Effect of preconceptional cervical electroconizationon the course of pregnancy and childbirth
Rosyuk E.A., Oboskalova T.A., Emelyanova E.S., Butorina N.V., Emelyanova T.G., Glukhov E.Yu., Neff E.I., Yakushev A.M.
Objective: This study aimed to investigate the impact of preconceptional cervical electroconization on the course of pregnancy and childbirth.
Materials and methods: This study compared the pregnancy course and birth outcomes of women who underwent preconceptional electroconization (n=50) with those without cervical pathology (n=48). Statistical analysis was performed using descriptive statistics in an Excel spreadsheet, and comparative analysis was conducted using Fisher's exact test.
Results: Among the pregnant women with a history of cervical electroconization, 34% had cardiovascular disease, 32% had gastrointestinal disease, 14% had neurological disease, 6% had Rh-negative blood, 14% had myomas, 10% were infertile, and 4% had congenital genital malformations. Women with a history of cervical electroconization were more likely to experience isthmic cervical insufficiency (10%) during pregnancy. The percentage of preterm births was higher in women with a history of cervical electroconization than in those without. Labor induction was performed in 22% of the cases, and labor augmentation with oxytocin was performed 7% less frequently than in women without a history of electroconization.
Conclusion: A history of cervical electroconization was associated with a higher prevalence of somatic and gynecological pathologies. However, it did not increase the frequency of cesarean sections or labor induction with oxytocin. No negative effects on the fetus were observed.
Authors' contributions: Rosyuk E.A., Yakushev A.M., Oboskalova T.A., Glukhov E.Yu., Neff E.I. – conception and design of the study; Emelyanova E.S., Butorina N.V., Emelyanova T.G. – material collection and processing; Rosyuk E.A. – statistical analysis, drafting of the manuscript.
Conflicts of interest: The authors have no conflicts of interest to declare.
Funding: There was no funding for this study.
Ethical Approval: The study was reviewed and approved by the Research Ethics Committee of the Ural State Medical University.
Patient Consent for Publication: All patients provided informed consent for the publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available upon request from the corresponding author after approval from the principal investigator.
For citation: Rosyuk E.A., Oboskalova T.A., Emelyanova E.S., Butorina N.V.,
Emelyanova T.G., Glukhov E.Yu., Neff E.I., Yakushev A.M.
Effect of preconceptional cervical electroconizationon the course of pregnancy and childbirth.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2024; (6): 105-112 (in Russian)
https://dx.doi.org/10.18565/aig.2024.23
Keywords
Cervical cancer and dysplasia of varying severity are among the most common diseases in women of reproductive age. Traditional approaches to treating early-stage cervical cancer and cervical dysplasia in women planning to become pregnant have been associated with reduced fertility and an increased risk of pregnancy complications [1]. However, with advancements in modern fertility preservation, it is now possible to achieve satisfactory reproductive and obstetric outcomes in women undergoing treatment for cervical cancer and cervical dysplasia. Nevertheless, careful monitoring of pregnancies in these patients is recommended because of their higher risk compared with the general population [2, 3].
Various excision methods, such as conization, loop electrosurgical excision procedure (LEEP excision), Large Loop Excision of the Transformation Zone (LLETZ excision), and Excision of the Transformation Zone with a NETZ needle (needle versus loop diathermy excision of the transformation zone), are used to treat cervical precancerous lesions [4]. All interventions are performed using various energies. In recent years, high-frequency radiowave excision using a large loop or cone-shaped electrode produced by Fotek LLC (Yekaterinburg, Russia) has become the preferred method for treating cervical diseases. This radiowave treatment modality is known to be safe and allows for precise removal of the affected area with minimal thermal damage to the surrounding tissue, thereby improving repair and preserving women's reproductive function [5, 6].
Previously, aggressive diagnostic and treatment strategies were used when cervical intraepithelial neoplasia (CIN) II or III was detected in pregnant women. However, conservative approaches are now preferred. Simultaneously, the European Society of Medical Oncology (ESMO, 2009) considers excisional biopsy a safe method of investigation [7]. Cervical conization has been shown to result in positive pregnancy outcomes and a reduced risk of preterm birth. While some studies suggest that excision may increase the risk of preterm birth, others have reported no significant adverse effects. The American Association of Colposcopy and Cervical Pathology (2011) recommends close monitoring for young pregnant women with CIN II–III, and only considers excision if cervical cancer is suspected. Russian authors suggest targeted biopsy or conization if CIN II–III are found in smears [8].
As can be seen from the above information, there are significant differences in diagnostic and therapeutic approaches between domestic and foreign clinicians when it comes to cervical precancer in pregnant women [9, 10]. Women with CIN are already at a higher risk of prematurity, and excision and ablative treatments further increase this risk. The incidence and severity of adverse effects are higher with deeper cones and excision rather than ablation [1, 9].
Given the differences in approaches and importance of the topic, the objective of this study was to examine the impact of preconceptional cervical electroconization on the course of pregnancy and childbirth.
Materials and methods
We searched for and analyzed current studies investigating the effect of cervical conization on the reproductive ability of women of fertile age. The sources used were PubMed, eLibrary, and Cyberleninka. The search was performed using keywords from scientific publications from 2018 to 2023. A retrospective analysis of the course of pregnancy and birth outcomes of patients from two Yekaterinburg obstetric hospitals, including Yekaterinburg Clinical Perinatal Center and City Clinical Hospital No. 40, from 2018 to 2022 (5 years), was conducted.
Convenience sampling was used to form group 1 (n=50), which included patients who had undergone cervical surgery prior to pregnancy with electroconization for CIN II–III, 44/50 (88%), CIN I, 1/50 (2%), or cancer in situ, 5/50 (10%). Each patient with electroconization was matched with a patient without previous surgery who gave birth on the same day; age differences in the matched groups did not exceed three years. In two cases, the authors did not find patients comparable in age who gave birth at the same hospital on the same day. Thus, group 2 (n=48) included patients of comparable age from the same hospitals who had no history of cervical disease or cervical surgery. After cervical electroconization, women in group 1 became pregnant at an average of 2 years and 7 months. In both groups, patients whose pregnancies ended during delivery were included.
Cervical electroconization was performed with a sail electrode on the universal electrosurgical EHF devices of Fotek LLC (Yekaterinburg, Russia), which generates a broadband radio wave electrosurgical current of a special shape, in the monopolar «Mixture» (thin layer of coagulation) or «Mixture 1» (thick layer of coagulation) mode) at a power of 90–120 W (depending on the size of the electrode and the device unit). Small, medium, and large sail electrodes have the same length as the endocervical component but differ in the size of the removed exocervical component.
The authors assessed the following criteria for cervical electroconization during pregnancy and childbirth: the presence of cervical shortening as a result of surgery (risk of isthmic-cervical insufficiency) and scar tissue formation in the electroconization zone ( risk of cervical dystocia). Primary and secondary outcomes included the risk of preterm birth, complications during childbirth, dominant mode of delivery in the presence of a history of cervical electroconization, and connection between a history of cervical conization and fetal pathology. The primary outcomes included the characteristics of pregnancy (primarily isthmic-cervical insufficiency) and childbirth (percentage of preterm birth, cesarean section, and labor anomalies). Secondary outcomes included obstetric and gynecological history and fetal birth outcomes. All outcomes were assessed only by medical professionals and were long-term (several years after the intervention).
Statistical analysis
Statistical analysis was performed using descriptive statistical methods using Excel. The normality of the distribution was determined using Statistica 6.0, and was found to be normal. Continuous variables showing a normal distribution were expressed as mean (M) and standard deviation (SD) and presented as M (SD). The significance of differences was tested using Fisher's test; if p<0.05, the data were considered statistically significant. To assess the effect of cervical electroconization on the course of pregnancy and childbirth, the authors used correlation analysis was performed using Statistica 6.0. The presence and nature of the relationships were assessed using Pearson’s correlation coefficient. If the correlation coefficient is closer to 1, there is a strong correlation; if it is closer to 0, the correlation is weak or absent. When the correlation coefficient is equal to one, we can say of a functional relationship, that is, changes in two values can be described by a mathematical function.
Results
The mean age of patients in group 1 was 32.84 (4.2) years, and that of patients in group 2 was 32.48 (4.2) years (p>0.05). In the resulting samples, none of the women were under 18 or over 40 years of age. At the age of 18 to 29 years there were 11/50 (22%) patients in group 1, 12/48 (25%) in group 2; at the age of 30 to 39 years there were 38/50 (76%) in group 1, and 36/48 (75%) in group 2 (p>0.05).
The mean number of births for women in group 1 was 2.4 (1.76), and that of patients in group 2 was 2.29 (1.38) (p=0.09). The mean number of abortions among women in group 1 was 0.84 (1.48), and that of patients in group 2 was 0.73 (1.32) (p=0.43).
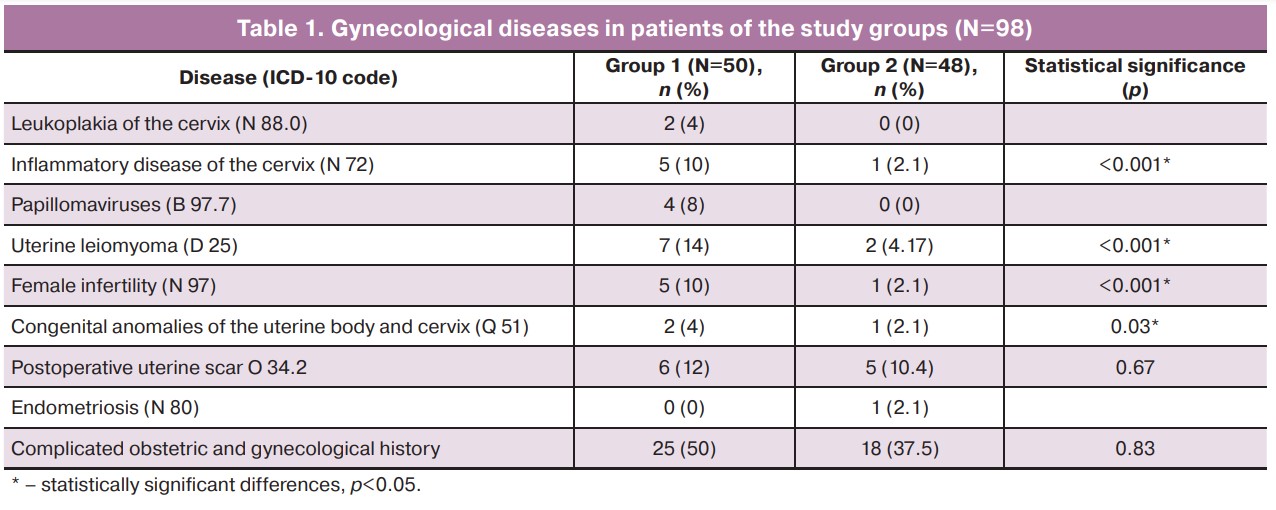
A comparative assessment of the structure of gynecological diseases among women in the study groups is presented in Table 1. We did not find significant differences in the frequency of detection of cervical leukoplakia, carriage of the highly oncogenic human papillomavirus (HPV), uterine scar, or endometriosis. In patients with a history of cervical electroconization, uterine fibroids were detected in 7/50 (14%) and in 2/48 (4.17 %) women without cervical electroconization (p<0.001). Infertility occurred in 5/50 (10%) patients in group 1 and in 1/48 (2.1%) patients in group 2 (p<0.05).
Congenital uterine malformations were detected in 2/50 (4%) patients in group 1 and in 1/48 (2.1%) patient in group 2 (p=0.03). Complicated obstetric and gynecologic history was quite common in both groups: in 25/50 (50%) women in group 1 and in 18/48 (37.5%) women in group 2; however, there were no statistically significant differences (p=0.78). Cervicitis occurred in 5/50 (10%) women in group 1 and in 1/48 (2.1%) in group 2 (p<0.05).
The structure of obstetric pathology in group 1 included isthmic cervical insufficiency (ICI) in 5/50 (10%), preeclampsia in 0/50 (0%), uterine scar in 4/50 (8%), HELLP syndrome in 0/50 (0%), placenta previa, and multiple gestation in 0/50 (0%) patients. In group 2, ICI was observed less frequently in 2/48 (4.2%) women (p=0.034), pre-eclampsia in 5/48 (10.4%) (p<0.05), uterine scar in 5/48 (10.4%) (p>0.05), HELLP syndrome, placenta previa, and multiple pregnancies in 1/48 (2.1%) of each nosological form (p>0.05). Patients in both groups had somatic pathologies. Women who underwent cervical electroconization before pregnancy were significantly more likely to be diagnosed with diseases of the skin and subcutaneous tissue (ICD-10 code L00-L99), 2/50 (4%); acute respiratory infections of the upper respiratory tract (J00-J06) during pregnancy, 4/50 (8%); diseases of the digestive system (K00-K93), 16/50 (32%); diseases of the nervous system (G00-G99), 7/50 (14%); diseases of the circulatory system ( I00-I99) and diseases characterized by high blood pressure (I10-I15), 17/50 (34%), viral hepatitis (B15-B19), and 4/50 (8%) (p<0.05). In group 1, Rh-negative blood without antibody titer was found in 3/50 (6%) patients and in 1/48 (2.1%) patients in group 2 (p<0.001) (Table 2).
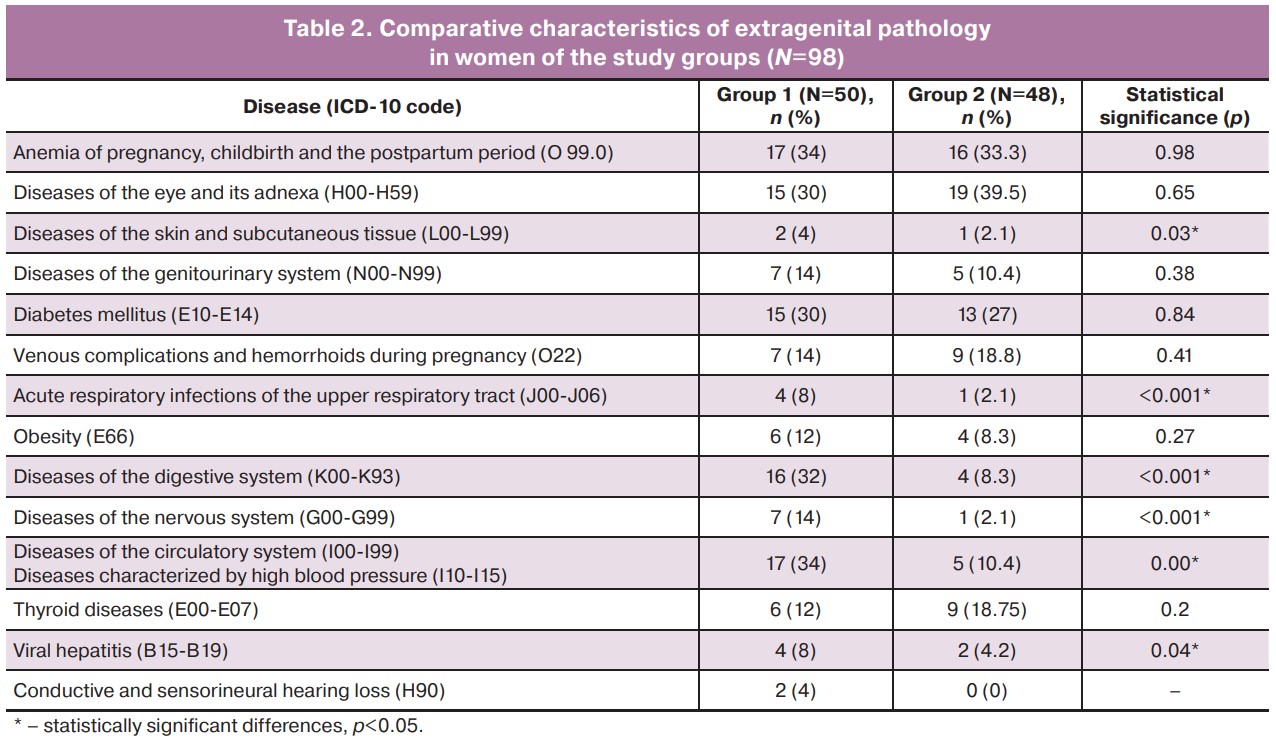
It should be noted that in group 1, extragenital diseases in women were more common and affected different systems and organs (Table 1). In group 2, only diseases of the eye and its adnexa were more common (H00-H59 – ICD-10 code) in 19/48 (39.5%) and venous complications and hemorrhoids during pregnancy (O22) in 9/48 (18.8%) patients (p>0.05).
There were no statistically significant differences in the rate of natural birth (46 and 46.7%, respectively), cesarean section (32 and 33.3%, respectively), and term birth (96 and 97.9%, respectively) between the two groups (p>0.05). The incidence of preterm birth was higher among women with a history of cervical electroconization (2/50, 4%) than among those in group 2 (1/48, 2.1%) (p=0.03).
Premature rupture of membranes occurred only in women in group 1 (2/50, 2%). In these patients, perineal lacerations during childbirth occurred in 17/50 (34%) cases and vaginal lacerations occurred in 1/50 (2%) patient. There were no cervical lacerations in any of the women; amniotomy was used in 10/50 (20%) cases and a Foley catheter was used for labor induction in 1/50 (2%) patients. Overall, the rate of labor induction was 11/50 (22%), suture removal from the cervix was performed in only 1/50 (2%) women, and vascular ligation to stop bleeding during labor was performed in 2/50 (4%) patients.
In group 2, perineal rupture occurred in 16/48 (33.3%) cases, vaginal rupture in 3/48 (6.25%), cervical rupture in 2/48 (4.2%), amniotomy in 5/48 (10.4%), and ligation of vessels for hemostatic purposes in 3/48 (6.25%).
Thus, the authors found statistically significant differences in the incidence of vaginal lacerations during labor (2 and 6.25%, respectively; p<0.001) and the frequency of labor induction during labor (22 and 10.4%, respectively; p=0.04). At the same time, the authors did not find significant differences in the frequency of labor augmentation with oxytocin in the study groups (11/50 (22%) and 14/48 (29.2%), respectively (p=0.80) or in the frequency of use of epidural anesthesia (11/50 (22%) and 11/48 (23%), respectively (p=0.40).
The blood loss volume during childbirth in patients of group 1 was 429.06 (352.6) ml, and 386.56 (229.9) ml in group 2 (p=0.004). Birth weight in group 1 was 3263 (486) g and 3122 (629) g in group 2 (p=0.08), birth body length in group 1 was 51 (2.9) cm and 51 (3.9) cm in group 2 (p=0.04), and Apgar score at 1/5 min in group 1 was 7.5/8.6, and 7.4/8.6, group 2 (p>0.05).
Correlation analysis showed a weak positive correlation between cervical electroconization before birth and the studied outcomes. In particular, the Pearson correlation coefficient between conization and preterm birth was 0.06 [95% CI: 0.9–-0.9], electroconization and ICI 0.14, electroconization and labor anomalies 0.16, electroconization and premature rupture of membranes 0.09, electroconization and birth weight 0.13, and electroconization and blood loss volume 0.07. A weak negative correlation was identified between electroconization and cesarean section, with a Pearson’s correlation coefficient of 0.01.
Discussion
Traditionally, the occurrence of precancerous cervical disease has been linked to HPV and other factors that contribute to its development [11–14]. However, our study showed that such patients have other features worthy of attention. In particular, women who have undergone electroconization for CIN II–III or more suffer from uterine fibroids and infertility and also have uterine malformations more often than women without a history of cervical pathology. Recent domestic studies have shown that women with uterine fibroids exhibit significant progesterone dysfunctions. It can increase the frequency of somatic mutations in myometrial cells, promote the development of uterine fibroids, and participate in hormone-mediated stimulation of fibroid growth. In addition, increased expression of apoptosis inhibitors, including the proto-oncogene bcl-2 and the cell proliferation regulator Ki-67 was also noted in leiomyoma nodules [15]. As we know, the level of Ki-67 expression is highest in patients with a high rate of progression of locally advanced forms of cervical cancer, so the presence of uterine fibroids at a young age can also be considered as a risk factor for precancerous cervical diseases in women with HPV [16].
The International Cancer Research Foundation suggests that body weight, nutrition, and physical activity can be the basis for cancer prevention in various locations [17]. Our study noted a high percentage of gastrointestinal diseases, particularly viral hepatitis, in women who underwent cervical electroconization, which may confirm data on the influence of diet on the development of neoplasia.
Diseases associated with the circulatory system occur 3 times more often in patients after cervical electroconization than in women with a healthy cervix. The authors can also assume that changes in the blood supply to the uterus and cervix are an additional criterion for the diagnosis of precancerous diseases, as described in a study by Lapochkina N.P. [18]. It remains unclear what is primary – microcirculation disorder or neoplasia. Further research in this direction is required [19]. Probably because of the presence of arterial hypertension before pregnancy, patients in group 1 received antihypertensive drugs during pregnancy from early pregnancy and acetylsalicylic acid as prophylaxis (because they were at high risk of preeclampsia). The authors' study showed that such prevention was effective: preeclampsia occurred in 0% of patients in group 1 and in 10.4% of patients in group 2. Interestingly, there is a high incidence of nervous system diseases in women with precancerous lesions of the cervix, and electroconization is often performed in patients with negative blood Rh factor. To date, the literature contains only data on the presence of psychological maladjustment in patients with cervical pathology in comparison with healthy women, but there is practically no data on the incidence of diseases of the nervous system [20].
The study did not find an increase in the number of cesarean sections performed in patients with a history of cervical electroconization. The results showed a statistically significant increase in the number of preterm births and use of ICI. In this case, correction of ICI was carried out mainly by intravaginal administration of progesterone preparations; an obstetric pessary and cervical suture were practically not used (only in one patient).
Patients with a history of cervical electroconization require labor induction. This may be due to a combination of factors, including disturbances in neuroendocrine regulation (gynecological pathology, a high percentage of diseases of the nervous system) and a mechanical factor (part of the tissue has been removed, and therefore, the receptors that take part in the initiation of labor). The need for labor augmentation with oxytocin is the same as that in healthy women. In this regard, we suggest that conservative therapy may be justified and effective in women with a history of cervical electroconization.
A history of cervical electroconization was not associated with the percentage of perineal lacerations or cervical dystocia during childbirth; these women did not have a cervical laceration. However, the percentage of vaginal lacerations was slightly higher than that in the healthy women. However, the authors are currently unable to explain this phenomenon. Most studies show that labor anomalies are often a multifactorial problem; the isolated effect of cervical electroconization is negligible and insignificant [21].
The blood loss volume in women who underwent cervical electroconization was significantly greater than that in patients in group 2. This may be due to a high percentage of cardiovascular diseases as well as other factors. An analysis of the literature shows that the diagnosis and prevention of massive bleeding during childbirth and the postpartum period are extremely complex and difficult tasks [22, 23].
Conclusion
Pregnant women with a history of cervical electroconization are at higher risk of developing cardiovascular, digestive, and nervous system diseases. In terms of gynecological issues, these patients may have uterine fibroids, infertility, and congenital malformations of the genital organs. It is more common for women who underwent electroconization to experience ICI. However, this can be managed by prescribing progesterone drugs, and the need for sutures or pessaries is minimal. The risk of preterm birth is higher in women who have undergone cervical electroconization than in those who have not. During labor, patients with a history of cervical electroconization may require labor induction and may experience increased blood loss. It should be noted that there was no increase in the frequency of cesarean sections or the need for labor augmentation with oxytocin in women who had undergone cervical electroconization. Furthermore, no negative effects on the fetus were observed.
References
- Kyrgiou M., Athanasiou A., Paraskevaidi M., Mitra A., Kalliala I., Martin-Hirsch P. et al. Adverse obstetric outcomes after local treatment for cervical preinvasive and early invasive disease according to cone depth: systematic review and meta-analysis. BMJ. 2016; 354: i3633. https://dx.doi.org/10.1136/bmj.i3633.
- Фириченко С.В., Манухин И.Б., Микаилова Л.У., Мынбаев О.А. Удаленная доля шейки матки и риск преждевременных родов. I Национальный конгресс «Онкология репродуктивных органов: от профилактики и раннего выявления к эффективному лечению», 19-21 мая 2016 года, Москва. Исследования и практика в медицине. 2016; Спецвыпуск: 178. [Firichenko S.V., Manukhin I.B., Mikailova L.U., Mynbayev O.A. Resection of lobe of the cervix and risk of preterm birth. The Ist National Congress "Oncology of reproductive organs: from prevention and early detection to effective treatment", May 19-21, 2016, Moscow. Research’n Practical Medicine Journal. 2016; (Special Issue): 178. (in Russian)].
- Yu X., Qie M., Huang L., Hou M. Successful pregnancy in a female with embryonal rhabdomyosarcoma of the cervix who received biopsy and chemotherapy alone without recurrence after 16 years: a case report and literature review. BMC Womens Health. 2023; 23(1): 466. https://dx.doi.org/10.1186/s12905-023-02623-6.
- Министерство здравоохранения Российской Федерации. Клинические рекомендации. Цервикальная интраэпителиальная неоплазия, эрозия и эктропион шейки матки. 2020. 59 c. [Ministry of Health of the Russian Federation. Clinical guidelines. Cervical intraepithelial neoplasia, erosion and ectropion of the cervix. 2020. 59 p. (in Russian)].
- Ильина И.Ю., Доброхотова Ю.Э. Совершенствование методов хирургического лечения патологии шейки матки. РМЖ. Мать и дитя. 2022; 5(3): 188-93. [Il’ina I.Yu., Dobrokhotova Yu.E. Optimizing surgical management of uterine cervix disorders. Russian Journal of Woman and Child Health. 2022; 5(3): 188-93 (in Russian)]. https://dx.doi.org/10.32364/2618-8430-2022-5-3-188-193.
- Паяниди Ю.Г., Боровкова Е.И., Доброхотова Ю.Э., Арутюнян А.М. Тактика ведения беременных с инвазивным раком шейки матки. РМЖ. Мать и дитя. 2019; 2(2): 135-8. [Payanidi Yu.G., Borovkova E.I., Dobrohotova Yu.E., Arutunyan A.M. Managing invasive cervical cancer in pregnancy. Russian Journal of Woman and Child Health. 2019; 2(2): 135-8. (in Russian)]. https://dx.doi.org/10.32364/2618-8430-2019-2-2-135-138.
- Бебнева Т.Н., Покуль Л.В. Современные аспекты дифференциального подхода к ведению беременных, отягощенных цервикальными интраэпителиальными неоплазиями. Трудный пациент. 2018; 16(1-2): 22-7. [Bebneva T.N., Pokul L.V. Modern aspects of the differential approach to the management of pregnant women with cervical intraepithelial neoplasias. Difficult Patient. 2018; 16(1-2): 22-7. (in Russian)].
- Кузнецова А.И., Петров Ю.А., Ермолова Н.В. Беременность и рак шейки матки. Главный врач Юга России. 2022; 2(83): 25-8. [Kuznetsova A.I., Petrov Yu.A., Ermolova N.V. Pregnancy and cervical cancer. Chief Physician of the South of Russia. 2022; 2(83): 25-8. (in Russian)].
- Rey Valzacchi G.M., Odetto D., Saadi J.M., Zamora L.B., Loza C., Medina M. et al. Conservative treatment of cervical cancer: A single center experience over a two-decade period. Gynecol. Oncol. Rep. 2023; 48: 101226. https://dx.doi.org/10.1016/j.gore.2023.101226.
- Kacerovsky M., Musilova I., Baresova S., Kolarova K., Matulova J., Wiik J. et al. Cervical excisional treatment increases the risk of intraamniotic infection in subsequent pregnancy complicated by preterm prelabor rupture of membranes. Am. J. Obstet. Gynecol. 2023; 229(1): 51.e1-51.e13. https://dx.doi.org/10.1016/j.ajog.2022.12.316.
- Han L., Chen Y., Zheng A., Chen H. Effect of preoperative cervical conization before hysterectomy on survival and recurrence of patients with cervical cancer: A systematic review and meta-analysis. Gynecol. Oncol. 2023; 174: 167-74. https://dx.doi.org/10.1016/j.ygyno.2023.05.004.
- Terzic M., Makhadiyeva D., Bila J., Andjic M., Dotlic J., Aimagambetova G. et al. Reproductive and obstetric outcomes after fertility-sparing treatments for cervical cancer: current approach and future directions. J. Clin. Med. 2023; 12(7): 2614. https://dx.doi.org/10.3390/jcm12072614.
- Hashiramoto S., Kinjo T., Tanaka S.E., Arai W., Shimada M., Ashikawa K. et al. Vaginal microbiota and pregnancy outcomes of patients with conization histories. J. Womens Health (Larchmt). 2023; 32(3): 375-84. https://dx.doi.org/10.1089/jwh.2022.0440.
- Коган Е.А., Файзулина Н.М., Исраилова А.Х., Козаченко А.В., Демура Т.А., Темишева Я.А., Екимов А.Н., Донников А.Е. Мониторинг больных, перенесших операцию конизации шейки матки по поводу цервикальной интраэпителиальной неоплазии (клинико-морфологические и молекулярно-биологические аспекты проблемы). Акушерство и гинекология. 2012; 1: 70-4. [Kogan E.A., Faizulina N.M., Israilova A.Kh., Kozachenko A.V., Demura T.A., Temisheva Ya.A., Ekimov A.N., Donnikov A.E. Monitoring patients undergoing conization of the cervix uteri for cervical intraepithelial neoplasia: Clinical, morphological, and molecular biological aspects. Obstetrics and Gynecology. 2012; (1): 70-4. (in Russian)].
- Аганезова Н.В., Аганезов С.С., Шило М.М. Миома матки: современные практические аспекты заболевания. Проблемы репродукции. 2022; 28(4): 97‑105. [Aganezova N.V., Aganezov S.S., Shilo M.M. Uterine fibroids: modern practical aspects of the disease. Russian Journal of Human Reproduction. 2022; 28(4): 97-105. (in Russian)]. https://dx.doi.org/10.17116/repro20222804197.
- Чуруксаева О.Н., Коломиец Л.А., Савенкова О.В., Недосеков В.В., Ибрагимова М.К. Прогностическое значение Ki67, циклооксигеназы-2 (COX-2) и p16ink4a у больных местнораспространенным раком шейки матки. Сибирский онкологический журнал. 2016; 15(5): 25-32. [Churuksaeva O.N., Kolomiets L.A., Savenkova O.V., Nedosekov V.V., Ibragimova M.K. Prognostic significance of Ki67, cyclooxygenase-2 (COX-2) and p16ink4a in patients with locally advanced cervical cancer. Siberian Journal of Oncology. 2016; 15(5): 25-32. (in Russian)]. https://dx.doi.org/10.21294/1814-4861-2016-15-5-25-32.
- Hermans K.E.P.E., van den Brandt P.A., Loef C., Jansen R.L.H., Schouten L.J. Adherence to the World Cancer Research Fund and the American Institute for Cancer Research lifestyle recommendations for cancer prevention and cancer of unknown primary risk. Clin. Nutr. 2022; 41(2): 526-35. https://dx.doi.org/10.1016/j.clnu.2021.12.038.
- Лапочкина Н.П., Джалалова П.М., Ротару Т.В. Изменения микроциркуляции слизистой оболочки шейки матки при предраковых заболеваниях. Вестник ИвГМА. 2021; 26(1): 40-3. [Lapochkina N.P., Jalalova P.M., Rotaru T.V. Microcirculation alterations in cervical mucosa in precancerous diseases. Bulletin of Ivanovo State Medical Academy. 2021; 26(1): 40-3. (in Russian)]. https://dx.doi.org/10.52246/1606-8157_2021_26_1_40.
- Никитаева А.П., Росюк Е.А., Вишнева Е.М. Влияние гестационной артериальной гипертензии на течение беременности и развитие осложнений со стороны матери и плода. Современные проблемы науки и образования. 2023; 4: 118-20. [Nikitaeva A.P., Rosyuk E.A., Vishneva E.M. The effect of gestational hypertension on the course of pregnancy and the development of maternal and fetal complications. Modern Problems of Science and Education. 2023; (4): 118-20. (in Russian)]. https://dx.doi.org/10.17513/spno.32862.
- Кононова И.Н., Рогачева Т.В. Проблема клинико-психологического сопровождения пациенток с патологией шейки матки. Медицинская психология в России. 2015; 1(30): 10. [Kononova I.N., Rogacheva T.V. The issue of the clinical and psychological support of patients with cervical pathology. Medical psychology in Russia. 2015; 1(30): 10. (in Russian)].
- Мочалова М.Н., Рындин В.И., Мудров В.А. Последствия травмы шейки матки как медицинская и социальная проблема. Российский вестник акушера-гинеколога. 2022; 22(6): 35‑41. [Mochalova M.N., Ryndin V.I., Mudrov V.A. Consequences of cervical trauma as a medical and social problem. Russian Bulletin of Obstetrician-Gynecologist. 2022; 22(6): 35 41. (in Russian)]. https://dx.doi.org/10.17116/rosakush20222206135.
- Зиганшин А.М., Кулавский В.А., Нагимова Э.М., Шакиров А.Р., Адигамова Г.С. Материнская смертность от послеродовых кровотечений. Медицинский вестник Башкортостана. 2019; 6(84): 53-7. [Ziganshin A.M., Kulavskiy V.A., Nagimova E.M., Shakirov A.R., Adigamova G.S. Maternal mortality from postpartum haemorrhage. Bashkortostan Medical Journal. 2019; 14(6): 53-7. (in Russian)].
- Бебнева Т.Н., Ковалев В.В., Лаврентьева И.В., Исламиди Д.К. Особенности структуры патологии шейки матки у беременных женщин. Уральский медицинский журнал. 2018; (13): 18-21. [Bebneva T.N., Kovaliov V.V., Lavrentieva I.V., Islamidi D.K. Features of the structure of the cervix pathology in pregnant women. Ural Medical Journal. 2018; (13): 18-21. (in Russian)]. https://dx.doi.org/10.25694/URMJ.2018.13.41.
Received 01.02.2024
Accepted 27.05.2024
About the Authors
Elena A. Rosyuk, PhD, Associate Professor, Department of Obstetrics and Gynecology, Ural State Medical University, Ministry of Health of Russia,620028, Russia, Yekaterinburg, Repina str., 3, +7(902)26-56-385, elenakdc@yandex.ru, https://orcid.org/0000-0003-1303-3955
Tatyana A. Oboskalova, Dr. Med. Sci., Professor, Head of the Department of Obstetrics and Gynecology, Ural State Medical University, Ministry of Health of Russia,
620028, Russia, Yekaterinburg, Repina str., 3, +7(912)28-37-631, oboskalova.tat@yandex.ru, https://orcid.org/ 0000-0003-0711-7896
Elena S. Emelyanova, student of the Faculty of Medicine and Prevention, Ural State Medical University, Ministry of Health of Russia, 620028, Russia, Yekaterinburg,
Repina str., 3, +7 (912) 628-76-32, lena.emelyanova2001@gmail.com
Natalya V. Butorina, student of the Faculty of Medicine and Prevention, Ural State Medical University, Ministry of Health of Russia, 620028, Russia, Yekaterinburg,
Repina str., 3.
Tatyana G. Emelyanova, Head of Women’s Consultation No. 1, Central City Clinical Hospital No. 6, 620144, Russia, Yekaterinburg, March 8 str., 126, + 7(982)62-70-745, lena.emelyanova2001@gmail.com
Evgeny Yu. Glukhov, Dr. Med. Sci., Professor at the Department of Obstetrics and Gynecology, Ural State Medical University, Ministry of Health of Russia,
620028, Russia, Yekaterinburg, Repina str., 3, + 7(922)22-41-411, dok@gynclinic.ru
Ekaterina I. Neff, PhD, Deputy Chief Physician, Gynecological Center «Women’s Clinic,» 620078, Russia, Yekaterinburg, Mira str., 44 B, +7(912)68-53-332, neff@gynclinic.ru
Alexander M. Yakushev, PhD, Associate Professor at the Department of Obstetrics and Gynecology, Ural State Medical University, Ministry of Health of Russia,
620028, Russia, Yekaterinburg, Repina str., 3, +7(902)87-60-683.