, оценка по шкале Апгар 8/9 баллов, масса 2410 г, длина 47 см. Интраоперационно диагностировано врастание плаценты, затрагивающее переднюю стенку и дно матки, попытка отделения плаценты без эффекта. Осуществить метропластику не удалось в связи с большой площадью врастания и массивной кровопотерей. Произведена перевязка подвздошных артерий, гистерэктомия. Общая кровопотеря составила 2000 мл (реинфузия аутоэритроцитов 400 мл с Ht 60, трансфузия свежезамороженной плазмы 1010 мл). Общая продолжительность операции 2 ч 26 мин.
По результатам патоморфологического заключения выявлен участок плотного прикрепления плаценты и участки с placenta accreta. Пациентка выписана домой в удовлетворительном состоянии на 6-е сутки.
Заключение
На сегодняшний день подавляющее количество врастаний плаценты связано с наличием рубца на матке и предлежанием плаценты. Другими факторами, предрасполагающими к развитию врастания плаценты, являются инструментальные внутриматочные вмешательства. Однако случаи врастания плаценты без рубца на матке встречаются крайне редко, что обусловлено диагностической сложностью. Такой тип врастания многие считают «истинным врастанием» (рис. 4). При этом врастание плаценты происходит по всей поверхности стенок матки и даже в дне.
В настоящее время отсутствуют четкие критерии диагностики врастания плаценты без рубца на матке, поэтому данный тип врастания чаще всего обнаруживается интраоперационно и является самым опасным. Часто хирурги, столкнувшиеся с такой ситуацией, не имеют соответствующей подготовки для выполнения органосохраняющей операции, что увеличивает риск массивной кровопотери и материнской смертности.
Только при своевременной диагностике «истинного врастания» возможно осуществление полноценной подготовки к операции. Для ранней постановки диагноза необходимо учитывать анамнез пациенток (многократные внутриматочные вмешательства с повреждением структуры миометрия), а также наличие предлежания плаценты по данным инструментальных обследований.
По нашему мнению, осуществить органосохраняющую операцию при «истинном врастании» крайне сложно, что связано с обширной площадью, топографией врастания и высоким риском материнских осложнений, а также необходимостью высокой квалификации хирургической бригады и условий предоперационной диагностики патологии.
Для снижения частоты патологической плацентации, необходимо с особой серьезностью подходить к вопросам, связанным с инвазивными вмешательствами на матке. Не только показания к кесареву сечению, должны быть обоснованными, но и любая инструментальная процедура на матке должны осуществляться только при абсолютной необходимости.



