Impact of noninvasive respiratory therapy in pregnant women with early severe preeclampsia on the levels of preeclampsia markers and mitochondrial DAMPs
Objective. To evaluate the clinical efficiency of continuous positive airway pressure (CPAP) therapy in the treatment of early severe preeclampsia according to clinical and laboratory findings and mitochondrial damage-associated molecular pattern (DAMP) levels.Skovorodina T.V., Vishnyakova P.A., Tsvirkun D.V., Shmakov R.G., Vysokikh M.Yu., Kalachin K.A., Pyregov A.V.
Material and methods. Blood biochemical tests were carried out to measure laboratory parameters (ALT, AST, AP, and LDH) and general urinalysis was used to identify proteinuria (PU) in women with severe preeclampsia before and after CPAP therapy. Microvesicle fractions were obtained from the plasma of female patients by differential centrifugation. The levels of L-ОРА1- and pre-TFAM were determined by chemiluminescent Western blotting.
Results. A significant decrease was found in the level of placental growth factor (PlGF), soluble fms-like tyrosine kinase 1 (sFlt-1), ALT, and PU indicators after one CPAP therapy cycle in patients with early severe preeclampsia. There was also a decline in the content of L-OPA1, a probable prognostic marker for severe preeclampsia.
Conclusion. The efficiency of CPAP therapy is confirmed by a decrease in the values of key clinical markers for preeclampsia, including the mtDAMP marker L-OPA1.
Keywords
A method for treating obstructive sleep apnea by creating a constant positive pressure in the airways was proposed by C.E. Sullivan et al. in 1981 [1]. The method was called CPAP-therapy, from the English abbreviation of the underlying mode of artificial ventilation of the lungs – Continuous Positive Airway Pressure (constant positive pressure in the airways). The essence of the technique is to create a constant positive pressure in the airways by the apparatus during the entire cycle of respiration through a tightly fitting facial mask. CPAP therapy is effective in people suffering from sleep apnea every night during the whole time of sleep. At the same time, there is an improvement in both the quality of sleep and daily activity. During sleep, due to the created air pressure, the patient’s upper respiratory tract is ensured.
An important risk factor for obstructive sleep apnea is pregnancy [2]. Anatomical and physiological changes (such as increased weight, a position during sleep on the back, reduced functional residual lung volume) that occur during pregnancy, affect the respiratory system, which creates conditions for increasing the frequency of sleep apnea. Also during pregnancy there is an increase in the blood supply to the capillaries of the respiratory mucosa, which thus narrows their lumen [3].
Some authors have associated sleep apnea syndrome with obstetric complications such as preeclampsia (PE), fetal growth retardation syndrome and antenatal fetal death [4]. A number of researchers hypothesized that intermittent nocturnal hypoxemia during obstructive sleep apnea leads to activation of the sympathetic nervous system, the development of endothelial dysfunction and oxidative stress [5]. PE is also associated with a systemic inflammatory response, endothelial dysfunction, and an imbalance of angiogenic and antiangiogenic factors [6]. Such mechanisms of vascular damage suggest a possible single pathogenetic pathway for the development of early PE in women with obstructive sleep apnea.
Recently, there are works devoted to the study of the effect of CPAP therapy on the course of pregnancy complicated by PE. A pilot prospective study of 12 pregnant women with PE was performed by Guilleminault et al. [7]. The study included 2 women with PE in anamnesis, 7 women with chronic hypertension, and 3 women with obesity. All women received nighttime CPAP therapy throughout pregnancy from its early stages (7.5 weeks of gestation). In women with chronic arterial hypertension, blood pressure was less than 140/90 mm Hg. st. throughout pregnancy without need for adjustment of drug therapy, and all these pregnancies ended in full-term with the birth of healthy children. Of the two women who had a history of PE, only one also developed PE, however, pregnancy with CPAP therapy was prolonged until 30 weeks.
Subsequently, based on the results of their first study, Poyares et al. reported a second randomized study that aimed to evaluate the potential efficacy of applying constant positive airway pressure [8]. Pregnant women with hypertension who received standard prenatal care and CPAP therapy (treatment group) were compared with pregnant women with hypertension who received methyldopa (control group). PE developed in one patient. In the treatment group, it was noted that blood pressure was significantly lower than in the control group. Also reduced doses of the necessary antihypertensive drugs. All newborns from mothers in the treatment group had an Apgar score of 1 minute higher than newborns from mothers in the control group.
Thus, existing studies to date show that the use of intensive care with respiratory CPAP support in pregnant women with hypertension can reduce the drug load and improve the perinatal outcome of pregnancy. However, this issue still needs careful study, which necessitates further research.
During oxidative stress in the placenta, intense syncytiotrophoblast shedding occurs, resulting in the appearance of various components, so-called DAMP (Damage Associated Molecular Patterns), in the feto-placental and maternal bloodstream, which have a pronounced pro-inflammatory effect and stimulate the activation and inflammation of the endothelial cells in the mother’s body [9]. The most studied of the mitochondrial DAMPs (mtDAMPs) are mitochondrial DNA (mtDNA), N-formyl peptide, miRNA, which are associated with the regulation of mitochondrial activity. McCarthy and Kenny study showed that PE is associated with a 5-fold increase in the amount of mtDNA in the maternal plasma, which leads to the activation of the immune response; accordingly, the number of pro-inflammatory cytokines increases, followed by the occurrence of endothelial dysfunction [10].
There are other mtDAMPs, such as TFAM, the most important player in replication and transcription of mtDNA; OPA1 protein, the main function of which is the realization of the fusion of internal mitochondrial membranes and mitochondrial membrane channel – VDAC1. Data concerning the involvement of mentioned proteins in pathology development are practically not found in scientific literature.
Since several studies have shown that CPAP therapy improves endothelial function, reduces oxidative stress and systemic inflammation [11], it could be suggested that the usage of CPAP therapy in pregnant women can enhance the immune system and thus reduce the immunogenic load in pathological conditions. This allows to develop an adaptive response to systemic inflammation: the number of syncytiotrophoblast particles in the maternal and fetoplacental blood flow decreases, which leads to the decrease of the mitochondrial DAMPs level [12].
This work aims to evaluate the clinical efficacy of CPAP therapy in the treatment of severe PE based on clinical and laboratory data and levels of mitochondrial DAMPs.
Material and research methods
The study included 20 pregnant women with early severe PE diagnosed according to the criteria of the International Statistical Classification of Diseases and Health Problems of the 10th revision. They were divided into 2 groups – in the 1st group, standard drug therapy was used in combination with CPAP therapy (group 1 – n = 10), in the 2nd group only standard drug therapy was used (2nd group, n = 10). CPAP therapy in the 1st group was conducted by courses, the average night duration of one course of therapy was 6 hours.
A comprehensive assessment of the health status of pregnant women was carried out using physical, clinical, laboratory and functional research methods, the average periods of pregnancy prolongation were evaluated, and outcomes for newborns were compared. Also, Western blot analysis with chemiluminescence detection was used to perform a comparative analysis of the relative content of mitochondrial proteins (pre-TFAM, OPA1-L) in the microvesicular plasma fraction of patients with severe PE before and after CPAP therapy courses. The levels of hepatic enzymes (alanine aminotransferase – ALT, aspartate aminotransferase – AST), lactate dehydrogenase (LDH), alkaline phosphatase (alkaline phosphatase), platelet count, placental growth factor (PlGF), sFlt-1 (soluble fms-like protein, ianthropylamine) were studied before and after courses CPAP therapy.
Research results and discussion
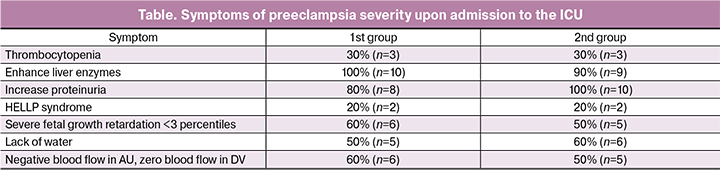
A severe form of PE has developed in 14 multigravida and in 6 primigravida. The main criteria for PE were: increased diastolic blood pressure ≥ 110 mmHg. Art., systolic blood pressure ≥ 160 mm Hg. st. in all 20 patients, thrombocytopenia (less than 100 * 109 / l) in 6 patients, elevated liver enzymes in 19 patients, increased proteinuria in 18 patients, the development of HELLP syndrome in 4 patients out of 20, and also in both groups fetus (table).
In the 1st group, an increase in sFlt-1, as well as the ratio of sFlt-1 / PlGF (which, according to recent data, indicates the risk of preterm birth [13]), was observed in 100% of cases. In the 2nd group, the increase occurred in 80% of cases (n = 8).
In both groups, PE developed against the background of previous chronic hypertension in 2 women (20%). The manifestation of severe PE symptoms on average in the 1st group occurred during gestation 26.64 ± 2.01 weeks, in the 2nd group – 27.56 ± 2.65 weeks.
The treatment of PE was carried out in accordance with generally accepted standards and included: magnesia, infusion therapy, two- or three-component antihypertensive therapy regimens, as well as anticoagulant therapy. Magnesia, as well as anticoagulant therapy, was received by 100% of patients in both groups. On the two-component scheme of antihypertensive therapy there were 9 (90%) patients of the 1st group and 8 (80%) patients of the 2nd group. Three-component therapy was used in 1 and 2 cases, respectively. The number of courses of CPAP therapy in the 1st group averaged 6.10 ± 1.27.
The use of CPAP therapy allowed to reduce the drug load after 1 course of use (the dose of antihypertensive drugs was reduced) in 2 (20%) cases.
In the group with the use of CPAP therapy, it was significantly more often the cause of delivery was the deterioration of the fetus (7 cases in the 1st group, 5 cases in the 2nd group) compared with the group with standard drug therapy (p < 0.01); at the same time, in the 2nd group, the severity of PE increased significantly more compared with the 1st group (p < 0.05), as a result of which a decision was made on the need for delivery (3 cases in the 1st group and 5 cases in the 2nd group).
In this way, it can be assumed that the use of constant positive pressure in the airways, in addition to drug therapy, relieves the symptoms of PE more often and more progressively, without significantly affecting the hemodynamics of the mother-placenta-fetus system.
In the group with traditional medical support, the duration of pregnancy prolongation ranged from 0 to 6 days maximum (average 2.5 days), whereas in the group where, in addition to drug therapy, CPAP respiratory support was performed, the duration of pregnancy prolongation ranged from 4 to 12 days (average 6.3 days). With the expectant management tactics, the term of prolongation of pregnancy in patients in the 1st group was higher on average by 3.8 days than in the 2nd group (p < 0.05).
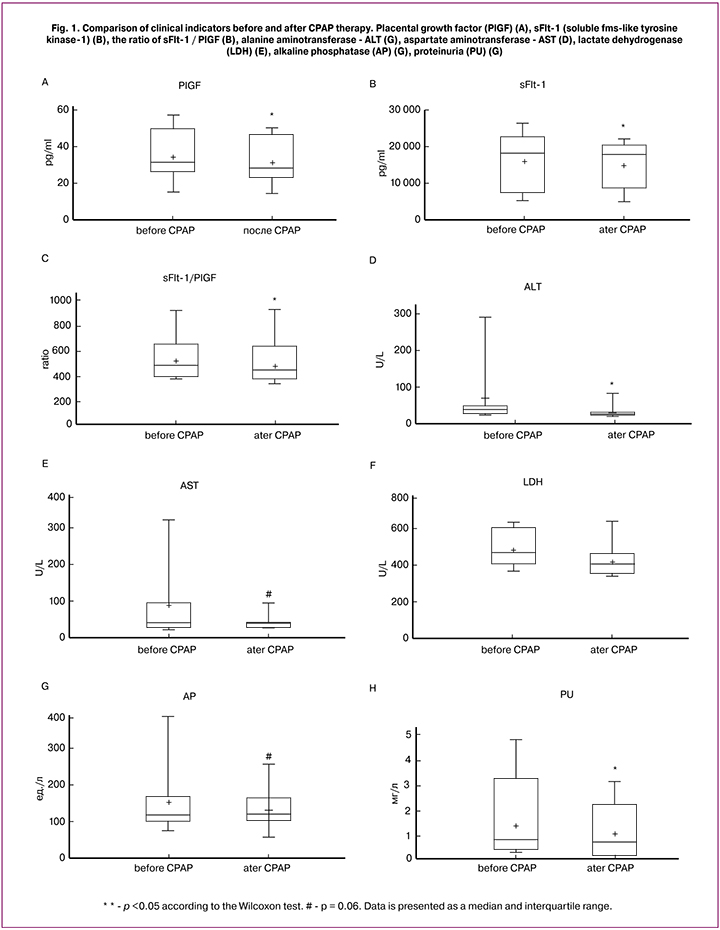
The study in group 1 showed a significant decrease in the levels of sFlt-1, PlGF, the relationship of sFlt-1 / PlGF, ALT in the blood of pregnant women even during one course of CPAP therapy. There was a significant decrease in proteinuria (Fig. 1). There was also a tendency to a decrease in the level of AST and alkaline phosphatase after CPAP therapy (p = 0.06). In the 2nd group, no decrease in the level of hepatic enzymes was observed, as well as proteinuria and sFlt-1, PlGF, and the sFlt-1 / PlGF ratio throughout the prolongation of pregnancy.
According to the questionnaire, 9 out of 10 women underwent CPAP therapy without any unpleasant sensations, and only in 1 case there was a complaint about difficulties in falling asleep due to the inconvenience from the pressure of the facial mask on the nose bridge. Also in 30% (n = 3), an improvement in the quality of sleep and general well-being after the start of CPAP therapy was subjectively noted.
When analyzing neonatal outcomes, it was noted that in the 1st group, the necessity for invasive respiratory support methods in newborns was significantly reduced (10%), whereas in the 2nd group, standard artificial respiration was used in 40% of cases (p < 0.05), as well as significantly reduced the need for the introduction of surfactant – in 70% in the 1st group, in 90% – in the 2nd group (p < 0.05). The length of stay in the neonatal intensive care unit was not statistically significantly different. Significant differences in the incidence of newborns between the groups with expectant management of pregnancy were also not found.
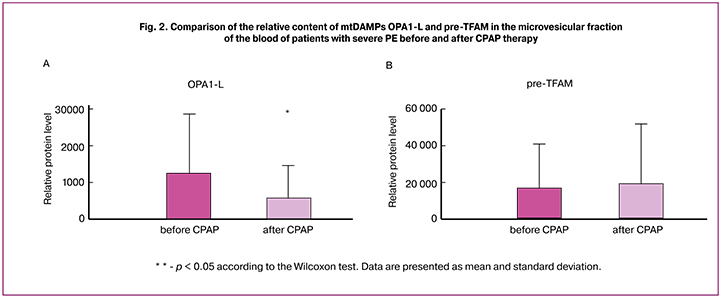
In our previous work we found that the presence of the OPA1-L and pre-TFAM proteins in blood microvesicles may be considered to be a prognostic marker and an indicator of the severity of PE [14]. The level of OPA1-L protein was increased in plasma microvesicles of patients with severe PE. Correlation between pre-TFAM level in microvesicles and proteinuria was also found. This makes OPA1-L and pre-TFAM likely candidates for mtDAMPs associated with severe PE.
In the present study, OPA1-L and pre-TFAM were measured in plasma microvesicles of women before and after CPAP therapy. It was found that the relative level of OPA1-L protein, that is the complete form of OPA1 responsible for fusion of the internal mitochondrial membranes, was significantly decreased already after the 1st course of CPAP therapy (Fig. 2A). Together with revealed significant changes in the main clinical indices (sFlt-1/PlGF, ALT and proteinuria) OPA1-L in microvesicles could be an important indicators of changes in the patient’s state. It can be supposed that CPAP therapy contributes to the normalization of the cardiovascular functioning and therefore leads to the decrease of mtDAMP OPA1-L level. We didn’t observe any significant changes of pre-TFAM content in microvesicles before and after CPAP.
Conclusion
We can conclude that application of CPAP respiratory support in the case of pregnancy complicated by PE assists in longer prolongation of pregnancy, decrease in drug loading during pregnancy and in more effective use of antihypertensive therapy. In this connection, an improvement in perinatal outcomes, a decrease in frequency of disease incidence in newborns and decrease in duration of stay in intensive care units are expected. CPAP therapy is a promising method for relieving symptoms of PE, but further detailed studies still needed for better as underlying mechanisms of action are not fully understood.
It is important to note that prolongation of pregnancy in patients with severe PE by CPAP therapy is possible only in perinatal centers of the 3rd level with adequate equipment, wide functionality of the anesthesiology, resuscitation and intensive care units both for adults and newborns, and the ability to provide high-tech patient care.
References
1. Issa F.G., Berthon-Jones M., Eves L. Reversal of obstructive sleep apnoea by continuous positive airway pressure applied through the nares. Lancet. 1981; 1(8225): 862-5.
2. Sahota P.K., Jain S.S., Dhand R. Sleep disorders in pregnancy. Curr. Opin. Pulm. Med. 2003; 9(6): 477-83.
3. Романова В.В., Горшинова В.К., Шмаков Р.Г., Шифман Е.М. Роль сонного апноэ в развитии преэклампсии. Акушерство и гинекология. 2012; 4-2: 4-9. [Romanova V.V., Gorshinova V.K., Shmakov R.G., Shifman E.M. Role of sleep apnea in the development of preeclampsia. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2012; 4-2: 4-9. (in Russian)]
4. Kapsimalis F., Kryger M. Obstructive sleep apnea in pregnancy. Sleep Med. Clin. 2007; 2: 603-13.
5. Gozal D., Kheirandish-Gozal L. Cardiovascular morbidity in obstructive sleep apnea oxidative stress, inflammation, and much more. Am. J. Respir. Crit. Care Med. 2008; 177(4): 369-75.
6. Ходжаева З.С., Коган Е.А., Клименченко Н.И., Акатьева А.С., Сафонова А.Д., Холин А.М., Вавина О.В., Сухих Г.Т. Клинико-патогенетические особенности ранней и поздней преэклампсии. Акушерство и гинекология. 2015; 1: 12-7. [Khodzhaeva Z.S., Kogan E.A., Klimenchenko N.I., Akatyeva A.S., Kholin A.M., Vavina O.V., Sukhikh G.T. Clinical and pathogenetic features of early and late preeclampsia. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2015; 1: 12-7. (in Russian)]
7. Visasiri Tantrakul, Jee Hyun Kim, Christian Guilleminault. Continuous positive airway pressure as a potential treatment for preeclampsia. Open Sleep J. 2013; 6(Suppl. 1: M5): 37-43.
8. Poyares D., Guilleminault C., Hachul H., Fujita L., Takaoka S., Tufik S., Sass N. Preeclampsia and nasal CPAP: Part 2. Hypertension during pregnancy, chronics noring, and early nasal CPAP intervention. Sleep Med. 2007; 9(1): 15-21.
9. Tong M., Johansson C., Xiao F., Stone P.R., James J.L., Chen Q. et al. Antiphospholipid antibodies increase the levels of mitochondrial DNA in placental extracellular vesicles: Alarmin-g for preeclampsia. Sci. Rep. 2017; 7(1): 16556.
10. Wenceslau C.F., McCarthy C.G., Szasz T., Spitler K., Goulopoulou S., Webb R.C. Mitochondrial damage-associated molecular patterns and vascular function. Eur. Heart J. 2014; 35(18): 1172-7.
11. Hopps E., Caimi G. Obstructive sleep apnea syndrome: links betwen pathophysiology and cardiovascular complications. Clin. Invest. Med. 2015;38(6): E362-70.
12. Сковородина Т.В., Вишнякова П.А., Шмаков Р.Г., Высоких М.Ю. Роль митохондриальных маркеров в патогенезе преэклампсии и оценка эффективности респираторной терапии в лечении преэклампсии. Акушерство и гинекология. 2017; 6: 5-9. [Skovorodina T.V., Vishnyakova P.A., Shmakov R.G., Vysokikh M.Yu. The role of mitochondrial markers in the pathogenesis of preeclampsia and the evaluation of the efficiency of respiratory therapy in the treatment of preeclampsia. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2017; (6): 5-9. (in Russian)] http://dx.doi.org/10.18565/aig.2017.6.5-9
13. Hoffmann J., Ossada V., Weber M., Stepan H. An intermediate sFlt-1/PlGF ratio indicates an increased risk for adverse pregnancy outcome. Pregnancy Hypertens. 2017;10: 165-70.
14. Сковородина Т.В., Вишнякова П.А., Цвиркун Д.В., Шмаков Р.Г., Высоких М.Ю. Роль митохондриальных молекул, ассоциированных с повреждением, в манифестации гипертензивных осложнений беременности. Акушерство и гинекология. 2017; 12: 84-8. [Skovorodina T.V., Vishnyakova P.A., Tsvirkun D.V., Shmakov R.G., Vysokikh M.Yu. Role of mitochondrial DAMPs in the manifestation of hypertensive complications of pregnancy. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2017; (12): 84-8. (in Russian)] https://dx.doi.org/10.18565/aig.2017.12.84-88
Received 06.04.2018
Accepted 20.04.2018
About the Authors
Skovorodina, Tatiana V., graduate student of National Medical Research Center of Obstetrics, Gynecology, and Perinatology named after Academician V.I. Kulakov,Ministry of Health of Russia. 117997, Russia, Moscow, Ac. Oparina str. 4. E-mail: t_skovorodina@oparina4.ru
Vishnyakova, Polina A., Researcher, Laboratory of Mitochondrial Medicine, National Medical Research Center of Obstetrics, Gynecology, and Perinatology named
after Academician V.I. Kulakov, Ministry of Health of Russia. 117997, Russia, Moscow, Ac. Oparina str. 4. E-mail: p_vishnyakova@oparina4.ru
Tsvirkun, Daria V., Senior Researcher, Laboratory of Mitochondrial Medicine, National Medical Research Center of Obstetrics, Gynecology, and Perinatology named
after Academician V.I. Kulakov, Ministry of Health of Russia. 117997, Russia, Moscow, Ac. Oparina str. 4. E-mail: darunyat@gmail.com
Shmakov, Roman G., Professor, Doctor of Medical Sciences, Chief Physician, National Medical Research Center of Obstetrics, Gynecology, and Perinatology named
after Academician V.I. Kulakov, Ministry of Health of Russia. 117997, Russia, Moscow, Ac. Oparina str. 4. E-mail: r_shmakov@oparina4.ru
Vysokikh, Mikhail Yu., Ph.D., head. laboratory of mitochondrial medicine, National Medical Research Center of Obstetrics, Gynecology, and Perinatology named
after Academician V.I. Kulakov, Ministry of Health of Russia. 117997, Russia, Moscow, Ac. Oparina str. 4. E-mail: m_vysokikh@oparina4.ru
Kalachin, Konstantin A., doctor of the anesthesiology and intensive care unit, National Medical Research Center of Obstetrics, Gynecology, and Perinatology named
after Academician V.I. Kulakov, Ministry of Health of Russia. 117997, Russia, Moscow, Ac. Oparina str. 4. E-mail: k_kalachin@oparina4.ru
Pyregov, Aleksey V., MD, Head of the Department of Anesthesiology and Resuscitation, National Medical Research Center of Obstetrics, Gynecology, and Perinatology named after Academician V.I. Kulakov, Ministry of Health of Russia. 117997, Russia, Moscow, Ac. Oparina str. 4. E-mail: a_pyregov@oparina4.ru
For citations: Skovorodina T.V., Vishnyakova P.A., Tsvirkun D.V., Shmakov R.G., Vysokikh M.Yu., Kalachin K.A., Pyregov A.V. Impact of noninvasive respiratory therapy in pregnant women with early severe preeclampsia on the levels of preeclampsia markers and mitochondrial DAMPs. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2018; (10): 52-8. (in Russian)
https://dx.doi.org/10.18565/aig.2018.10.52-58