The impact of COVID-19 on the ovarian reserve in women
Objective: To investigate ovarian reserve and menstrual function in women with COVID-19 of various severity. Materials and methods: This prospective study analyzed parameters of ovarian reserve (AMH, FSH, and the AFC) and menstrual cycle (cycle length, menstrual duration) in 41 patients before and after COVID-19 disease. The interval between measurements was 6–12 months. Mild and moderate COVID-19 was observed in 31 (group 1) and 10 (group 2) patients. The inclusion criteria were age 18–45 years, preserved menstrual function. Non-inclusion criteria were decreased ovarian reserve before the onset of COVID-19 (AMH<1.2 ng/mL, AFC<5), a history of COVID-19 vaccination, pregnancy and lactation, severe somatic and infectious comorbidities affecting ovarian reserve. Results: In patients of late reproductive age (LRA) (>35 years), COVID-19 was associated with a reduction in ovarian reserve. Furthermore, patients with more severe COVID-19 had a more pronounced decrease in AFC. When simultaneously assessing the effect of infection severity and age on ovarian reserve, it was found that LRA patients with a more severe form of infection had the biggest decrease in ovarian reserve. The menstrual cycle did not change significantly. Conclusion: The study findings reflect the impact of both age and severity of COVID-19 on ovarian reserve in women. In women of LRA, a decrease in ovarian reserve can occur spontaneously, and the time difference can be very significant. Therefore, one cannot accurately state that ovarian reserve reduction was due to the disease. Nevertheless, the effect of infection severity on the degree of ovarian reserve reduction suggests an adverse effect of SARS-CoV-2 on ovarian function in women.Ermakova D.M., Dolgushin G.O., Ivanets T.Yu., Vtorushina V.V., Dolgushina N.V.
Keywords
The current literature is lacking sufficient coverage of the evidence regarding damage to the female reproductive system resulting from SARS-CoV-2 infection. According to the GeneCards database, expression of the major SARS-CoV-2 receptor proteins is detected in granulosa cells at all stages of follicle development, surface ovarian epithelium, as well as in theca and corpus luteum granulosa cells, which include ACE2, TMPRSS2 and basigin (CD147), suggesting that SARS-CoV-2 can penetrate into a woman's body by this route and influence folliculogenesis [1]. SARS-CoV-2 can probably penetrate ovarian tissue and oocytes by interacting with these receptors, leading to their damage [2]. There have been sporadic studies that have investigated the effects of COVID-19 on the female reproductive system, but their results were uncertain [3–6]. There are also very few studies on the detection of SARS-CoV-2 in female reproductive secretions or in products of conception [7-10]. Taking into account the non-declining COVID-19 incidence and the emergence of new strains of the infection, the study of SARS-CoV-2 effect on reproductive potential in women seems to be an urgent task.
The present study aimed to investigate ovarian reserve and menstrual function in women with COVID-19 of various severity.
Materials and methods
This prospective study was conducted at the Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia. The study analyzed the parameters of the ovarian reserve (AMH, FSH, and AFC) and menstrual cycle (cycle length, menstrual duration) in 41 patients before and after COVID-19 disease. All patients provided their informed consent to participate in the study. The interval between measurements was 6–12 months. Mild and moderate COVID-19 was observed in 31 (group 1) and 10 (group 2) patients.
Inclusion criteria were age 18 to 45 years, preserved menstrual function, presence of data on hormonal status (anti-Mullerian hormone (AMH), follicle stimulating hormone (FSH) and antral follicle count (AFC) prior to disease onset (not more than 6 months before the disease onset). Exclusion criteria were decreased ovarian reserve before the onset of COVID-19 (AMH<1.2 ng/mL, AFC<5), a history of COVID-19 vaccination, pregnancy and lactation, severe somatic and infectious comorbidities affecting ovarian reserve.
Data on COVID-19 were obtained from patient medical records, confirmed by information entered into the USHIS, and by determination of serum IgG antibodies against SARS-CoV-2 above the positivity index (PI). The criterion for mild COVID-19 was a subfebrile temperature (<38°C) in the absence of clinical manifestations of a moderate course of infection. The criteria for moderate COVID-19 included a temperature above 38°C, exertion dyspnea, signs of pneumonia with minimal or moderate lung involvement (CT 1–2), and the absence of clinical manifestations of severe SARS-CoV-2 infection [11].
The analysis of serum samples to determine FSH and AMH levels was performed by electro chemiluminescent method on days 2–5 of the menstrual cycle, performed on a Cobas e411 automatic immunochemical analyzer (Roche Diagnostics GmbH, Germany), using commercial kits of this manufacturer.
Endometrial thickness and structural characteristics, ovarian volume, and AFC were assessed by ultrasound on days 5–8 of the menstrual cycle.
Antibodies to SARS-CoV-2 in serum samples were determined using the "Reagent kit for detection of class G antibodies to spike protein SARS-CoV-2 by enzyme immunoassay" ("DS-IFA-ANTI-SARS-CoV-2-G(S)", produced by RPC Diagnostic Systems (Russia) for qualitative detection of antibodies in human blood serum (plasma) by enzyme immunoassay (EIA). The result of the analysis was evaluated by the PI value calculated by the formula: PI=OD of the sample/cutoff, where OD of sample is the optical density of the sample. The result was considered positive with PI>1.2, negative with PI <0.8, and equivocal with PI from 0.8 to 1.2.
Statistical analysis
Statistical analysis was performed using Statistica 10 (USA) software. Categorical variables were presented as counts and percentages. Categorical variables were compared by the χ2 test. McNemar’s test was used to compare the proportions among the paired samples. The distribution of continuous variables was tested for normality using the Kolmogorov-Smirnov test and graphical analysis of the data. It was found that numerical variables were not normally distributed and they were reported as the median (Me) and interquartile range (Q1; Q3). The groups were compared using nonparametric Sign test for paired samples and Mann–Whitney test for unpaired samples. The Spearman correlation coefficient was calculated to assess the correlation between the variables. Differences between groups were considered statistically significant at p<0.05.
Results
Patients with a history of more severe COVID-19 were older [42 (35–44) years] than patients in group1 [32 (27–41) years] (p=0.038). The morbidity of the patients was low considering their young age. The dynamics of the parameters characterizing the patients' ovarian reserve and menstrual function are summarized in Table.
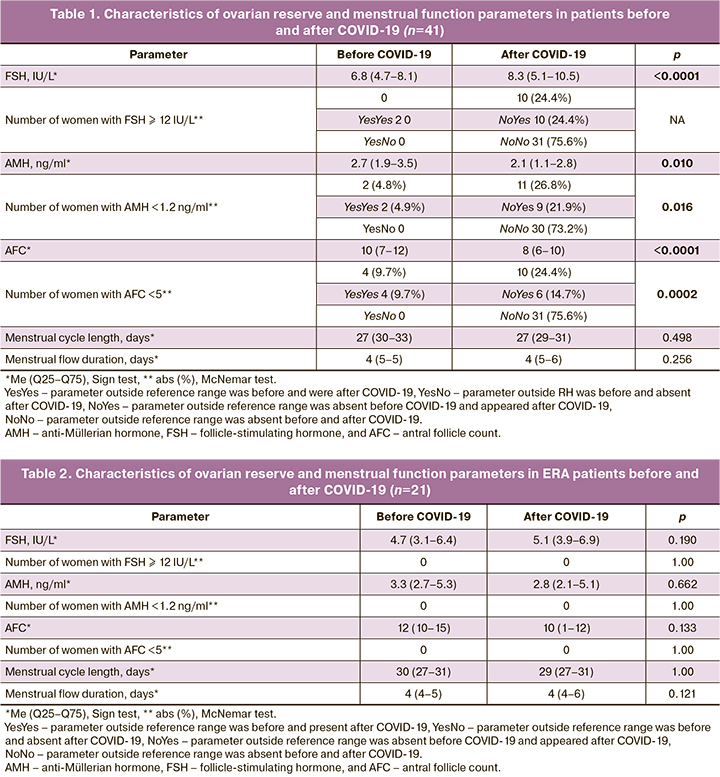
The evaluation was then performed for patients of early (≤35 years, n=21) (ERA) and late (>35 years, n=20) reproductive age (LRA) (Tables 2, 3).
No changes in the parameters of the menstrual cycle (menstrual cycle length, duration of menstrual flow) were observed in both in the subgroups of whole group and in the ERA and LRA patients. At the same time, a significant increase in the mean FSH level, a decrease of the AFC and AMH levels, a significant increase in the number of patients with elevated FSH levels, lower AFC and AMH levels above/below the normal ovarian reserve values were revealed in the whole group of women. Stratification of patients by age revealed that these changes were present only in the subgroup of patients of LRA. That is, after COVID-19, there was a decrease in ovarian reserve in patients of LRA.
The age of the patients significantly correlated with the parameters of the ovarian reserve as before the disease: FSH (r=0.7141, p<0.0001), AMH (r=-0.6424, p<0.0001), AFC (r=-0.7030, p<0.0001), and after disease: FSH (r=0.8495, p<0.0001), AMH (r=-0.7157, p<0.0001), AFC (r=-0.8013, p<0.0001). That is, the older the women, the higher were their FSH levels and the lower their AMH and AFC levels.
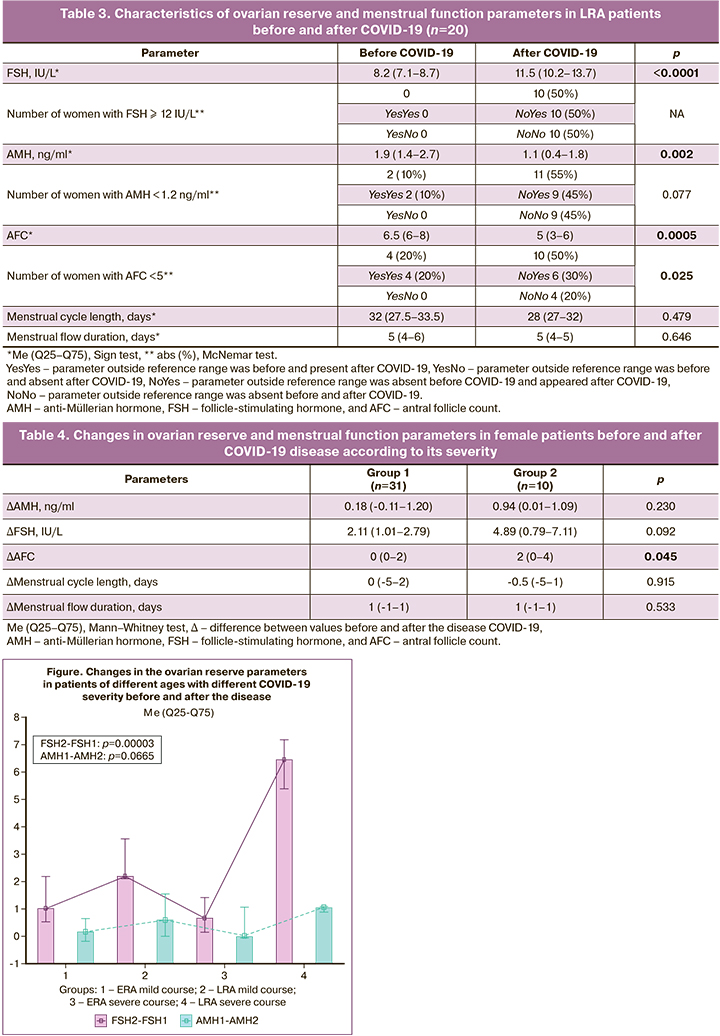
The deltas (Δ) of AMH, FSH and AFC were given. A positive Δ value always indicated a negative trend, e.g., ΔAMH=AMH1-AMH2, ΔFSH=FSH2-FSH1. Patients with more severe COVID-19 had a more pronounced decrease in AFC, while the menstrual cycle was unchanged (Table 4).
In a simultaneous evaluation of the effect of infection severity and age on ovarian reserve, the maximum decrease in ovarian reserve was observed in the LRA patients with more severe COVID-19. The menstrual cycle did not change significantly (Figure).
Discussion
Patients with a history of more severe COVID-19 were older. This is consistent with published research evidence. Therefore, age is a proven risk factor for disease severity [12].
There are few studies on the effect of COVID-19 on female reproductive system. In the study by Bentov Y. et al. no effect of infection on ovarian reserve and oocyte quality was observed in women undergoing ART [3]. The study of Wang M. et al. reported similar results [4]. Li K. et al. also showed no changes in the ovarian reserve after infection, but they noted changes in the menstrual cycle in the form of oligo or opsomenorrhea [5]. According to a study by Ding T. et al., patients with a history of COVID-19 had a decrease in ovarian reserve (decreased AMH levels), and this was most pronounced in LRA women [6]. Our data are consistent with the latter study. Patients of LRA were found to have significantly lower levels of AMH and AFC levels and higher FSH reflecting their ovarian reserve.
Conclusion
The study findings reflect the impact of both the age and severity of COVID-19 on ovarian reserve in women. In women of LRA, a decrease in ovarian reserve can occur spontaneously, and the time difference can be very significant. Therefore, one cannot accurately state that ovarian reserve reduction was due to the disease. Nevertheless, the effect of infection severity on the degree of ovarian reserve reduction suggests an adverse effect of SARS-CoV-2 on ovarian function in women.
References
- GeneCards: the human gene database. Available at: https://www.genecards.org/
- Долгушин Г.О., Романов А.Ю. Влияние SARS-COV-2 на репродукцию человека. Акушерство и гинекология. 2020; 11: 6-12. https://dx.doi.org/10.18565/aig.2020.11.6-12. [Dolgushin G.O., Romanov A.Yu. Effects of SARS-CoV-2 on human reproduction. Obstetrics and Gynecology. 2020; 11: 6-12. (in Russian)]. https://dx.doi.org/10.18565/aig.2020.11.6-12.
- Bentov Y., Beharier O., Moav-Zafrir A., Kabessa M., Godin M., Greenfield C.S. et al. Ovarian follicular function is not altered by SARS–CoV-2 infection or BNT162b2 mRNA COVID-19 vaccination. Hum. Reprod. 2021; 36(9): 2506-13. https://dx.doi.org/10.1093/humrep/deab182.
- Wang M., Yang Q., Ren X., Hu J., Li Z., Long R. et al. Investigating the impact of asymptomatic or mild SARS-CoV-2 infection on female fertility and in vitro fertilization outcomes: a retrospective cohort study. EClinicalMedicine. 2021; 38: 101013. https://dx.doi.org/10.1016/j.eclinm.2021.101013.
- Li K., Chen G., Hou H., Liao Q., Chen J., Bai H. et al. Analysis of sex hormones and menstruation in COVID-19 women of child-bearing age. Reprod. Biomed. Online. 2021; 42(1): 260-7. https://dx.doi.org/10.1016/j.rbmo.2020.09.020.
- Ding T., Wang T., Zhang J., Cui P., Chen Z., Zhou S. et al. Analysis of ovarian injury associated with COVID-19 disease in reproductive-aged women in Wuhan, China: an observational ssudy. Front. Med. (Lausanne). 2021; 8: 635255. https://dx.doi.org/10.3389/fmed.2021.635255.
- Cui P., Chen Z., Wang T., Dai J., Zhang J., Ding T. et al. Clinical features and sexual transmission potential of SARS-CoV-2 infected female patients: a descriptive study in Wuhan, China. medRxiv. February 2020. https://dx.doi.org/10.1101/2020.02.26.20028225.
- Scorzolini L., Corpolongo A., Castilletti C., Lalle E., Mariano A., Nicastri E. Comment of the potential risks of sexual and vertical transmission of Covid-19 infection. Clin. Infect. Dis. 2020; 71(16): 298. https://dx.doi.org/10.1093/cid/ciaa445.
- Demirel C., Tulek F., Celik H.G., Donmez E., Tuysuz G., Gökcan B. Failure to detect viral RNA in follicular eluid aspirates from a SARS-CoV-2-positive woman. Reprod. Sci. 2021; 28(8): 2144-6. https://dx.doi.org/10.1007/s43032-021-00502-9.
- Barragan M., Guillén J.J., Martin-Palomino N., Rodriguez A., Vassena R. Undetectable viral RNA in oocytes from SARS-CoV-2 positive women. Hum. Reprod. 2021; 36(2): 390-4. https://dx.doi.org/10.1093/humrep/deaa284.
- Временные методические рекомендации «Профилактика, диагностика и лечение новой коронавирусной инфекции (COVID-19)» Версия 7. 3 (утв. Министерством здравоохранения РФ 3 июня 2020 г.). Доступно по: https://base.garant.ru/74212510/ [Temporary guidelines “Prevention, diagnosis and treatment of new coronavirus infection (COVID-19)” Version 7 (approved by the Ministry of Health of the Russian Federation on June 3, 2020) (in Russian)]. Available at: https://base.garant.ru/74212510/
- Chen N., Zhou M., Dong X., Qu J., Gong F., Han Y. et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet. 2020; 395(10223): 507-13.https://dx.doi.org/10.1016/S0140-6736(20)30211-7.
Received 29.08.2022
Accepted 15.09.2022
About the Authors
Darya M. Ermakova, postgraduate student, Department of Assistive Technologies in Infertility Treatment, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Healthcare of the Russian Federation, daria.ermakova.97@bk.ru, https://orcid.org/0000-0002-8558-4687,117997, Russia, Moscow, Academician Oparin str., 4.
Grigory O. Dolgushin, resident of Faculty of Fundamental Medicine, Lomonosov Moscow State University, grdolgushin@yandex.ru, 117192, Russia, Moscow,
Lomonosovsky Prospekt, 31-5.
Tatyana Yu. Ivanets, Dr. Med. Sci., Head of the Clinical Diagnostic Laboratory, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Healthcare of the Russian Federation, t_ivanets@oparina4.ru, 117997, Russia, Moscow, Academician Oparin str., 4.
Valentina V. Vtorushina, PhD, Doctor of Clinical Laboratory Diagnostics,
Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Healthcare of the Russian Federation,
vtorushina@inbox.ru, 117997, Russia, Moscow, Academician Oparin str., 4.
Nataliya V. Dolgushina, Dr. Med. Sci., Professor, Deputy Director – Head of the Department for Scientific Projects Organization, Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Healthcare of the Russian Federation, n_dolgushina@oparina4.ru,
https://orcid.org/0000-0003-1116-138X, 117997, Russia, Moscow, Academician Oparin str., 4.
Authors' contributions: Ermakova D.M. – patient recruitment, manuscript drafting; Dolgushin G.O. – literature search, manuscript drafting; Ivanets T.Yu. – determination of AMH and FSH levels in the patients enrolled in the study;
Vtorushina V.V. – determination of IgG and IgM antibody levels to SARS-CoV-2; Dolgushina N.V. – planning the manuscript, reviewing and final approval of the article, statistical analysis.
Conflicts of interest: The authors have no conflicts of interest to declare.
Funding: This work was supported by the "Contribution to the Future" charitable foundation as part of the "Stop Coronavirus Together" campaign.
Ethical Approval: The study was reviewed and approved by the Research Ethics Committee of the V.I. Kulakov NMRC for OG&P.
Patient Consent for Publication: All patients provided informed consent for the publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available on request from the corresponding author after approval from the principal investigator.
For citation: Ermakova D.M., Dolgushin G.O., Ivanets T.Yu., Vtorushina V.V., Dolgushina N.V. The impact of COVID-19 on the ovarian reserve in women.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2022; 10: 123-128 (in Russian)
https://dx.doi.org/10.18565/aig.2022.10.123-128



