Validation of the Russian-language version of the questionnaire for assessing chronic constipation severity
Diagnosis of constipation severity and underlying pathophysiologic mechanisms, including in patients pelvic organ prolapse, is a challenging issue. However, validated and easy-to-use tools to guide constipation management are lacking. Objective: To validate a Russian-language version of the KESS questionnaire in patients with functional defecation disorders (FDD). Materials and methods: English version of the KESS questionnaire was translated and adapted. All patients in the study and control group underwent examination to exclude organic causes of constipation, as well as high-resolution anorectal manometry and X-ray defecography. The data obtained using the KESS questionnaire was compared with that using the previously registered questionnaire "The system of scoring of colon evacuation function disorders." Statistical analysis was performed using a nonparametric module of the SPSS (IBM, USA). Results: Data for the final analysis was available on 273 subjects (in 193 of them, FDD was confirmed by instrumental diagnostic investigations). The time to complete the KESS questionnaire was 3.5±0.76 minutes, the scores in the study and control groups were 18.4±3.1 and 2.7±0.9, respectively (p<0.001). The threshold score for differentiating patients with and without FDD was ≥10; diagnostic sensitivity was 100% [95% confidence interval (95% CI) 97–100%], diagnostic specificity was 100% [95% CI 71–100%]. The correlation of the results with the Scoring System was 0.748. No factors contributing to a possible decrease in the diagnostic value of the KESS questionnaire have been identified. Conclusion: The Russian-language version of the KESS questionnaire is a reliable tool for assessing constipation severity and making a differential diagnosis of the underlying pathophysiologic mechanisms.Fomenko O.Yu., Morozov S.V., Morozov D.A., Shkoda A.S., Poryadin G.V., Kashnikov V.N., Popov A.A., Fedorov A.A., Apolikhina I.A., Chuprynin V.D., Kozlov V.A., Belousova S.V., Pimenova E.S., Nekrasov M.A., Achkasov S.I.
Keywords
Validation of the Russian-language version of the KESS questionnaire
Chronic constipation is a disorder in the gastrointestinal tract characterized by infrequent stools, excessive straining, and abdominal pain during bowel movements, a feeling of incomplete emptying, hard stools, an increase in the time spent on the toilet (or unsuccessful defecation attempts), and the need for manual evacuation [1–5]. Chronic constipation affects 12–16% of the population in developed countries, has a significant impact on patients' quality of life, and causes a substantial increase in health care costs [1, 6]. Of particular interest due to diagnostic difficulty is constipation in patients with pelvic organ prolapse, especially posterior prolapse in the form of rectocele. This disorder disguises itself as a clinical picture of pelvic organ prolapse (excessive straining, manual evacuation, pain during bowel movements). After excluding organic causes, the most common causes of constipation are functional disorders associated with impaired bowel motility.
The primary pathophysiological mechanism underlying functional constipation is delayed colonic transit and/or impaired ability to satisfactorily evacuate the rectum due to pelvic dyssynergy [7–9]. The latter includes a paradoxical contraction or inadequate relaxation of the pelvic floor muscles during an attempt to defecate with or without insufficient propulsion of the contents. In some cases, a combination of several cologenic and proctogenic factors is possible [6, 10]. Both mechanisms of constipation are relevant for patients with internal genital organs prolapse, mainly for patients with posterior prolapse in the form of rectocele.
Although a practitioner has therapeutic armamentarium including a wide range of laxatives and physical treatments, the choice of pathogenetically relevant management strategy (laxatives, antispasmodics, biofeedback therapy, pelvic floor exercises, etc.) is still challenging [ 6, 10]. It requires the adequate diagnosis of factors that underlie the disease manifestations. International guidelines recommend a set of investigations including defecography or MR-defecography, anorectal manometry, balloon expulsion test, and assessment of colonic transit rate [7–9]. However, the entire range of these diagnostic modalities is available only in specialized centers. This dictates the need to introduce simple, affordable, and reliable methods that allow you to choose a treatment regimen based on understanding the pathophysiological mechanisms and the severity of manifestations in a particular patient. The only such tool validated in Russia is the “The scoring system for assessing colon evacuation disorders” [11, 12]. Despite the ease of use, this questionnaire does not fully meet modern requirements and is not used internationally. At the same time, Russian-language versions of internationally adopted diagnostic questionnaires, such as the Cleveland scale [13] or the Knowles-Eccersley-Scott-Symptom (KESS) questionnaire [14], have not been validated in our country. Moreover, the original KESS questionnaire authors showed the possibility of differential diagnosis of functional defecation disorders (FDD) using specially developed formulas, which may help a practitioner significantly simplify and streamline patients’ assessment.
In this regard, the present study aimed to validate a Russian-language version of the KESS questionnaire in patients with functional defecation disorders.
Materials and methods
The study was conducted at the Ryzhikh NMRC for Coloproctology of Minzdrav of Russia in 2018–2020 and included 273 patients with chronic constipation and rectocele, a type of pelvic organ prolapse. The grade of the rectocele was determined using an X-ray.
The study evaluated: 1) the feasibility of using the Russian-language version of the KESS questionnaire in patients with FDD, 2) the factors that potentially limit the feasibility of its use.
The criteria for inclusion in the study were the patient's desire to take part in the study, a signed informed consent; the presence of one of the variants of FDD syndrome per revised Rome IV criteria [7–9], confirmed by specialized investigations, including high-resolution anorectal manometry, evacuation test, and defecography. A study participant had to be fluent in Russian at a conversational level. The inclusion criteria for participants in the control group were the same, except FDD ruled out by similar specialized investigations. The exclusion criteria were organic causes of constipation (inflammatory bowel disease, cancer) according to colonoscopy, gastrointestinal surgery (except for a history of appendectomy and laparoscopic cholecystectomy more than one year before), taking medications that can lead to the development of constipation, severe comorbidities of any organs and systems, inability to read and understand the questionnaire. The final analysis did not include the data of patients who provided incomplete responses to the questionnaire and cases where diagnostic findings suggested by the study protocol were partially or entirely missing.
The Russian-language version of the KESS questionnaire
The English version of the KESS scale was provided by its authors (C. Knowles et al. [14]) upon request explaining the study's objective. The questionnaire was translated into Russian by two professional medical translators, native speakers of the Russian language, who worked independently of each other. Both translation options were discussed at a joint meeting of translators and the staff of the Clinical Pathophysiology Laboratory of the Ryzhikh NMRC for Coloproctology, Ministry of Health of Russia. In the course of the discussion, a version of the questionnaire was developed that most closely corresponded to the meaning of the original and linguistic norms. The Russian version was translated into English by a professional translation agency, and the translator was not familiar with the original version. The resulting double translation was approved by the authors of the original questionnaire. Thus, the official translation of the KESS questionnaire was made per the current recommendations of the World Health Organization [15]. The Russian-language version of the questionnaire is shown in Figure 1.
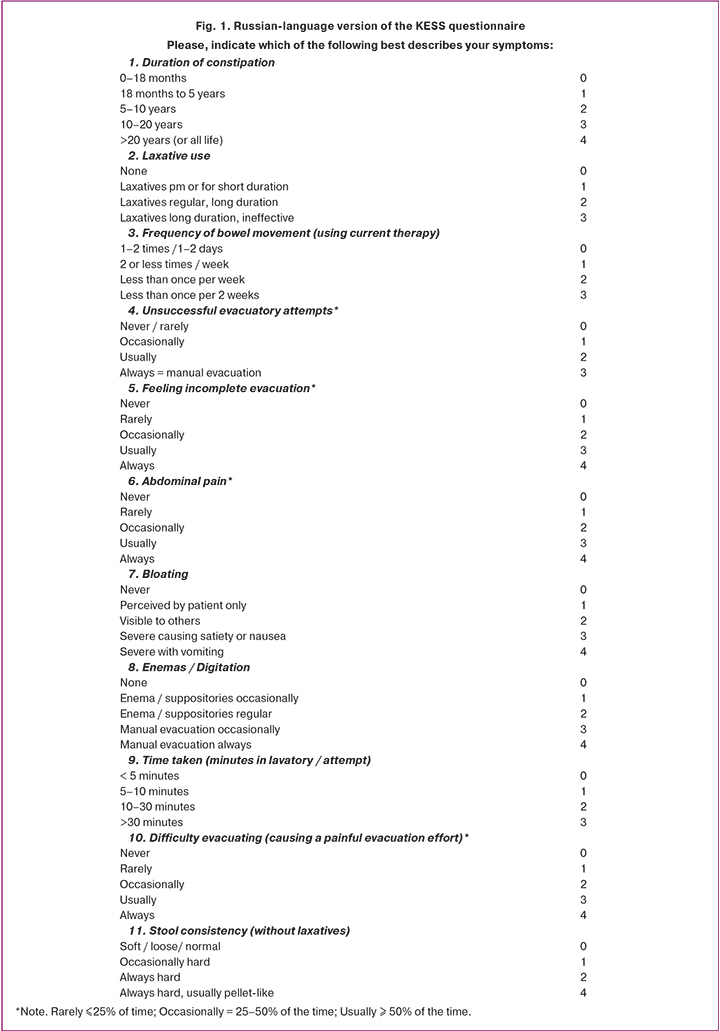
The KESS questionnaire is designed for self-completion by the patient and consists of 11 questions, each of which offers several response options with different score values. The total score is obtained by simple summation. A greater number of points determine a greater degree of manifestation. The questionnaire questions represent internationally agreed criteria for constipation [13, 16]. It is simple enough to be completed in under five minutes. Each question has four or five possible answers ranging between zero and three or zero and four points. The KESS score is the sum of all scores gained on individual questions with a maximum of 39 points. The answers to each question were worded such that any patient who fitted the agreed criteria for constipation would be likely to score at least one point per question [14].
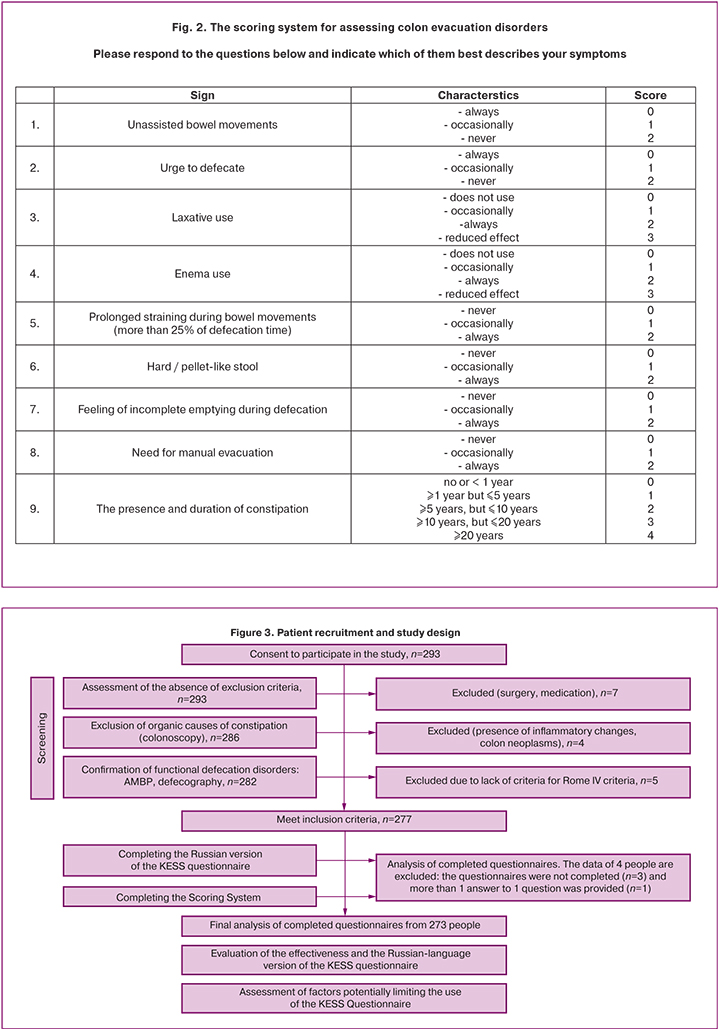
Scoring system for assessing colon evacuation disorders
The scoring system for assessing colon evacuation disorders of the Ryzhikh NMRC of Coloproctology of Minzdrav of Russia (from now on - the Scoring System) is a unified Russian-language questionnaire for evaluating defecation in patients with constipation [11]. For each of the nine questions included in the questionnaire, answer options are given, estimated in points. The maximum score is 22 points characterizing the most pronounced colon evacuation dysfunction (Fig. 2).
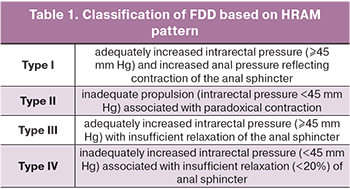
High-resolution anorectal manometry
The examination was conducted according to the standard technique (Head of the Laboratory of Clinical Pathophysiology of the Ryzhikh NMRC of Coloproctology, Dr. Med. Sci. O.Yu. Fomenko) using water perfused catheters for HRAM (Unisensor, Switzerland) and Solar GI software (Laborie, Netherlands). Evaluation of high-resolution anorectal manometry (HRAM) data was carried out following revised Rome IV revision criteria (Table 1) [6, 9, 17].
Defecography
The examination was conducted according to the standard method (the Head of the Department of Radiology of the Ryzhikh NMRC of Coloproctology, Dr. Med. Sci. I.V. Zarodnyuk). The rectocele grade was determined as follows: rectal protrusion measuring up to 2 cm was assessed as grade 1rectocele; from 2 to 4 cm as grade 2 rectocele, and over 4 cm as grade 3 rectocele. The size of the rectocele was measured as the distance between the extended longitudinal axis of the anal canal and the most protruding part of the protrusion [18]. Functional emptying disorders were confirmed by an increase in the residual rectal volume of more than 20% and an emptying time of more than 25 s [18].
Statistical analysis
Statistical analysis was performed using the SPSS IBM Statistics software (IBM, USA). Variables were compared with nonparametric methods. ROC curves were constructed to identify the threshold values for the presence of FDD by defining optimal values of sensitivity and specificity. The reliability of the KESS questionnaire was verified by assessing discriminant and convergent validity. The latter was determined by correlations between the final indicator of the KESS scale, on the one hand, and the Scoring System, on the other.
Patient recruitment and study design are shown in Figure 3.
Results
In total, data from 273 people were available for the final analysis. Of these, 193 patients with confirmed the FDD variants (93 women and 100 men, mean age 46.3±14.1) and 80 control subjects without constipation. The age of the controls was comparable to that in the study group (49.5±12.2, p>0.05). The groups did not differ in sex, with 48.2% and 53.8% of women in the study and control group, respectively, p=0.4.
Assessment of the diagnostic accuracy of the KESS questionnaire in FDD patients
On average, completing the Russian-language version of the KESS questionnaire took 3.5±0.76 minutes. The results obtained for the participants of both groups differed significantly: mean scores in the study and control group were 18.4±3.1 and 2.7±0.9, respectively (p<0.001).
The threshold score for distinguishing patients with and without FDD using the KESS questionnaire was≥10, the sensitivity was 100% [95% confidence interval (CI) 97–100%], and specificity was 100% [95% CI 71–100%].
Comparison of KESS questionnaire indicators with the results of a validated tool - the Scoring system questionnaire
The reliability of the KESS questionnaire was verified by assessing convergent validity. The latter was investigated using the method of correlation relationships between the final indicator of the KESS questionnaire, on the one hand, and the Scoring System, on the other. The mean score according to the Scoring System was 10.0±3.2. Using Spearman's rank correlation coefficient, the correlation coefficient between the indicators of the questionnaires was 0.748 (p<0.01), which indicated a strong correlation.
Analysis of factors potentially limiting the use of the questionnaire
Using the nonparametric (variables did not meet normality assumptions) Mann–Whitney U-test, we assessed the differences in the scores of the questionnaire between:
- men and women of the study group;
- patients over 65 and under this age;
- nulliparous and parous women;
- patients who have given birth to one and more than one child;
- patients with grade 1 and 2 rectocele versus grade 3 rectocele (Table 2).
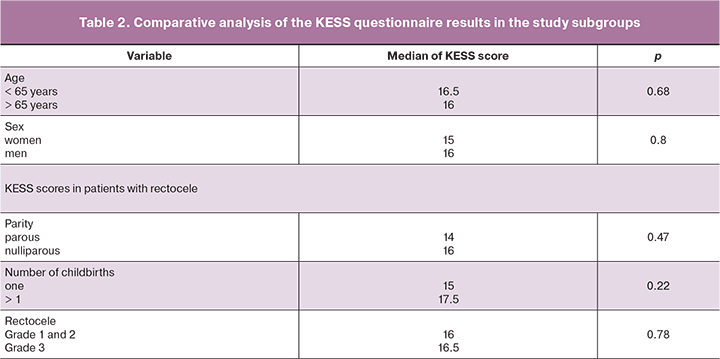
As a result, we found that, despite some differences in medians, in general, there were no significant differences between the KESS scores in patients depending on parity, age, and grade of rectocele. The KESS scores do not generally depend on the demographic characteristics of the patients and the grade of rectocele.
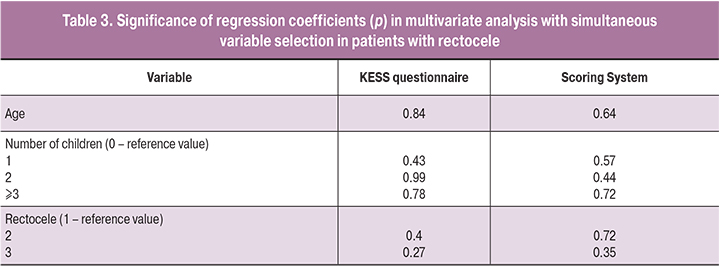
To identify the possibility of the influence of all these features on the KESS scores, we conducted a multivariate regression analysis using linear regression and robust standard errors.
As a result, we also did not reveal the influence of any characteristics of the patients on the questionnaires - both the Scoring System and KESS - all factors were also insignificant (Table 3).
Discussion
This study presents the Russian-language version of the KESS questionnaire and the results of assessing the feasibility of its use in patients with FDD. The choice of the KESS questionnaire (proposed by English researchers back in 2000) [14] is due to its simplicity and reliability and its increasing popularity in international practice as a method that can differentiate groups of patients with constipation based on the pathophysiological mechanisms underlying the symptom. The original version has been translated and validated in many countries of the world, including France, Norway, China, Italy, etc. [19–22]. This questionnaire development was aimed at differential diagnosis of pathophysiological causes of functional constipation in terms of cologenic (delayed intestinal transit), proctogenic (obstructed defecation due to dyssynergic defecation, or insufficient efforts, inadequate rectal propulsive forces), as well as mixed disorders [14]. At the same time, the linear discriminant analysis provided formulas for identifying the pathophysiological mechanisms of constipation with an accuracy of 55% (95% CI 43–67%) based on only five questionnaire items using the formula:
FDD = -5.813 + (0.969 × score for duration of constipation (question 1)) - (0.005 x score for laxative use (question 2)) - (1.484 × score for frequency of bowel movements (question 3)) + (1.899 × score for abdominal pain (question 6)) + (2.003 × score for time per bowel movement (question 9)),
where score is the number of points per question.
Interpretation: 9–20 points – FDD (proctogenic constipation); 8 points or less – a mixed form of constipation (cologenic and proctogenic).
Moreover, the KESS questionnaire has the best predictive power for identifying patients with FDD: 76% (95% CI 55–91%).
In our study, the Russian-language version of the questionnaire practically did not differ in effectiveness from the English version. We have demonstrated similar scores in patients with FDD and healthy volunteers compared to the original research. An essential factor is that the identified cut-off values for the score on the KESS questionnaire did not differ in our study from the original publication.
In contrast to similar studies, we attempted to analyze the factors that could affect the questionnaire's effectiveness, such as demographic characteristics, the presence and severity of rectocele, and obstetric history. We found that these factors do not significantly affect the effectiveness of the KESS questionnaire in the study population.
Comparison of the results of the Russian-language version of KESS and the results obtained using the Scoring System showed a high correlation of values. However, the latter does not consider factors such as the time spent on one bowel movement and abdominal pain. However, these factors are essential components of the calculation of formulas that determine the likelihood of a particular pathophysiological mechanism of constipation in a specific patient and show a close relationship with both the clinical picture and the results of functional investigations such as defecography and anorectal manometry [14, 23, 24]. Therefore, using the KESS questionnaire for the differential diagnosis of the pathogenetic mechanisms underlying the disease is preferable. In contrast, the combined use of both questionnaires can increase the diagnostic accuracy in general.
In this study, we did not assess the possibility of using the KESS questionnaire to evaluate the effectiveness and choice of management strategy. These aspects were not the aim of this study and required additional research in the Russian population. Nevertheless, international experience with the questionnaire shows that in constipation caused by delayed colonic transit, patients may benefit to a greater extent from the prescription of drugs that increase colonic motility (if organic pathology is reliably excluded). At the same time, restoration of pelvic floor muscle activity using physiotherapeutic methods (biofeedback therapy or tibial neuromodulation) will be effective in patients with functional disorders [25].
Conclusions
1. The Russian-language version of the KESS questionnaire demonstrates sensitivity similar to the original version regarding the diagnosis of constipation in patients with FDD.
2. Using a threshold >10, the total KESS score allows for reliable differentiation of patients with FDD from control subjects.
3. The use of the KESS questionnaire does not depend on the most common limiting factors, including demographic characteristics, obstetric history, and rectocele severity.
4. The Russian-language version of the KESS questionnaire can be used as a reliable and straightforward method for differential diagnosis of constipation with various pathophysiological mechanisms.
References
- Фоменко О.Ю., Титов А.Ю., Бирюков О.М., Мудров А.А., Белоусова С.В., Егорова Д.В. Диагностика и консервативное лечение функциональных расстройств дефекации. Колопроктология. 2016; 3: 48-54. https://dx.doi.org/10.33878/2073-7556-2016-0-3-48-54. [Fomenko O.U., Titov A.U., Birukov O.M., Mudrov A.A., Belousova S.V., Egorova D.V. Diagnosis and conservative treatment of functional disorders of defecation. Koloproktologia/Coloproctology. 2016; 3(57): 48-54. (in Russian)]. https://dx.doi.org/10.33878/2073-7556-2016-0-3-48-54.
- Фоменко О.Ю., Шелыгин Ю.А., Порядин Г.В., Титов А.Ю., Пономаренко А.А., Мудров А.А., Белоусова С.В. Функциональное состояние мышц тазового дна у пациентов с синдромом обструктивной дефекации. Колопроктология. 2017; 2: 55-61. [Fomenko O.Yu., Shelygin Yu.A., Poryadin G.V., Titov A.Yu., Ponomarenko A.A., Mudrov A.A. et al. Functional state of the pelvic floor muscles in patients with the pelvic prolapse. Koloproktologia/ Coloproctology. 2017; 2(60): 55-61. (in Russian)]. https://dx.doi.org/10.33878/2073-7556-2017-0-2-55-61.
- Preston D.M., Lennard-Jones J.E. Anismus in chronic constipation. Dig. Dis. Sci. 1985; 30(5): 413-8. https://dx.doi.org/10.1007/BF01318172.
- Rao S.S., Welcher K.D., Leistikow J.S. Obstructive defecation: a failure of rectoanal coordination. Am. J. Gastroenterol. 1998; 93(7): 1042-50. https://dx.doi.org/10.1111/j.1572-0241.1998.00326.x.
- Schwandner O., Stuto A., Jayne D., Lenisa L., Pigot F., Tuech J.J. et al. Decision-making algorithm for the STARR procedure in obstructed defecation syndrome: position statement of the group of STARR pioneers. Surg. Innov. 2008; 15(2): 105-9. https://dx.doi.org/10.1177/1553350608316684.
- Головенко А.О., Фоменко О.Ю., Егорова Д.В., Белоус С.С. Терапия по принципу «биологической обратной связи» в лечении хронического запора. Экспериментальная и клиническая гастроэнтерология. 2017; 3: 99-105. [Golovenko A.O., Fomenko O.Yu., Egorova D.V., Belous S.S. Biofeedback therapy for treatment of chronic constipation. Experimental and Clinical Gastroenterology. 2017; (3): 99-105. (in Russian)]. URL: https://cyberleninka.ru/article/n/terapiya-po-printsipu-biologicheskoy-obratnoy-svyazi-v-lechenii-hronicheskogo-zapora (дата обращения: 28.10.2020).
- Drossman D.A., Hasler W.L. Rome IV-functional GI disorders: disorders of gut-brain interaction. Gastroenterology. 2016; 150(6): 1257-61. https://dx.doi.org/10.1053/j.gastro.2016.03.035.
- Lacy B.E., Mearin F., Chang L., Chey W.D., Lembo A.J.,Simren M. et al. Bowel disorders. Gastroenterology. 2016; 150(6): 1393-407.e5. https://dx.doi.org/10.1053/j.gastro.2016.02.031.
- Rao S.S., Bharucha A.E., Chiarioni G., Felt-Bersma R., Knowles Ch., Malcolm A. et al. Anorectal disorders. Gastroenterology. 2016; 150(6): 1430-42.e4. https://dx.doi.org/10.1053/j.gastro.2016.02.009.
- Шелыгин Ю.А., ред. Клинические рекомендации. Колопроктология. М.: ГЭОТАР-Медиа; 2015. 528с. [Shelygin Yu.A., ed. Clinical recommendations. Coloproctology. M.: GEOTAR-Media; 2015. 528 p. (in Russian)]. http://www.gnck.ru/rec/recommendation_diag_2015.pdf (дата обращения 28.10.2020)
- Шелыгин Ю.А., Бирюков О.М., Титов А.Ю., Фоменко О.Ю., Мудров А.А. Существуют ли предикторы результатов хирургического лечения ректоцеле? Колопроктология. 2015; 1: 64-9. [Shelygin Y.A., Biryukov O.M., Titov A.Y., Fomenko O.Y., Mudrov A.A. Do the predictors of results of rectocele repair exist? Koloproktologia/ Coloproctology. 2015; 1(51):64-9. (in Russian)]. https://www.elibrary.ru/item.asp?id=23047272 (дата обращения 28.10.2020).
- Воробьев Г.И., Шелыгин Ю.А., Титов А.Ю., Подмаренкова Л.Ф., Зароднюк И.В., Мудров А.А. Особенности клинической картины и характер функциональных нарушений у больных ректоцеле. Колопроктология. 2004; 2: 8-14. [Vorobyev G.I., Shelygin Yu.A., Titov A.Yu., Podmarenkova L.F., Zarodnyuk I.V., Mudrov A.A. Features of the clinical picture and the nature of functional disorders in patients with rectocele. Coloproctology. 2004; 2(8): 8-14. (in Russian)].
- Agachan F., Chen T., Pfeifer J., Reissman P., Wexner S.D. A constipation scoring system to simplify evaluation and management of constipated patients. Dis Colon Rectum. 1996; 39(6): 681-5. https://dx.doi.org/10.1007/BF02056950.
- Knowles C.H., Eccersley A.J., Scott S.M., Walker S.M., Reeves B., Lunniss P.J. Linear discriminant analysis of symptoms in patients with chronic constipation: validation of a new scoring system (KESS). Dis. Colon Rectum. 2000; 43(10): 1419-26. https://dx.doi.org/10.1007/BF02236639.
- World Health Organization. Process of translation and adaptation of instruments. 2010; Available at: https://www.who.int/substance_abuse/research_tools/translation/en/ Accessed 24.08.2020.
- Rao S.S., Rattanakovit K., Patcharatrakul T. Diagnosis and management of chronic constipation in adults. Nat. Rev. Gastroenterol. Hepatol. 2016; 13(5): 295-305. https://dx.doi.org/10.1038/nrgastro.2016.53.
- Фоменко О.Ю., Козлов В.А., Алешин Д.В., Бирюков О.М., Белоусова С.В., Мудров А.А., Некрасов М.А. Консервативная реабилитация пациентов старших возрастных групп с нарушением опорожнения кишечника на фоне пролапса тазовых органов. Экспериментальная и клиническая гастроэнтерология. 2019; 5: 111-20. [Fomenko O.Yu., Kozlov V.A., Aleshin D.V., Biryukov O.M., Belousova S.V., Mudrov A.A., Nekrasov M.A. Conservative rehabilitation of the elderly patients with impaired bowel emptying and pelvic organs prolaps. Experimental and Clinical Gastroenterology. 2019; 165(5): 111-20. (in Russian)]. doi: 10.31146/1682-8658-ecg-165-5-111-120.
- Зароднюк И.В. Рентгенологическая дефекография в обследовании колопроктологических больных. Радиология-практика. 2004; 2: 26-30. [Zarodnyuk I.V. Radiological defecography in the examination of coloproctological patients. Radiology is a practice. 2004; 2: 26-30. (in Russian)]. http://www.radp.ru/db/20042/RP_2004_2_26.pdf (дата обращения 28.10.2020)
- Abramowitz L., Béziaud N., Labreze L., Giardina V., Caussé C., Chuberre B. et al. Prevalence and impact of constipation and bowel dysfunction induced by strong opioids: a cross-sectional survey of 520 patients with cancer pain: DYONISOS study. J. Med. Econ. 2013; 16(12): 1423-33.https://dx.doi.org/10.3111/13696998.2013.851082.
- Johnson E., Carlsen E., Mjåland O., Drolsum A. Intern invaginasjon i rectum behandlet med rektopeksi og sigmoideumreseksjon [Internal rectal invagination treated with rectopexy and sigmoid resection]. Tidsskr. Nor. Laegeforen. 2004; 124(5): 632-3. https://tidsskriftet.no/2004/03/aktuelt/intern-invaginasjon-i-rectum-behandlet-med-rektopeksi-og-sigmoideumreseksjon (дата обращения 28.10.2020)
- Wang C.P., Tsai P.Y. Efficacy of spinal magnetic stimulation in elderly persons with chronic constipation. J. Chin. Med. Assoc. 2012; 75(3): 127-31. https://dx.doi.org/10.1016/j.jcma.2012.02.004.
- Finco C., Luongo B., Savastano S., Polato F., Sarzo G., Caruso V. et al. Selection criteria for surgery in patients with obstructed defecation, rectocele and anorectal prolapse. Chir. Ital. 2007; 59(4): 513-20.
- Шелыгин Ю.А., Фоменко О.Ю., Морозов С.В., Маев И.В., Никитюк Д.Б., Алешин Д.В., Белоусова С.В., Бирюкова М.Г., Бордин Д.С., Веселов А.В., Гвоздев М.Ю., Индейкина Л.Х., Исаков В.А., Кашников В.Н., Кузьминов А.М., Кучерявый Ю.А., Титов А.Ю., Федоров Е.Д. Междисциплинарный консенсус по использованию русскоязычной терминологии методов аноректальной сфинктерометрии и профилометрии. Терапевтический архив. 2020; 92(8): 128-35. [Shelygin Yu.A., Fomenko O.Yu., Morozov S.V., Maev I.V., Nikityuk D.B. et al. Interdisciplinary consensus on Russian-language terminology of anorectal sphincterometry and profilometry. Therapeutic Archive. 2020; 92(8): 128-35. (in Russian)]. https://dx.doi.org/10.26442/00403660.2020.08.000766.
- Шелыгин Ю.А., Фоменко О.Ю., Морозов С.В., Маев И.В., Никитюк Д.Б., Алешин Д.В., Ачкасов С.И., Баркалова Е.В., Башанкаев Б.М., Бирюков О.М., Бирюкова М.Г., Бордин Д.С., Варданян А.В., Веселов А.В., Гвоздев М.Ю., Индейкина Л.Х., Исаков В.А., Касян Г.Р., Кузьминов А.М., Кучерявый Ю.А. и др. Аноректальная манометрия высокого разрешения. Рекомендации по русскоязычной терминологии на основе междисциплинарного консенсуса. Экспериментальная и клиническая гастроэнтерология. 2020; 2: 55-64. [Shelygin Yu.A., Fomenko O.Yu., Morozov S.V., Maev I.V., Nikityuk D.B. et al. High resolution anorectal manometry. Recommendations on Russian-language terminology based on interdisciplinary consensus. Experimental and Clinical Gastroenterology. 2020; 174(2): 55-64. (in Russian)]. https://dx.doi.org/10.31146/1682-8658-ecg-174-2-55-64.
- Fomenko O., Morozov S., Biryukov O., Kozlov V.A., Reutova A.A., Rumyantsev A.S. et al. Efficacy of conservative treatment of patients with functional defecatory disorders in patients with pelvic organ prolapse. Colorectal Disease. 2020; 22(Suppl. 1): 232. https://dx.doi.org/10.1111/codi.15332.
Received 11.06.2021
Accepted 03.11.2021
About the Authors
Oksana Yu. Fomenko, Dr. Med. Sci., Associate Professor, Head of the Laboratory of Clinical Pathophysiology, Ryzhikh NMRC of Coloproctology,Ministry of Health of Russia, +7(916)481-73-27, oksana671@yandex.ru, https://orcid.org/0000-0001-9603-6988; Scopus Author ID: 16401538300,
123423, Russia, Moscow, Salama Adilya str., 2.
Sergey V. Morozov, MD, Leading Researcher at the Department of Gastroenterology and Hepatology, Federal Research Center of Nutrition and Biotechnology,
https://orcid.org/0000-0001-6816-3058, Scopus Author ID: 19836606400, 109240, Russia, Moscow, Ustinsky proezd, 2/14
Dmitriy A. Morozov, Dr. Med. Sci. Professor, Head of L.P. Aleksanrov Department of Pediatric Surgery and Urology-Andrology, Sechenov First MSMU,
Ministry of Health of Russia, https://orcid.org/0000-0002-1940-1395, 119991, Russia, Moscow, Trubetskaya str., 8-2.
Andrey S. Shkoda, Dr. Med. Sci., Professor, Head of Vorokhobov City Hospital No 67, Moscow Health Department, https://orcid.org/0000-0002-9783-1796,
123423, Russia, Moscow, Salama Adilya str., 2/44-1.
Gennady V. Poryadin, Corresponding Member of the RAS, Dr. Med. Sci., Professor at the Department of Pathophysiology and Clinical Pathophysiology,
Honorary Professor of Pirogov RNRMU, Ministry of Health of Russia, rsmu@rsmu.ru, https://orcid.org/0000-0003-2010-3296; Scopus AuthorID: 55985271400,
117997, Russia, Moscow, Ostrovityanova str., 1.
Vladimir N. Kashnikov, Dr. Med. Sci., Deputy Director for Research and Clinical Work, Ryzhikh NMRC of Coloproctology, Ministry of Health of Russia,
https://orcid.org/0000-0002-5385-7898, 123423, Russia, Moscow, Salama Adilya str., 2.
Aleksandr A. Popov, Dr. Med. Sci., Professor, Head of the Department of Endoscopic Surgery, Moscow Regional Research Institute of Obstetrics and Gynecology,
https://orcid.org/0000-0001-8734-1673, Scopus Author ID: 57189994962, 101000, Russia, Moscow, Pokrovka str., 22а.
Anton A. Fedorov, MD, Senior Researcher at the Department of Endoscopic Surgery, Moscow Regional Research Institute of Obstetrics and Gynecology,
https://orcid.org/0000-0002-7674-5258, 101000, Russia, Moscow, Pokrovka str., 22а.
Inna A. Apolikhina, Dr. Med. Sci., Professor, Head of the Department of Aesthetic Gynecology and Rehabilitation, V.I. Kulakov NMRC for OG&P,
Ministry of Health of Russia; Professor of the Department of Obstetrics, Gynecology, Perinatology and Reproductology, Sechenov First MSMU, Ministry of Health of Russia, https://orcid.org/0000-0002-4581-6295, 117997, Russia, Moscow, Ac. Oparin str., 4.
Vladimir D. Chuprynin, PhD, Head of the Department of Operative Gynecology and General Surgery, V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia,
https://orcid.org/0000-0002-2997-9019, 117997, Russia, Moscow, Ac. Oparin str., 4.
Vladimir A. Kozlov, Associate Professor, PhD in Economics, Researcher, Ryzhikh NMRC of Coloproctology, Ministry of Health of Russia,
https://orcid.org/0000-0003-1788-1484; Scopus AuthorID: 55429890300, 123423, Russia, Moscow, Salama Adilya str., 2.
Svetlana V. Belousova, PhD, Senior Researcher at the Laboratory of Clinical Pathophysiology, Ryzhikh NMRC of Coloproctology, Ministry of Health of Russia,
https://orcid.org/0000-0003-1475-2599, 123423, Russia, Moscow, Salama Adilya str., 2.
Evgeniya S. Pimenova, PhD, Associate Professor at the Aleksanrov Department of Pediatric Surgery and Urology-Andrology, Sechenov First MSMU,
Ministry of Health of Russia; Pediatric surgeon, Speransky Childrens Hospital, https://orcid.org/0000-0001-7206-5987, 119991, Russia, Moscow, Trubetskaya str., 8-2.
Maksim A. Nekrasov, Junior Researcher at the Laboratory of Clinical Pathophysiology, Ryzhikh NMRC of Coloproctology, Ministry of Health of Russia,
https://orcid.org/0000-0002-5767-0123, 123423, Russia, Moscow, Salama Adilya str., 2.
Sergey I. Achkasov, Dr. Med. Sci., Professor, Head of the Department of Oncology and Colon Surgery, Ryzhikh NMRC of Coloproctology, Ministry of Health of Russia,
https://orcid.org/0000-0001-9294-5447, 123423, Russia, Moscow, Salama Adilya str., 2.
Corresponding author: Oksana Yu. Fomenko, oksana671@yandex.ru
Authors' contributions: Fomenko O.Yu., Achkasov S.I., Poryadin G.V., Shkoda A.S. – conception and design of the study; Belousova S.V., Fedorov A.A., Nekrasov M.A. – data collection and analysis; Kozlov V.A. – statistical analysis;
Fomenko O.Yu., Morozov S.V. – manuscript drafting; Morozov D.A., Kashnikov V.N., Pimenova E.S., Popov A.A.,
Apolikhina I.A., Chuprynin V.D. – manuscript editing.
Conflicts of interest: The authors have no conflicts of interest to declare.
Funding: There was no funding for this study.
Patient Consent for Publication: All patients provided informed consent for the publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available on request from the corresponding author after approval from the principal investigator.
For citation: Fomenko O.Yu., Morozov S.V., Morozov D.A.,
Shkoda A.S., Poryadin G.V., Kashnikov V.N., Popov A.A., Fedorov A.A.,
Apolikhina I.A., Chuprynin V.D., Kozlov V.A., Belousova S.V.,
Pimenova E.S., Nekrasov M.A., Achkasov S.I. Validation of the Russian-language version of the questionnaire for assessing chronic constipation severity.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2021; 12: 136-145 (in Russian)
https://dx.doi.org/10.18565/aig.2021.12.136-145