Микробиота влагалища – это совокупность микроорганизмов, которые активно заселяют слизистую влагалища и создают динамическую систему, определяющую репродуктивное здоровье женщины [1, 2]. В структуре микробиоты влагалища женщин насчитывается более 40 видов микроорганизмов, при этом доминируют Lactobacillus spp. (90–95%), остальные 5–10% микробиоты представлены облигатными анаэробными и, в меньшей степени, факультативно-анаэробными, аэробными и микроаэрофильными бактериями [3]. Микробиота влагалища также может включать условно-патогенные микроорганизмы (УПМ), которые мигрируют из кишечной микробиоты, способные при определенных условиях вызывать инфекционно-воспалительные заболевания женских половых путей. Выделение микроорганизмов из биологического материала и тем более их индикация (например, с помощью ПЦР-диагностики) не являются доказательством их этиологической роли, так как те же самые микроорганизмы колонизируют влагалище в норме. Именно нарушения количественных соотношений в бактериальном сообществе влагалища приводят к развитию клинических проявлений неспецифического вагинита [4].
Вагинит – это воспалительное заболевание слизистой оболочки влагалища инфекционной или неинфекционной природы [5]. Вагинит является одной из наиболее распространенных причин обращения к врачу-гинекологу и зачастую носит рецидивирующий характер течения заболевания. В современных условиях эффективное лечение прежде всего должно быть направлено на восстановление нормального баланса вагинального микробиома и поддержание здорового равновесия его бактериальных компонентов.
В рекомендациях Американской коллегии акушеров-гинекологов указываются наиболее часто встречающиеся инфекционные поражения слизистой влагалища: кандидозный вульвовагинит (КВВ) – 17–39%, бактериальный вагиноз (БВ) – 22–50% и трихомониаз – 4–35% [6].
Благодаря внедрению современных методов микробиологического исследования появилась возможность обнаружения специфических возбудителей, в том числе T. vaginalis, у пациенток, предъявляющих жалобы на выделения из половых путей [7].
Структура этиологии КВВ, развитие которого ранее связывали чаще всего с Candida albicans, меняется. Примерно у 15% пациенток в настоящее время КВВ вызывается представителями дрожжевых грибов Candida «non-albicans» видов, например, Candida glabrata, для лечения которых обычно рекомендуется применение локальных противогрибковых препаратов, но с учетом антибиотикограммы [8].
Появляется все больше исследований, посвященных изучению смешанных форм (микст-инфекций), которые часто характеризуются рецидивирующим течением и требуют особого подхода к лечению [9,10]. В некоторых случаях постановка диагноза может вызвать затруднения у врача акушера-гинеколога. Смешанный вагинит – воспалительное заболевание влагалища, вызванное как минимум двумя патогенами, что приводит к выраженному нарушению вагинальной микробиоты и появлению более сложного сочетания вагинальных симптомов и признаков, затрудняющих диагностику [9, 10]. Схожесть выделений из половых путей в сочетании с повышением рН часто усложняет проведение дифференциальной диагностики аэробного вагинита (АВ) и бактериального вагиноза (БВ), а, следовательно, усложняется назначение оптимальной терапии. Таким образом, важно, чтобы в существующей нормативно-правовой документации и клинических рекомендациях была оптимальная информация для практикующих врачей акушеров-гинекологов, позволяющая более корректно устанавливать клинический диагноз и составлять план лечения на базе доказательной медицины, для снижения рецидивов и осложнений.
Бактериальный вагиноз
БВ – невоспалительный синдром, характеризующийся дисбиозом вагинальной микробиоты, выраженный в снижении количества лактобацилл (вплоть до полного их исчезновения) и в увеличении количества облигатных и факультативных анаэробных УПМ. Это определение приводится в новом документе «Клинические рекомендации. Бактериальный вагиноз» от 2022 г., разработанном Российским обществом дерматовенерологов и косметологов и утвержденном Минздравом России [3]. Обращает на себя внимание, что в утвержденных РОАГ «Клинических рекомендациях. Воспалительные болезни шейки матки, влагалища и вульвы» (2021) [11] нет раздела «бактериальный вагиноз», что подчеркивает невоспалительный характер этого заболевания.
Международная классификация болезней 10-го пересмотра (МКБ-10) не выделяет БВ в самостоятельное заболевание, и статистически его относят к коду N89 «Другие невоспалительные заболевания влагалища».
В последние годы при использовании молекулярно-биологических методов и метода MALDI-TOF-MS анализа показано, что существует гораздо большее разнообразие микроорганизмов, ассоциированных с БВ, чем считалось ранее. Действительно, БВ – полимикробное дисбиотическое заболевание, при котором на фоне резкого уменьшения содержания Lactobacillus spp. увеличивается количество факультативных и облигатных анаэробов и микроаэрофилов: Gardnerella vaginalis, Peptostreptococcus, Clostridiales spp., Prevotella spp., Bacteroides, Fusobacterium, Veillonella, Eubacterium, Atopobium vaginaе, Mobiluncus spp. и др. На современном уровне знаний признается ведущая роль G. vaginalis и A. vaginaе в этиопатогенезе БВ [3].
По мировым статистическим данным, БВ занимает одно из первых мест среди заболеваний влагалища и развивается преимущественно у женщин репродуктивного возраста: у 80–87% пациенток вне беременности с патологическими вагинальными выделениями и у 37–40% беременных женщин.
В последнее время наряду с общеизвестными ключевыми звеньями патогенеза БВ обнаружены новые данные, которые складываются в более сложную картину, представляющую патологический «замкнутый круг» [3]:
- снижение титра лактобацилл обусловливает снижение концентрации молочной кислоты;
- сдвиг рН влагалища в щелочную сторону;
- увеличение количества G. vaginalis в синергизме с анаэробами;
- увеличение выработки ваголизина, способствующее повреждению эпителия влагалища;
- избыток углеводов вследствие повышенного цитолиза эпителия, приводящий к усилению синтеза жирных кислот (С3–С6) – маркерных метаболитов БВ;
- истощение запасов гликогена, усугубляющее деструкцию эпителиальных клеток влагалища.
Кроме того, по последним данным, БВ связан с развитием полимикробной биопленки. Длительно существующая биопленка обусловливает [3]:
- затяжное течение и склонность к хроническому патологическому процессу;
- повышенную вероятность диссеминации возбудителя;
- неэффективность традиционной терапии.
Для БВ характерны гомогенные беловато-серые выделения с неприятным «рыбным» запахом, усиливающиеся после незащищенного полового акта, дискомфорт в области наружных половых органов, диспареуния и др. Однако при осмотре слизистой оболочки вульвы и влагалища проявления воспалительной реакции отсутствуют.
Верификация диагноза БВ осуществляется на основании следующих лабораторных исследований [3]:
- микроскопические исследования влагалищного отделяемого – выявление «ключевых» клеток в мазках, окрашенных по Граму;
- микробиологические исследования (классические, с видовой идентификацией бактерий методом MALDI-TOF-MS анализа, и молекулярно-биологические при помощи мультиплексной ПЦР).
Для подтверждения диагноза БВ применяют критерии Амселя, при этом необходимо наличие не менее 3 из 4 критериев [3]:
- влагалищные выделения густые и гомогенные по своей консистенции, часто с неприятным «рыбным» запахом;
- изменение значений вагинального рН (>4,5);
- положительный результат аминотеста (определение летучих аминов – появление «рыбного» запаха при смешивании на предметном стекле отделяемого вагинального тракта с 10% раствором гидроокиси калия);
- наличие «ключевых» клеток при микроскопическом исследовании мазка, полученного со слизистой влагалища.
Для БВ микроскопическое исследование влагалищного отделяемого является наиболее простым, низкозатратным и быстрым методом, позволяет исключить КВВ (при визуализации дрожжевых клеток, псевдомицелия дрожжеподобных грибов), а также обнаружить «ключевые» клетки и оценить степень воспаления. Молекулярно-биологические методы исследования (мультиплексная ПЦР в реальном времени) имеют важное диагностическое значение для выявления высоких титров микроорганизмов, ассоциированных с БВ, т.к. качественное обнаружение только лишь G. vaginalis, и/или A. vaginaе, и/или Mobiluncus spр. методом ПЦР не дает оснований для подтверждения диагноза БВ [12].
Отсутствие 3 из 4 критериев Амселя, воспалительные изменения стенки влагалища, несмотря на характерные для БВ симптомы и признаки (гомогенные выделения, обильно покрывающие стенку влагалища, повышение рН и др.), не позволяют ставить диагноз БВ. На современном уровне знаний воспалительное заболевание влагалища, связанное с наличием двух и более аэробных и факультативно-анаэробных микроорганизмов, должно расцениваться как смешанный вагинит, проявления которого часто атипичны, а диагностика и лечение являются более сложными.
Стандартная схема фармакотерапии БВ у небеременных пациенток репродуктивного возраста кардинально отличается от подходов к лечению воспалительных заболеваний влагалища, в том числе АВ, и направлена на элиминацию повышенного количества анаэробных микроорганизмов [3]. Клинический эффект обеспечивается назначением этиотропных препаратов группы 5-нитроимидазола (метронидазол перорально или интравагинально) или клиндамицина (интравагинально), сопоставимых по своей эффективности, хотя предпочтение рекомендуется отдавать локальной терапии. У беременных женщин применяются пероральные формы этих препаратов, начиная со II триместра беременности.
Аэробный вагинит
АВ – это воспаление слизистой оболочки влагалища вследствие нарушения микробиоценоза влагалища и воздействия условно-патогенных аэробных и факультативно-анаэробных микроорганизмов [8, 11]. В рекомендациях РОАГ (2019), АВ – это воспалительное заболевание слизистой оболочки влагалища, возникающее при активации и воздействии на эпителиальные клетки условно-патогенных аэробных микроорганизмов [13]. Термин «аэробный вагинит» впервые был предложен G. Donders в 2002 г. для обозначения нарушения микробиоценоза влагалища, сопровождающегося воспалением и отличного от БВ [14].
Для АВ характерны обильные желтоватые выделения, чаще с неприятным запахом, выраженная гиперемия и отек слизистой оболочки влагалища, при этом пациентки испытывают дискомфорт во влагалище, зуд, жжение, раздражение вульвы, диспареунию.
АВ характеризуется резким снижением количества лактобацилл, усиленным ростом грамотрицательной или грамположительной аэробной микрофлоры, главным образом, Escherichia coli или Enterococcus spp., выраженной лейкоцитарной реакцией и увеличением рН. В последующем происходит повышение рН, которое может быть более значительным, чем при БВ (> 4,5, нередко >6) [15].
Аэробы запускают цитокиновый каскад воспаления и провоцируют развитие вагинита и его симптоматики (зуда, жжения). Анаэробы же, наоборот, ингибируют воспалительную реакцию посредством синтеза короткоцепочечных жирных кислот.
Таким образом, в отличие от БВ, AВ – это воспалительный вариант патологии влагалища, для которого характерны воспаление слизистой влагалища, высокие уровни провоспалительных цитокинов, рекрутирование так называемых «токсических лейкоцитов» (гранулоцитов), отражающих наличие выраженной воспалительной реакции, чего не происходит при БВ [16]. В редких случаях АВ может протекать в тяжелой форме, когда гиперемия и отек стенки влагалища особенно ярко выражены, такая форма АВ носит название «десквамативный воспалительный вагинит» [17].
МКБ-10 не выделяет этиологический фактор воспаления при вульвовагинитах, поэтому АВ не представлен как самостоятельное заболевание и статистически его относят к категориям: N73 «Другие воспалительные болезни женских тазовых органов», N76 «Другие воспалительные болезни влагалища и вульвы», N76.0 «Острый вагинит» и N76.1 «Подострый и хронический вагинит».
Для лабораторной диагностики АВ характерны:
- повышение рН>4,5;
- негативный тест с 10% КОН;
- выраженная лейкоцитарная реакция (при микроскопическом исследовании мазков, окрашенных по Граму, важным критерием является соотношение >10 лейкоцитов к 1 эпителиальной клетке в поле зрения).
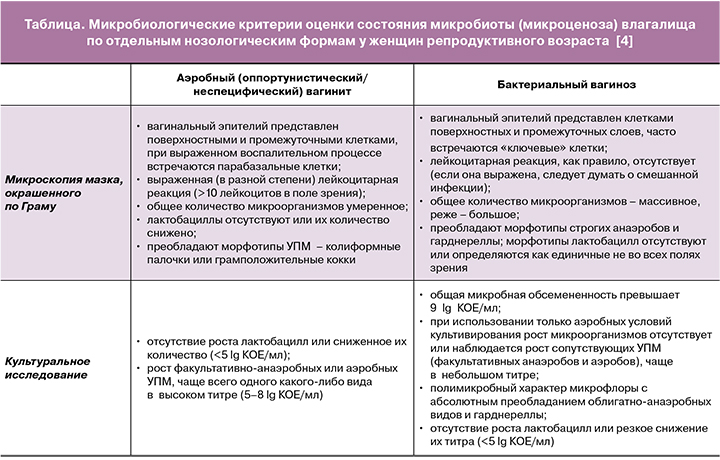
С 2011 г. в ФГБУ «НМИЦ АГП им В.И. Кулакова» Минздрава России используется медицинская технология «Интегральная оценка микробиоты влагалища. Диагностика оппортунистических вагинитов», где обозначено, что диагностика вагинитов основана на сочетании микроскопии мазков, окрашенных по Граму, и культурального исследования вагинального отделяемого, что дает возможность с наименьшими экономическими затратами получить достоверную информацию о состоянии микробиоты влагалища, диагностировать инфекции, вызванные УПМ, и предложить наиболее рациональные схемы этиотропного лечения при выявлении возбудителя в каждом конкретном случае» (таблица) [4].
В клинических рекомендациях РОАГ (2021) «Воспалительные болезни шейки матки, влагалища и вульвы» отмечается, что «для лечения АВ с целью эрадикации УПМ и клинического выздоровления могут быть использованы зарегистрированные на территории РФ для лечения вульвовагинитов и цервицитов противомикробные препараты (антибиотики, противогрибковые препараты и антисептики), по АТХ – Антисептики и противомикробные препараты для лечения гинекологических заболеваний».
Терапевтический выбор при АВ предполагает применение антибиотиков широкого спектра действия, обладающих действием против большинства бактерий кишечного происхождения, бактерицидным эффектом и, что немаловажно, слабым или полным отсутствием влияния на нормальную вагинальную микробиоту [11].
Смешанный вагинит
В России термин «смешанный вагинит» имеет большую историю и определялся ранее как бактериально/грибково/трихомонадный процесс. В настоящее время термин «смешанный вагинит» закреплен в проекте клинических рекомендаций РОАГ (2021) «Воспалительные болезни шейки матки, влагалища и вульвы» как «воспалительное заболевание влагалища, вызванное как минимум двумя патогенами», что, несомненно, усложняет клиническую картину и затрудняет постановку диагноза [11].
Результаты систематического обзора литературы за последние 10 лет по изучению смешанных вагинитов показали достаточно высокую частоту сочетания AВ и БВ по сравнению с числом других смешанных вагинитов: от 18,24 до 54,90% [10, 18]. Обращает внимание некоторое увеличение пропорции сочетания AВ+БВ среди других смешанных вагинитов с 2013 по 2016 гг., возможно, связанное с улучшением диагностики. Для верификации диагноза БВ необходимо наличие не менее 3 из 4 критериев Амселя и отсутствие воспалительной реакции со стороны слизистой влагалища при осмотре и выраженной лейкоцитарной реакции при микроскопии (соотношение лейкоциты/эпителий <1), в противном случае сочетание аэробных и анаэробных УПМ может расцениваться как смешанный вагинит.
В международном многоцентровом исследовании PRISM (2019), проведенном в 4 европейских странах, комбинация полимиксин B+неомицин+нистатин продемонстрировала высокую клиническую эффективность в лечении разных видов вагинальной инфекции, в том числе эффективность при смешанном вагините составила 87,7% [19].
Известно, что оптимальное лечение вагинальных инфекций должно оказывать минимальный эффект на Lactobacillus spp., что способствует нормализации pH, а значит, повышает эффективность лечения и служит профилактикой рецидивов. В нескольких исследованиях лечение комбинацией полимиксин В+неомицин+нистатин приводило к созданию благоприятных условий для восстановления нормального микробиоценоза влагалища, что позволяет не только сохранять лактобациллы, но даже усиливать их рост [20, 21]. Кроме того, к моменту окончательной оценки эффективности лечения на 12-е сутки от начала лечения аэробного и смешанного вагинита обнаружена полная элиминация УПМ, при этом препарат не оказывал негативного влияния на содержание Lactobacillus spp. по данным ПЦР-диагностики, у 97,2% пациенток отмечено значительное снижение pH влагалищной среды [21].
Таким образом:
- АВ и БВ являются разными клиническими формами (воспалительной и невоспалительной) заболеваний влагалища. Это подтверждают разные коды МКБ-10. В клинических рекомендациях РОАГ от 2021 г. БВ упоминается только как диагноз исключения для других вагинитов [11].
- АВ и БВ требуют различных подходов к терапии, что закреплено в отечественных рекомендациях [3, 11].
Смешанный вагинит, как часто встречающаяся форма вагинита, представляет терапевтическую проблему для врача акушера-гинеколога, т.к. УПМ при смешанном вагините определяются в различных комбинациях и труднее поддаются эрадикации, что объясняет более частые рецидивы [10].
Для верификации диагноза БВ необходимо наличие не менее 3 из 4 критериев Амселя, в противном случае сочетание аэробных и анаэробных УПМ может расцениваться как смешанный вагинит с соответствующими подходами к лечению. Тем более важна количественная оценка, поскольку в более низких концентрациях эти УПМ входят в состав нормального микробиоценоза влагалища [4].
Заключение
Основной целью лечения смешанного вагинита должно быть воздействие на аэробные микроорганизмы путем местного применения бактерицидных антибиотиков широкого спектра действия, в том числе в сочетании с противогрибковыми препаратами, для элиминации дрожжевых грибов и предотвращения развития резистентности УПМ к антимикробным препаратам. Одновременно с воздействием на основную причину развития симптоматики – аэробные бактерии, лечение должно способствовать созданию условий для сохранения эндогенных лактобацилл и нормализации микробиоты влагалища.