Screening for serum thyroid-stimulating hormone levels in infertile women as the basis for predicting the outcomes of assisted reproductive technology programs
Objective. To estimate the blood levels of thyroid-stimulating hormone (TSH) in infertile women and to evaluate its effect on the outcome of infertility treatment using assisted reproductive technologies (ART). Subjects and methods. The study sample included 171 married couples with a confirmed diagnosis of infertility, who referred for IVF and IVF/ICSI in the period 2016 to 2017. All the female patients underwent superovulation induction in the IVF and IVF/ICSI program. Serum TSH levels were measured one month before the start of an ART session. Results. Medical records indicated that autoimmune thyroiditis was diagnosed in 56 (32.7%) of the examinees. Patients with a TSH concentration of less than 1.4 mIU/ml were statistically significantly more frequently observed to have a positive infertility treatment outcome manifested by the highest proportion of ART deliveries (75.8%) than in those with that of more than 1.4 mIU/ml (p <0.001). Conclusion. The given results show that the decrease in blood TSH levels to less than 1.4 mIU/ml before ART is associated with the higher incidence of clinical pregnancy resulting from ART.Paskar S.S., Kalugina A.S.
Keywords
Currently, screening for thyroid function in women with infertility before in vitro fertilization (IVF) is supported by many international communities [1, 2]. Ovarian stimulation during the IVF treatment is known to affect thyroid function not only due to excessive estrogenic activity but also directly, since receptors associated with the thyroid function were found in granulosa cells of human follicles and the endometrium. The relationship between ovarian stimulation and thyroid function has been investigated in several clinical studies. Some of them showed that controlled ovarian hyperstimulation during treatment cycles by assisted reproduction technologies (ART) induced a long-term (3 months after the end of the stimulation cycle) effect on the levels of thyroid-stimulating hormone (TSH), which was most pronounced in hypothyroid women [3]. It is extremely important to determine preconception levels of TSH. Among women with clinical hypothyroidism anticipating pregnancy, optimal preconception levels of TSH associated with better pregnancy outcomes are believed to be<2.5 mIU/mL [1, 4]. Other researchers suggest that in women with hypothyroidism who are planning to become pregnant, serum TSH levels should be in the normal range but should not be greater than about 1.2 mIU/mL [5].
Therefore, the vast majority of hypothyroid-treated women who achieve pregnancy through IVF need an increase in the dosage of thyroid hormone therapy during gestation, especially during the first 5-7 weeks’ gestation [6]. In the case of subclinical hypothyroidism, when TSH exceeds the threshold of 4.0 mIU/mL, levothyroxine therapy should be administered before the IVF program. Some authors suggest that the same intervention might also be justified for women with a TSH concentration of more than 2.5 mIU/mL before IVF [7].
The benefits of replacement levothyroxine therapy in the management of hypothyroid women were demonstrated by Busnelli A. et al. [8]. The authors reviewed the treatment protocols of hypothyroid-treated women who achieved a live birth through IVF. Patients with hypothyroidism undergoing IVF/intracytoplasmic sperm injection (ICSI) needed longer hormonal stimulation and also more often had low-quality embryos retrieved during fertilization and cultivation. However, no significant differences in the conception rates were observed. The authors emphasize that the absence of differences in the conception rates is associated with adequate replacement levothyroxine therapy. Therefore, adequate levothyroxine treatment maintaining TSH levels below 2.5 mIU/mL may overcome the detrimental effects of hypothyroidism in ART programs and improve the treatment effectiveness.
A serum TSH test is relatively inexpensive, accurate, and readily available, and taking into account the effectiveness of replacement levothyroxine therapy, mandatory screening of women for thyroid dysfunction before the ART program seems an optimal approach.
This study aimed to investigate the implication of testing serum TSH in infertile women to predict outcomes of infertility treatment with ART procedures.
Materials and methods
The study comprised 171 married couples with a confirmed diagnosis of infertility who applied for IVF and IVF/ICSI procedures from 2016 to 2017. The age of women ranged from 22 to 35 years. All patients underwent controlled ovarian hyperstimulation. We used standard stimulation schemes without additional modifications: a long gonadotropin-releasing hormone agonist protocol with preliminary pituitary desensitization or a gonadotropin-releasing hormone antagonists protocol. Fertilization and cultivation were carried out under the accepted standards of ART. After the completion of IVF and IVF/ICSI, the embryos were transferred to the uterine cavity, and hormonal support was administered for the period of early embryogenesis. The support continued until chorionic gonadotropin pregnancy test on day 12-14 after the embryo transfer, after which further management strategy was determined. Women with a positive human chorionic gonadotropin pregnancy test continued receiving early pregnancy support and on day 21 after the embryo transfer underwent ultrasonography to diagnose clinical pregnancy. Nine months after the onset of clinical pregnancy, the patients were followed by telephone interviews to register long-term outcomes of ART programs. Serum levels of TSH were measured one month before starting the ART procedure using chemiluminescent immunoassay. Patients with thyroid disease were consulted by an endocrinologist before starting infertility treatment. The results of this study included the assessment of the incidence of clinical pregnancy and childbirth after ART depending on TSH level.
This study was approved by the Research Ethics Committee of the I.P. Pavlov FSPbSMU of Minzdrav of Russia; written informed consent was obtained from all patients enrolled in the study. The study patient selection was carried out according to the inclusion and exclusion criteria.
Inclusion criteria were as follows: couples with an established diagnosis of tubal-peritoneal infertility or male factor infertility, external genital endometriosis, anovulation, as well as unspecified causes of infertility; a first cycle of IVF/ICSI treatment.
Exclusion criteria were as follows: women aged over 35 years, severe forms of oligoastenoteratozoospermia, azoospermia, and aspermia.
Statistical analysis was performed using STATISTICA 10.0 (StatSoft, Inc. 2007-2011) and SPSS, ver. 17.0 (SPSS Inc., USA) statistical software. The results were assessed with nonparametric statistics methods. Continuous variables are presented as median (Me) and interquartile range (25%; 75%). After testing the distribution of continuous variables for normality, the variables were compared with the two-sided Mann – Whitney test for independent samples. Categorical variables (in particular, binary ones) were analyzed using Pearson’s chi-squared test (χ2). Bonferroni correction was applied for multiple comparisons of binary variables. The critical level of significance when testing statistical hypotheses was considered at p <0.05.
Results
Before starting ART programs, clinical and anamnestic characteristics of infertile women (n = 171) were analyzed. Fifty-six (32.7%) of them had autoimmune thyroiditis, and 36 (21%) received replacement levothyroxine therapy depending on the presence of hypothyroidism and subclinical hypothyroidism. The mean serum TSH level in patients receiving replacement levothyroxine therapy for thyroid disease was 2.25 (2.0; 2.7) mIU/ml.
Therefore, baseline serum TSH concentration before starting infertility treatment of patients with thyroid disease was completely corrected.
According to the study objective, before starting the IVF protocol, the patients were divided into two groups categorized by serum TSH levels including 70 (41%) and 101 (59%) women with TSH level of <2.0 mIU/ml and ≥2.0-5.0 mIU/mL, respectively. The initial clinical and laboratory characteristics of the studied groups are presented in table 1.
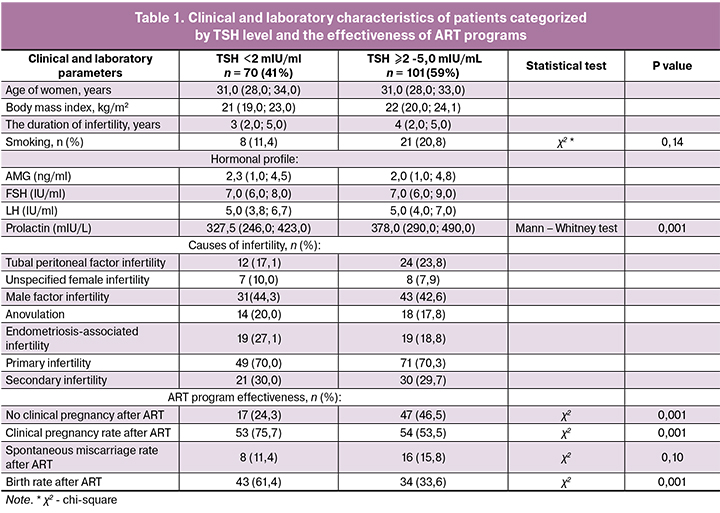
The mean age of 59.8%, 40%, and 4.6% of women undergoing ART procedures was 30 – 35, <30, and <25 years, respectively. The mean age of patients with TSH level <2.0 mIU/mL and ≥2.0-5.0 mIU/mL was 31 (28; 33) and 31 (28; 34) years, respectively. At the time of treatment, the duration of infertility ranged from 1 year to 3 years and from 3 to 5 years in 125 (73.2%) and 39 (22.7%) patients, respectively. The duration of infertile marriage in women with TSH level <2.0 mIU/mL and ≥2.0-5.0 mIU/mL was 3 (2; 5) and 4 (2; 5 ) years, respectively.
There were no statistically significant differences in age and duration of infertility between these groups.
It is worth noting that patients with TSH ≥2.0-5.0 mIU/mL were more likely to smoke (20.8%) than women with TSH <2.0 mIU/mL (11.4%); the difference was statistically significant at p = 0.14 (χ2 test).
In both groups, the most prevalent type of infertility was primary (70%) and male factor infertility (in 44.3% of patients with TSH <2.0 mIU/mL and in 42.6% of patients with TSH of ≥2.0 -5.0 mIU/ml). The second most common cause of infertility among patients with TSH <2.0 mIU/mL was infertility associated with endometriosis (27%), and in the group with TSH ≥2.0-5.0 mIU/mL - tubal peritoneal infertility (23.8%).
No statistically significant differences were observed between the study groups in the hormonal profiles. The level of anti-Muller hormone (AMH) was 2.3 (1.0; 4.5) and 2.0 (1.0; 4.8) ng/ml in the group with TSH <2.0 mIU/ mL and TSH ≥2.0-5.0 mIU/ml, respectively. Normal AMH concentrations are probably associated with the patients’ young age (women under 35 years), as well as with a high proportion of male factor infertility. It should be noted that the patients with TSH ≥2.0-5.0 mIU/mL had slightly higher serum prolactin levels. The prolactin level in the group with TSH ≥2.0-5.0 mIU/mL was 378.0 (290.0; 490.0) mIU/mL versus 327.5 (246.0; 423.0) mIU/mL in group with TSH <2.0 mIU/ml; the difference was statistically significant (p = 0.006, Mann – Whitney test).
Patients with TSH ≥2-5.0 mIU/mL significantly more often failed to achieve a clinical pregnancy after ART (47%) than patients with TSH <2.0mIU/mL (24.3%). Besides, women with TSH ≥2.0-5.0 mIU/mL were less likely to achieve positive long-term outcomes of the ART procedure (relative birth rate was 33.6%). At the same time, they had a rather high early spontaneous miscarriage rate after the end of the IVF procedures. The statistical significance of the differences between groups of patients is presented in table 1. In particular, as seen from table 1, women with a TSH level <2 mIU/mL had two times fewer early spontaneous miscarriages after ART than patients with TSH ≥ 2.0-5.0 mIU/ml.
The relationship between serum TSH level and pregnancy outcomes was analyzed using Pearson’s chi-square test for 2x2 contingency tables.
Depending on the TSH values and taking into account a sufficient number of observations for conducting a multiple comparative analysis, the sample was divided into four subgroups (Table 2).
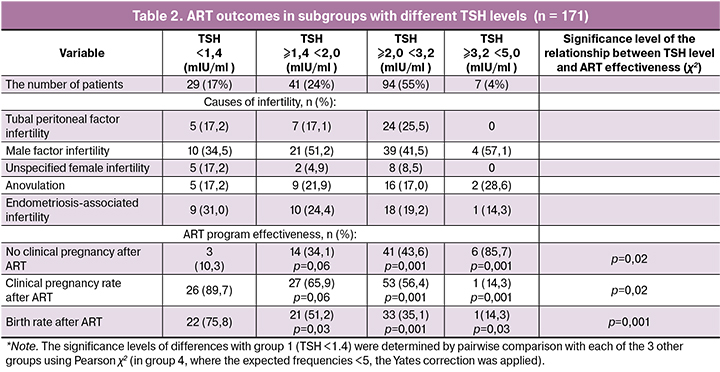
The patients with TSH levels below1.4 mIU/mL had the lowest rate of negative IVF outcomes (10.3%) and the highest birth rate after IVF (75.8%), compared with other groups. The most significant difference (p = 0.001) was observed with group 4 with TSH values of ≥3.2 - 5.0 mIU/ml. Therefore, a TSH level below 1.4 mIU/mL is associated with a positive treatment outcome, namely, a live birth.
Discussion
Some studies have been focused on the fact that autoimmune thyroiditis is more common among women with infertility [9, 10]. In this study, 32.7% of participants had autoimmune thyroiditis, which is consistent with the relevant literature and confirms the high prevalence of thyroid disease among patients with infertility.
The international literature [11] has reported some evidence on an association between subclinical hypothyroidism with an increased risk of adverse pregnancy outcomes, including spontaneous miscarriages. The present study demonstrated that with a decrease in TSH <2 mIU/ml is associated with a two-fold decrease in the rate of early spontaneous miscarriage. However, given the fact that all patients with thyroid diseases in the presented study received adequate replacement levothyroxine therapy before starting the IVF protocol, no significant reliability could be identified on this issue.
The benefits of replacement levothyroxine therapy have been proven in numerous studies [6, 7, 11]. This study demonstrated an adequate correction of the TSH level before starting the ART protocol. Thus, the serum TSH level in patients receiving therapy for thyroid disease was 2.25 mIU/ml, which justifies the administration of levothyroxine as a rather effective treatment for hypothyroidism.
The optimal TSH level before starting the ART protocol has been a subject of debate in the literature. Currently, available evidence suggests that optimal preconception levels of TSH levels should not exceed 2.5 mIU/mL [1, 4], though some report them to be 1.2 mIU/mL [12]. In the present work, a significant relationship was found between the serum TSH level below1.4 mIU/mL and the positive long-term outcomes of infertility treatment using IVF. These results once again focus on the relativity of the recommended TSH threshold of 2.5 mIU/ml before IVF. Data on a significant effect of a TSH level below 1.4 mIU/mL may play an important role in counseling services for preparing couples for ART programs.
Conclusion
The study findings show that a decrease in the serum TSH to a level below 1.4 mIU/mL before ART is associated with a higher rate of positive outcomes of infertility treatment using IVF. However, further studies are needed to determine the relationship between TSH levels and the miscarriage after ART.
References
- Stagnaro-Green A., Abalovich M., Alexander E., Azizi F., Mestman J., Negro R. et al. Guidelines of the American Thyroid Association for the diagnosis and management of thyroid disease during pregnancy and postpartum. Thyroid. 2011; 21(10): 1081-125. https://doi.org/10.1089/thy.2011.0087
- Rijal B., Shrestha R., Jha B. Association of thyroid dysfunction among infertile women visiting infertility center of Om Hospital, Kathmandu, Nepal. Nepal Med. Coll. J. 2011; 13(4): 247-9.
- Busnelli A., Somigliana E., Ferrari S., Filippi F., Vannucchi G., Fugazzola L., Fedele L. The long-term impact of controlled ovarian hyperstimulation on thyroid function. Endocr. Pract. 2016; 22(4): 389-95. https://doi.org/10.4158/EP15933
- Перминова С.Г. Бесплодие у женщин с патологией щитовидной железы: принципы диагностики, тактика ведения: автореф. дисс. ... д-ра мед. наук. М.; 2010. 49 с.[Perminova S.G. Infertility in women with thyroid disease: principles of diagnosis, management tactics. Author’s abstract dis. ... Dr. med sciences. M., 2010. 49 p.(InRuss.)]
- Abalovich M., Alcaraz G., Kleiman-Rubinsztein J., Pavlove M.M., Cornelio C., Levalle O., Gutierrez S. The relationship of preconception thyrotropin levels to requirements for increasing the levothyroxine dose during pregnancy in women with primary hypothyroidism. Thyroid. 2010; 20(10): 1175-8. https://doi.org/10.1089/thy.2009.0457
- Busnelli A., Vannucchi G., Paffoni A., Faulisi S., Fugazzola L., Fedele L., Somigliana E. Levothyroxine dose adjustment in hypothyroid women achieving pregnancy through IVF. Eur. J. Endocrinol. 2015; 173(4): 417-24. https://doi.org/10.1530/EJE-15-0151
- Mintziori G., Goulis D.G., Kolibianakis E.M. Thyroid function and IVF outcome: when to investigate and when to intervene? Curr. Opin. Obstet. Gynecol. 2016; 28(3): 191-7. https://doi.org/10.1097/GCO.0000000000000263.
- Busnelli A., Somigliana E., Benaglia L., Leonardi M., Ragni G., Fedele L. In vitro fertilization outcomes in treated hypothyroidism. Thyroid. 2013; 23(10): 1319-25. https://doi.org/10.1089/thy.2013.0044
- Verma I., Sood R., Juneja S., Kaur S. Prevalence of hypothyroidism in infertile women and evaluation of response of treatment for hypothyroidism on infertility. Int. J. Appl. Basic Med. Res. 2012; 2(1): 17-9.
- Перминова С.Г. Бесплодие у женщин с заболеваниями щитовидной железы: принципы диагностики, тактика ведения. Акушерство и гинекология: новости, мнения, обучение. 2013; 2: 18-24.[Perminova S.G. Infertility in women with thyroid diseases: principles of diagnosis, management tactics. Obstetrics and gynecologists: news, opinions, training. 2013; 2: 18-24.(InRuss.)]
- Maraka S., Mwangi R., McCoy R.G., Yao X., Sangaralingham L.R., Singh Ospina N.M. et al. Thyroid hormone treatment among pregnant women with subclinical hypothyroidism: US national assessment. BMJ. 2017; 356: i6865. https://doi.org/10.1136/bmj.i6865.
- Reh A., Grifo J., Danoff A. What is a normal thyroid-stimulating hormone (TSH) level? Effects of stricter TSH thresholds on pregnancy outcomes after in vitro fertilization. Fertil. Steril. 2010; 94(7): 2920-2. https://doi.org/10.1016/j.fertnstert. 2010.06.041.
Received 19.11.2019
Accepted 07.12.2018
About the Authors
Paskar Svetlana S., PhD student of the Department of Obstetrics and Gynecology and Neonatology, Pavlov of First Saint Petersburg State Medical University.https://orcid.org/0000-0002-9308-324; 8-921-417-43-77, paskarsvetlana@mail.ru
197022 Russia, Saint Petersburg, L’va Tolstogo st., 6/8.
Kalugina Alla S., MD, Professor of the Department of Obstetrics and Gynecology and Neonatology, Pavlov of First Saint Petersburg State Medical University; deputy chief medical officer of «AVA-Peter» Clinic. 197022 Russia, Saint Petersburg, L’va Tolstogo st., 6/8;
191186 Russia, Saint-Petersburg, Nevsky pr., 22-24/
For citation: Paskar S.S., Kalugina A.S. Screening for serum thyroid-stimulating hormone levels in infertile women as the basis for predicting the outcomes of assisted reproductive technology programs.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology.2019; 8:78-83 (in Russian).
https://dx.doi.org/10.18565/aig.2019.8.78-83