Стрессовая доминанта, возникающая после принятия факта о необходимости и неизбежности операции, становится триггером к запуску ряда патологических процессов в разных системах и органах женского организма, которые могут отрицательно сказаться на самой операции и ее исходе [1, 2]. При проведении предоперационного обследования боязнь анестезиологического пособия и оперативного вмешательства может способствовать изменению вагинального спектра микрофлоры в сторону увеличения количества условно-патогенной микрофлоры. Данный факт становится еще одной проблемой как для самой пациентки, учитывая, что операция может быть просто отменена, так и для оперирующего врача, принимая во внимание повышение рисков инфекционных осложнений в послеоперационном периоде. Таким образом, проведение предоперационной подготовки вагинального тракта женщин имеет большое значение.
Согласно приказу Минздрава России от 20.10.2020 г. №1130н «Об утверждении порядка оказания медицинской помощи по профилю "акушерство и гинекология"», все пациентки проходят плановое обследование перед операцией по утвержденному и рекомендуемому списку мероприятий предоперационной подготовки [3]. У ряда женщин диагностируются неспецифический вагинит, а также вульвовагиниты специфической этиологии, безусловно, требующие проведения терапии.
С неспецифическим вагинитом, вульвовагинитами различной этиологии, бактериальным вагинозом практикующие гинекологи также часто встречаются в своей рутинной практике [4–6]. Оценивая структуру воспалительных заболеваний нижнего генитального тракта, частота вышеупомянутых нозологий неуклонно растет [7, 8]. Проблема заключается в том, что отличительными особенностями данных патологических состояний являются полимикробный этиологический характер, скрытые/стертые клинические проявления, тенденция к частым рецидивам [9, 10]. Все это создает определенные трудности в выборе терапии. Особенно острым и актуальным этот вопрос становится при проведении предоперационной подготовки пациентки и имеющихся сжатых сроках лечения/профилактической подготовки вагинального тракта перед гинекологической операцией, которые обычно составляют 2–3 недели.
Рядом исследователей доказан полимикробный характер вагинальной флоры [11–14], качественный и численный состав которой непостоянны и изменяются в силу внешних и внутренних воздействий. Любое изменение состава вагинальной флоры – риск для возникновения бактериального вагиноза, неспецифического аэробного вагинита, грибковых и протозойных вагинитов. А в случае длительного отсутствия терапии – перехода к хронизации процесса [15], что в дальнейшем будет повышать риски инфекционных осложнений, особенно в ситуации, когда пациентка готовится к операции на фоне стресса и в послеоперационном периоде.
Одной из значимых и серьезных задач в современной гинекологии можно назвать снижение частоты септических осложнений в послеоперационном периоде. Понятно желание каждого практикующего специалиста идти в ногу со временем, но не всегда это возможно. Краеугольной проблемой в этом аспекте и камнем преткновения является повышение частоты резистентности микроорганизмов к антимикробным лекарственным препаратам. В рутинной практике гинеколог, столкнувшись с проблемой нарушения микрофлоры влагалища, будет назначать эмпирическую терапию, то есть он должен быть уверен в высокой полимикробной активности препарата и максимальной клинической эффективности терапии в патологическом очаге.
За последнее десятилетие на фармакологическом рынке РФ появился огромный спектр лекарственных препаратов для лечения неспецифического аэробного вагинита, вульвовагинитов различной этиологии, бактериального вагиноза, кандидозного кольпита. Зачастую в клинической практике гинеколог сталкивается с вагинитами со смешанным характером вагинальной микрофлоры, что, безусловно, требует комплексного подхода. В таких случаях для терапии назначаются комбинированные препараты, воздействующие на весь спектр патологической смешанной флоры. В частности, целесообразно применить комплексный препарат «Таржифорт» компании «Авексима», имеющий в составе оптимальную комбинацию: метронидазол – 500 мг, хлорамфеникол – 200 мг, натамицин – 150 мг, гидрокортизона ацетат – 15 мг. Препарат «Таржифорт» производится в форме вагинальных свечей, имеет оптимальный профиль безопасности и может быть назначен пациенткам как с патологическими влагалищными выделениями, наличием зуда и дискомфорта в области вульвы, так и в качестве плановой предоперационной подготовки с целью санации вагинального тракта для снижения рисков септических осложнений и профилактики возникновения рецидивов неспецифического аэробного вагинита в послеоперационном периоде.
Для получения актуальных и современных данных по клинической эффективности препарата «Таржифорт» нами проведено клиническое исследование – наблюдение, целью которого была оценка эффективности предоперационной санации вагинального тракта комбинированным препаратом «Таржифорт» у пациенток с полимикробным характером вагинальной микробиоты на фоне различного спектра гинекологической патологии (неспецифический аэробный вагинит, вульвовагинит различной этиологии, бактериальный вагиноз, кандидозный кольпит), планирующих оперативное лечение, и с целью снижения осложнений в послеоперационном периоде.
Материалы и методы
В рамках исследования – клинического наблюдения проведены клинико-лабораторное обследование и предоперационная подготовка вагинального тракта 96 пациенток в возрасте от 28 до 62 лет с многообразием нозологических форм гинекологической патологии, которые значились в очереди на оперативное лечение в одной из ГКБ ДЗ г. Москвы. При подготовке к плановому оперативному лечению на органах малого таза у данной категории пациенток были диагностированы различные нарушения состава вагинальной флоры: неспецифический аэробный вагинит, бактериальный вагиноз, кандидозный кольпит, а также смешанные вульвовагиниты. Все женщины были разделены на 3 группы в зависимости от нозологии: 1-я группа – 42/96 (43,8%) пациентки со смешанным вульвовагинитом, 2-я группа – 30/96 (31,2%) женщин с вульвовагинальным кандидозом, 3-я группа – 24/96 (25%) пациентки с бактериальным вагинозом.
Наблюдение за пациентками включало 3 визита до оперативного лечения и 1 визит после операции. На первом визите пациентка записывалась на плановую операцию (в среднем за 1 месяц до оперативного лечения). Перед оперативным лечением на первом визите всем пациенткам, помимо стандартного спектра предоперационного обследования, были проведены pH-метрия влагалища, бактериоскопическое исследование, комплексное исследование микрофлоры урогенитального тракта, основанное на использовании метода ПЦР (Фемофлор-16). Во время второго визита (15–21-й день до оперативного лечения) проводили анализ результатов диагностических мероприятий, упомянутых выше. По результатам диагностики женщинам ставили диагноз и назначали терапию. Учитывая наличие жалоб, клинических проявлений при активации условно-патогенной флоры влагалища, данные гинекологического осмотра, назначали местную санацию комбинированным препаратом «Таржифорт» (метронидазол – 500 мг, хлорамфеникол – 200 мг, натамицин – 150 мг, гидрокортизона ацетат – 15 мг) по 1 суппозиторию на ночь в течение 10 дней. На фоне местной санации давали оценку динамике клинических проявлений и эффективности терапии – приглашали пациенток на третий визит для повторного забора материала за 2–3 дня до даты операции.
Пациентки с диагностированными повторными нарушениями состава вагинальной микрофлоры не имели воспалительной реакции в мазках при бактериоскопическом исследовании, и в плановом порядке их брали на оперативное лечение согласно графику. Баквагиноз у них был выявлен за несколько дней до плановой операции, и поэтому они применяли «Таржифорт» вторым курсом в дни до операции и сразу с 1-х суток после операции. Таких пациенток было 9/96. Эти женщины приходили на следующий, четвертый визит через 3–4 недели после оперативного лечения для оценки эффективности терапии (2 курса лечения).
Результаты и обсуждение
Перед оперативным лечением всем пациенткам, которые обратилась в ГКБ ДЗ г. Москвы по поводу своего основного заболевания, было проведено предоперационное обследование согласно приказу Минздрава России от 20.10.2020 г. № 1130н «Об утверждении порядка оказания медицинской помощи по профилю "акушерство и гинекология"». Принимая во внимание наличие жалоб у пациенток, которые участвовали впоследствии в клиническом наблюдении, дополнительно были проведены тесты на определение нарушений характера вагинальной микрофлоры: pH-метрия влагалища, Фемофлор-16 – соскоб из влагалища.
Общая характеристика пациенток исследуемых групп включала возрастной аспект. Средний возраст женщин, принимавших участие в наблюдении, составил 38,5 (0,5) года. Спектр нозологической патологии, с которой пациентки обращались для оперативного лечения, был разнообразным, представлен на рисунке 1.
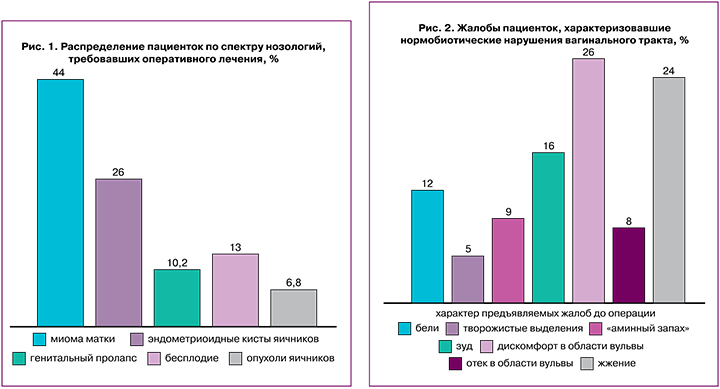
Помимо жалоб, патогномоничных основной нозологии, с которой пациентки обратились для оперативного лечения в стационар, на первых двух визитах женщины также предъявляли жалобы, характерные для нарушения микробиоценоза влагалища: патологические обильные бели/желтоватый/творожистый характер выделений из влагалища, отек слизистой влагалища, зуд, жжение, дискомфорт в области вульвы, «аминный» запах из влагалища. Ряд пациенток жалоб не предъявляли, но патологические изменения в анализах у них были выявлены. Распределение пациенток по нозологиям представлено на рисунке 2.
Все пациентки, прошедшие первичную диагностику перед оперативным лечением, имели нарушения вагинальной микрофлоры, характер спектра вагинальных нарушений показан на рисунке 3.
Пациентки были распределены в исследуемые группы исходя из полученных результатов по данным анализа Фемофлор-16: 1-я группа – пациентки со смешанным вульвовагинитом – 42/96 (43,8%), у которых флора вагинального тракта была представлена лактобактериями в сниженном количестве, выявлена патологическая кокковая микрофлора, во 2-й группе наблюдаемых – 30/96 (31,2%) женщин с вульвовагинальным кандидозом, у которых выявлены грибы рода Candida в диагностически значимом титре, 3-ю группу пациенток составили 24/96 (25%) женщины с бактериальным вагинозом, у них было выявлено значимое снижение количества лактобактерий в совокупности с повышенным содержанием Gardnerella vaginalis/Prevotella bivia/Porphyromonas, и/или Eubacterium, и/или Sneathia/Leptotrichia/Fusobacterium, и/или Megasphaera/Veillonella/Dialister, и/или Lachnobacterium/Clostridium, и/или Peptostreptococcus, и/или Atopobium vaginae. Таким образом, по структуре дисбиотических нарушений вагинального тракта у пациенток преобладали ассоциации условно-патогенных бактерий, грибы рода Candida, преимущественно вместе с анаэробами, и облигатно-анаэробные возбудители Gardnerella vaginalis, Atopobium vaginae и Eubacterium spp.
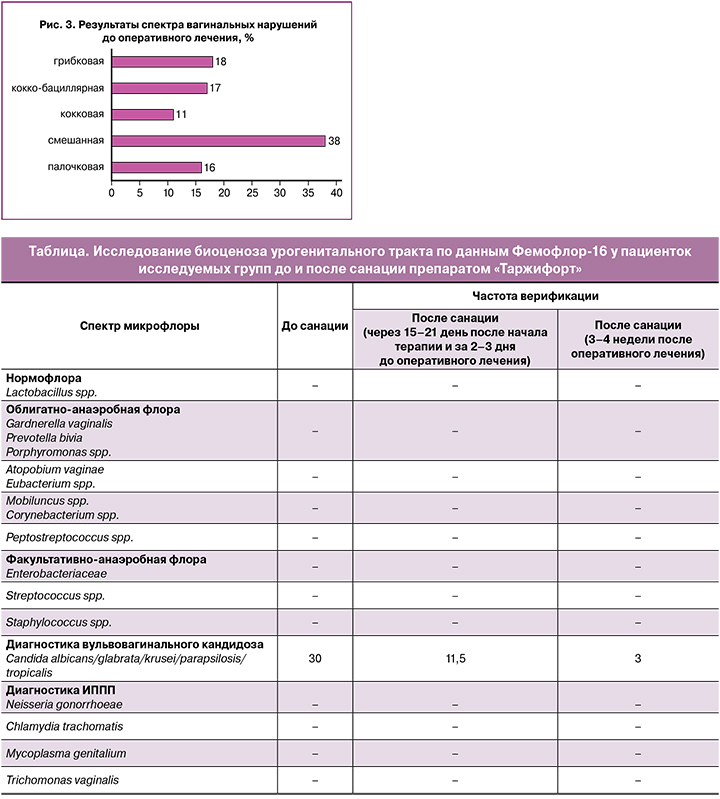
Принимая во внимание жалобы ряда пациенток (34,4%) и результаты предоперационной диагностики у пациенток, которые жалобы не предъявляли (65,5%), на первом и втором визитах всем женщинам была назначена санация влагалища комбинированным препаратом «Таржифорт» (метронидазол – 500 мг, хлорамфеникол – 200 мг, натамицин – 150 мг, гидрокортизона ацетат – 15 мг) по 1 суппозиторию на ночь интравагинально в течение 10 дней. Оценивали динамику эмпирической терапии у пациенток исследуемых групп. После курса первичной санации препаратом «Таржифорт» проводили комплексную количественную оценку микробиоценоза вагинального тракта (Фемофлор-16), в результате которой наблюдали значимое снижение концентрации условно-патогенной флоры вагинального тракта преимущественно за счет облигатно-анаэробной флоры. Результаты представлены в таблице.
У 14 пациенток из 1-й группы со смешанным вульвовагинитом не было выявлено нарушений вагинальной микрофлоры по данным Фемофлор-16, несмотря на наличие у них жалоб и изменений в бактериоскопическом анализе: отмечались лейкоциты более 10 в поле зрения и незначительное количество эпителиальных клеток в поле зрения, а также наличие «ключевых клеток». После одного полного курса препарата «Таржифорт» нормализация микрофлоры была достигнута на втором и третьем визитах (в период с 15-го по 21-й дни после начала терапии и за 2–3 дня до оперативного лечения) у 86/96 (89,5%) пациенток, а на четвертом визите через месяц после оперативного лечения у 91/96 (94,8%) женщины при комплексной оценке урогенитальной микрофлоры было подтверждено восстановление влагалищной флоры с присутствием лактонормофлоры, что показало эффективность препарата «Таржифорт».
В 1-й группе пациенток спектр выявленной облигатно-анаэробной микрофлоры до начала санации был разнообразным. По данным контрольных исследований (Фемофлор-16), повторные нарушения микрофлоры были выявлены у 7/28 женщин (учитывая, что у 14 пациенток ранее был диагностирован нормоценоз), таким образом, 25% пациенток был назначен повторный курс санации до оперативного лечения. Терапию женщины 1-й группы продолжили и в послеоперационном периоде, учитывая отсутствие противопоказаний к местной санации препаратом «Таржифорт». В данной группе женщин со смешанным характером вульвовагинита только у 1 пациентки через месяц после оперативного лечения на четвертом визите был выявлен рецидив смешанного аэробного вагинита, что в целом могло быть ассоциировано с основной нозологической патологией – генитальным пролапсом, по поводу которого проводилось оперативное лечение, и возможной реакцией слизистой влагалища на шовный материал, а также с выраженными нарушениями местного иммунного статуса, что препятствовало быстрому восстановлению вагинальной микрофлоры и потребовало дополнительных назначений для ускорения репаративных процессов слизистой влагалища.
Во 2-й группе женщин с диагностированным вульвовагинальным кандидозом как по результатам бактериоскопической диагностики, так и по данным Фемофлор-16 только у 2 пациенток после санации эффекта не отмечали. Им назначили повторный курс препарата «Таржифорт» совместно с системными антимикотиками. При контрольном заборе материала у 1 женщины по данным лабораторной диагностики была выявлена грибковая инфекция рода Candida. При этом обе женщины не предъявляли жалобы на зуд и творожистые выделения из влагалища, патогномоничные для вульвовагинального кандидоза.
Оценивая 3-ю группу пациенток, у которых присутствовала факультативно-анаэробная флора в диагностически значимых титрах в вагинальном тракте, было показано, что после санации только 4 из 24 пациенток потребовался повторный курс терапии.
Всем пациенткам с пролапсом гениталий назначали после операции препарат «Таржифорт» в течение 10 дней.
На контрольном визите через 4 недели после оперативного лечения ни одна из женщин в данной группе не предъявляла жалоб. Клиническая эффективность препарата «Таржифорт» была подтверждена лабораторно, при микроскопии влагалищных мазков и оценке pH-метрии вагинального содержимого, которое смещалось в сторону кислого pH.
Таким образом, при оценке жалоб на патологические выделения и их объем после проведенного лечения зафиксировано снижение объема вагинальных выделений у 39/42 92,4% пациенток в 1-й группе. Отмечено нивелирование жалоб на зуд, жжение и дискомфорт в области вульвы у 23/30 (78,2%) и 16/24 (66,4%) женщин во 2-й и 3-й группах соответственно. «Аминный запах» отсутствовал у всех женщин, получавших терапию.
Спектр вагинальной микрофлоры, который оценивали сразу после терапии (до оперативного лечения) и через 3–4 недели после операции, был нормальным у 91,4% пациенток. Данное состояние сохранялось у 88,2% женщин после операции. Спектр условно-патогенной вагинальной флоры был разнообразным, как было показано в нашем клиническом наблюдении.
Следует подчеркнуть, что во всех нозологических группах у пациенток, принимавших участие в данном клиническом наблюдении, зафиксировано отсутствие послеоперационных осложнений. Ранний послеоперационный период у всех пациенток протекал гладко. При клиническом наблюдении за женщинами как до оперативного лечения, так и после него побочных эффектов на фоне применения препарата «Таржифорт» зафиксировано не было, что свидетельствует о хорошей переносимости данного препарата. Особого внимания заслуживает когорта пациенток с генитальным пролапсом, у которых априори нарушена анатомия тазового дна, присутствуют нарушения как микробиоценоза влагалища [16, 17], что повышает риски восходящей инфекции, так и послеоперационных осложнений [18], учитывая депрессию местного иммунитета. Данный факт подтверждает необходимость как глубокого обследования пациенток с определением состава вагинальной микрофлоры, так и назначения соответствующей терапии, предшествующей оперативному лечению с лечебной целью или для профилактики восходящей инфекции.
Заключение
Наш опыт применения препарата «Таржифорт» подтвердил его клиническую эффективность и лекарственную безопасность. По нашему мнению, этот препарат можно рекомендовать к применению в качестве терапии смешанных вагинитов, вульвовагинального кандидоза и бактериального вагиноза. Препарат «Таржифорт» благодаря комплексному составу патогенетически воздействует на весь спектр бактериальных ассоциаций, характерных для бактериального вагиноза, обладает антимикотической активностью против грибковой флоры рода Candida, эффективен в отношении факультативно-анаэробных бактерий. «Таржифорт» не вызывает побочных эффектов и осложнений на фоне местной терапии, что особенно важно в послеоперационном периоде. Назначение препарата «Таржифорт» в качестве эмпирической терапии будет целесообразным и с фармакоэкономической точки зрения, учитывая невысокую стоимость препарата. Данный факт будет важен для врача амбулаторного звена и врача стационара, что безусловно повысит комплаентность к терапии.
Благодаря оптимальному составу препарат «Таржифорт» оказывает противомикробное и антимикотическое действия, устраняет клинические проявления дисбаланса микрофлоры влагалища: исчезают зуд и дискомфорт в области вульвы, снижается выраженная патологическая секреция влагалищных выделений.
Препарат «Таржифорт» может быть широко применен в акушерско-гинекологической практике и в качестве профилактической санации вагинального тракта у пациенток перед плановыми гинекологическими операциями.