Ultrasound monitoring of the surgical treatment effectiveness in patients with cervical and uterine cancers
Aim: The aim of the study was to determine ultrasound criteria for progression of cervical cancer and uterine cancer in patients after surgical and complex treatment with dynamic observation.Chekalova M.A., Kryazheva V.S.
Materials and methods: The study included 10 patients with diagnosis of cervical and uterine cancers. The patients underwent surgical and complex treatment. Standard and advanced ultrasound technologies were used to identify early progression of these diseases. Elastography for stiffness assessment was performed using ultrasound diagnostic systems Hitachi Arietta V70, Toshiba Aplio 500.
Results: Based on the obtained results, a number of ultrasound-derived criteria for recurrences of cervical and uterine cancers as focal lesions after complex treatment were found. They allowed to detect suspected disease progression up to clinical manifestations. Differential diagnostics showed benign postoperative changes, and ultrasound examination showed their specific sighs. Additionally, ultrasound criteria were defined for the unchanged vaginal stump after surgical treatment. The signs were presented both in standard gray-scale mode and using advanced ultrasound technologies — elastography and stiffness measurements.
Conclusion: Multiparametric ultrasound examination with standard grayscale imaging mode including elastography and stiffness assessment is a reliable way to improve the quality of preclinical diagnosis of recurrences and metastases of cervical and uterine cancers after complex treatment, as well as differential diagnosis of benign postoperative changes.
Keywords
Cervical cancer (CC) ranks second in the structure of onсogynecologic pathologies and fifth in the structure of malignant neoplasms among the female population [1].
Uterine cancer (UC) ranks six among malignant neoplasms among the female population in the world and reaches 4.8% [1].
Due to steady growth of these diseases, the most important objective of modern oncogynecology is to improve the quality of preclinical diagnosis and progression and recurrence prediction of CC and UC.
According to Nechushkina V.M., the recurrence rate for stage I UC is 15.9% and 30.1% for stage II [2].
Preclinical diagnosis and prediction of recurrences metastasis of CC and UC after surgical treatment is extremely important to improve patient survival, as well as quality of life [3, 4].
Ultrasound (US) examination is one of the most common techniques in the diagnosis of oncogynecologic pathology. It is a non-invasive available diagnostic technique that can be used repeatedly.
Complex use of ultrasound in patients with cervical and uterine cancers, make it possible to visualize and assess the echographic structure, shape and contours of the cervix and uterus, to determine tumor size and volume; and in locally advanced cancer to assess tumor growth into nearby structures, as well as the degree of vascularization and stiffness in the visualized area of interest.
New techniques are constantly being developed in the arsenal of ultrasound diagnostics that allow to extend the area and improve the quality of visualization. One of these methods is elastography (EG) for non-invasive assessment of the stiffness of tissue by "ultrasound palpation" in real time.
The aim of the study was to determine ultrasound criteria for progression of cervical and uterine cancers in patients after surgical and complex treatment with dynamic observation.
Materials and methods
The study included 102 patients under follow-up surveillance during 5 years after surgical treatment. CC was diagnosed in 56 (54.9%) cases, and UC in 46 (44.1%).
The average age of patients with diagnosis of CC was 48.9±4.5 years, and 57.8±3.2 years with diagnosis of UC.
Considering the method of treatment for patients included in the study, mostly CC stage T1b1 (IB1) in 56 women (54.9 %) was diagnosed, and UC stage T1b (IB) in 46 women (45.1%).
Most patients – 48 (47.1%) underwent surgical treatment that included extirpation of the uterus and its appendages, and lymph node dissection. Among them, 40 patients (38.9%) received combined treatment and 14 patients (13.7%) received complex treatment.
In the process of dynamic monitoring, progression of the disease was detected in 61 patients (59.8%). During the period of surveillance (for more than 6 months), remission was detected in 41 patients (30.2%).
The minimum reccurence term for CC and UC was 6 months (n=9 (15.2%)), the maximum recurrence term 6 and more years (n=4 (6.8%)) after treatment. On average, in half of the patients under surveillance, progression of the disease was detected in the first 3 years after treatment.
According to the published data, reccurrence and metastases of cervical cancer are categorized into local (pelvic), loco-regional with tumor lesions in the pelvis and in the areas of regional metastasis, which include retroperitoneal lymph nodes located along common, external and internal iliac arteries [4, 5].
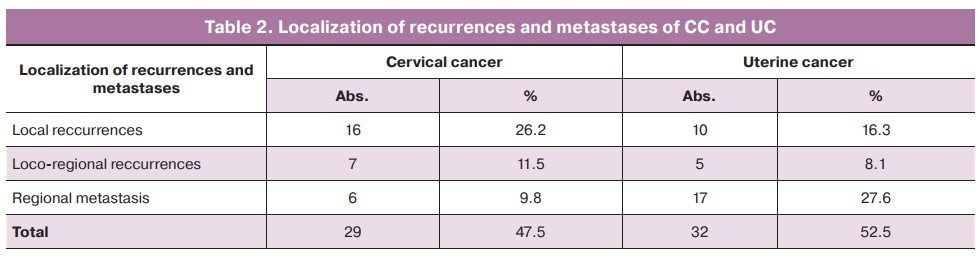
In our study, local recurrence of CC and UC was diagnosed in most cases –
in 38 patients (62.3%). Among them, in 12 patients (19.6%) along with local recurrence, metastasis were found in lymph nodes along the iliac (common, external, internal) and lumbar (para-aortic and paracaval) arteries.
In 21 cases (34.4%), only metastases in the retroperitoneal lymph nodes were found. In 18 (29.5%) cases, distant metastases in liver, cervical-supraclavicular lymph nodes were detected.
All cases of recurrence were confirmed by cytological and morphological investigation.
In 9 cases (27.3%), ultrasound-guided puncture biopsy of regional metastatic lesions was performed with subsequent verification. In 22 cases (66.7%), the obtained ultrasound data were confirmed by other imaging techniques (magnetic resonance imaging, positron emission tomography).
The ultrasound examination was performed using high-quality ultrasound imaging system Hitachi Arietta V70, Toshiba Aplio 500 with high visualization quality, color Doppler imaging (CDI), EG and assessment of tissue stiffness coefficient.
To assess the effectiveness of treatment, ultrasound imaging was performed in the following areas:
- The retroperitoneum, including the kidneys, pelvicalyceal system, renal collecting ducts, and retroperitoneal lymph nodes located along the abdominal aorta, inferior vena cava and iliac arteries.
- Pelvic area (vaginal wall, vaginal cuff and surrounding tissues).
The patients underwent ultrasound examination according to the established period: before treatment, one month, 3-6 months, 1 year, 1.5 years and further every year after treatment.
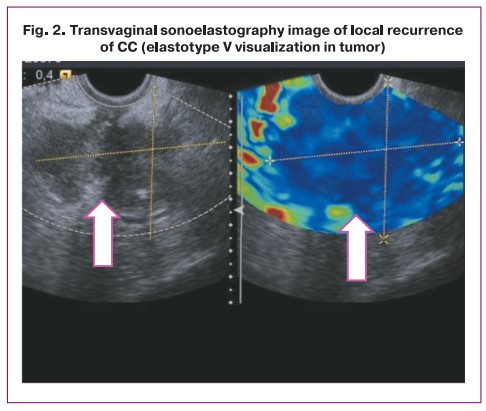
Elastography assessment was performed using five-degree scoring system consisting of elastograms adjusted for gynecological pathologies (Table 1) [6]. According to the classification, solid structures indicating tumors were mapped as elastotype V (blue color).
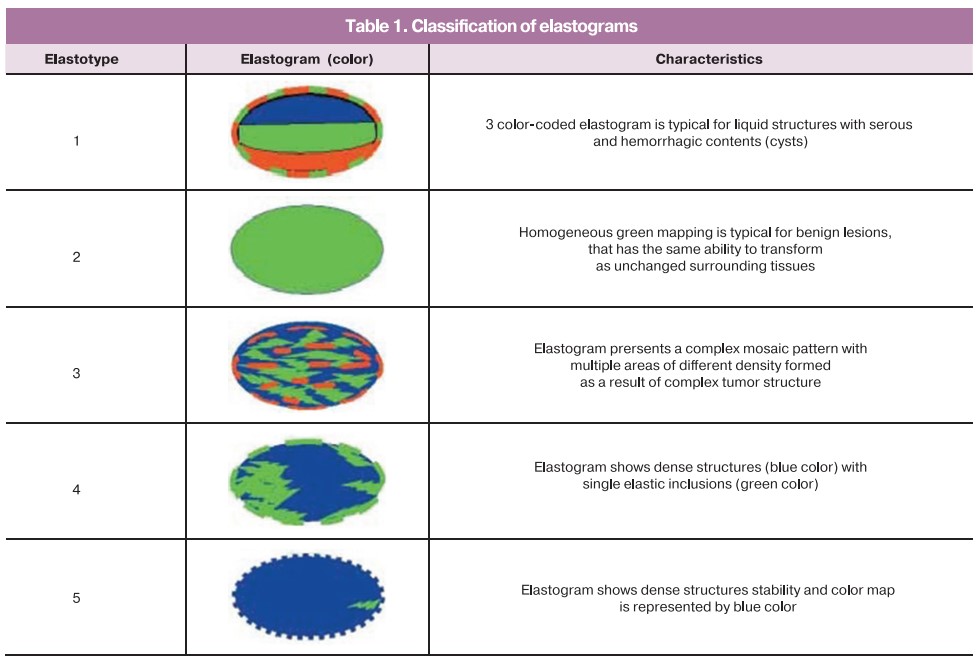
Assessment of tissue density coefficient using digital images of tissue density was an important addition to color elastograms for the differential diagnosis of visualized volumetric masses. The appropriate option was selected on the operating touch panel of the ultrasonic device to calculate the stiffness coefficient. Area A was set manually with maximum coverage in the pathological focus or normal tissue, then, preferably at the same level, area B was set in the reference tissue region. The diagnostic device calculated the obtained result automatically. It is important to note that, when elastometry was used, it was necessary to obtain reproducibility of the result.
Results and discussion
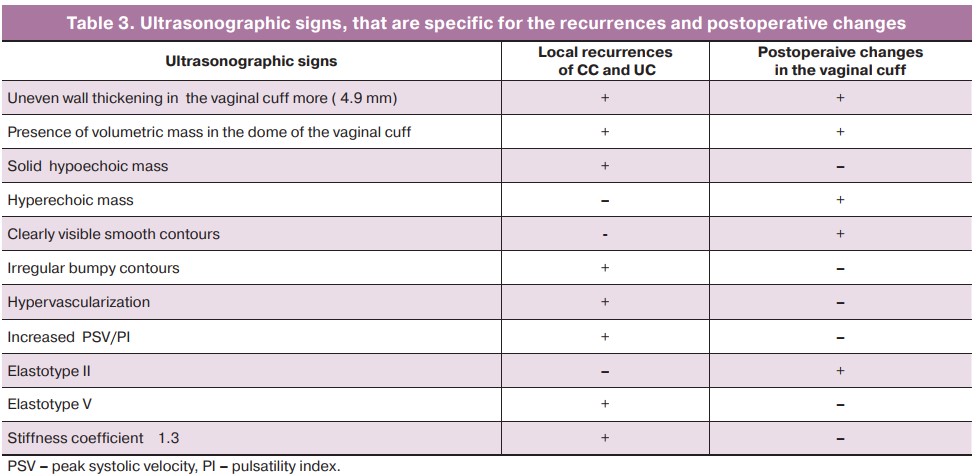
Our study found that CC is characterized by local and loco-regional recurrences, while regional metastases are specific for UC. The incidence rates of diagnosed distant metastases of CC and UC were similar (Table 2).
Moreover, local recurrences of CC and UC after surgical and/or complex treatment had similar ultrasound signs; consequently, the major task of diagnostician was identification of the presence or suspicion of tumor process.
Visualization of changes, that indicated the presence of local recurrences, represented uneven wall thickening over 5.1 mm in the vaginal cuff. A solid hypoechoic mass was detected (Fig. 1).
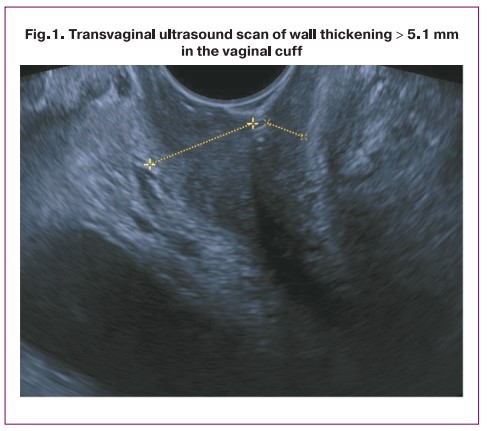
For comparison, transvaginal sonography, with an empty bladder, demonstrated that that average wall thickness in the vaginal cuff was 4.1±0,85 mm and had clearly visible smooth contours.
According to ultrasound examination, local recurrences of CC and UC after surgical treatment were mostly localized in the dome of the vaginal cuff in 30 women (78.9%). In most patients – 31 (81.6%), ultrasound grayscale images demonstrated irregular and blurred contours of the mass, bumpy contours were visualized in 4 (10.5%) women and radiant in 3 (7.8%).
Color Doppler assessment demonstrated vascularization and the presence of diffuse or peripheral hypervascularization in the area of the vaginal cuff and/or in a volumetric mass in the surrounding area. This indicated the presence of malignant transformations of pelvic masses in all cases (100%).
At the same time, in most cases – 30 (73.2%), isolated loci with anatomically maintained course of arteries were found in the unchanged vaginal walls, that indicated normal ultrasound imaging results.
The next step in the evaluation process of the effectiveness of surgical treatment was elastography. Elastograms were obtained in accordance with the above described classification. Local recurrences of CC and UC that were found in most cases – 29 (76.3%), elastography color map represented by blue color (elastotype V). This indicated the pathologic result and high mass density that was specific for malignant process (Fig. 2).
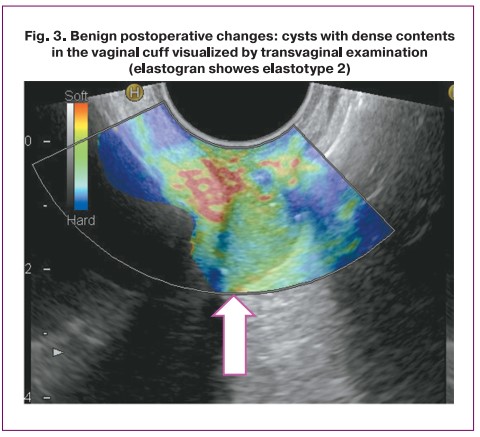
In patients who were in remission, grayscale image of the unchanged vaginal cuff in 22 (73.3%) cases was mapped with green color image, hat indicated elastotype 2 according to the classification.
Stiffness coefficient in recurrences of CC and UC was assessed in 29 (52.1%) cases. At the same time, comparison of stiffness coefficient in the tumor and surrounding tissues showed difference between the numerical values. Accordingly, for tumor tissues with the values of 4.0–5.1 (4.7±0.37) indicated tumors of high density. The sonoelastograpy image showed blue color (elastotype 5).
Postoperative changes, such as cysts with transparent and dense contents, and granulations that thickened wall in the vaginal cuff and were suspected to be a sign of malignancy, always had clearly visible smooth contours and regular shape. Color Doppler imaging did not show vascularization, and elastography image always demonstrated elastotype 2 (Fig. 3). All described ultrasound signs indicated benign volumetric mass, and this was confirmed by cytological examination. Table 3 shows the visualized signs, which were specific for local recurrences and postoperative changes after surgical (complex) treatment.
Visualizing the retroperitoneal space, we suspected, that the lymph nodes detected by us, had specific ultrasound signs of metastasis, such as rounded shape, no division into the cortex and medulla, predominantly hypoechoic structure. We have identified both isolated pathological altered lymph nodes and the nodes that merged forming conglomerates located along the vascular bundles in the retroperitoneal space.
Modified lymph nodes of the size from 0.9 to 7.6 cm were most often located at the level of the first lumbar vertebrae (L1) just to the left of the abdominal aorta and/or in the aortocaval space.
Most often, metastatic pelvic lymph nodes were visualized in the area of bifurcation of the common iliac arteries and were posterior to the external iliac arteries.
We did not obtain additional information using color-coded angiography mode to visualize the blood flow in the retroperitoneal lymph nodes. Also, elastography did not provide additional information to the results of grayscale ultrasound imaging. Probably, this was due to deep lymph node location. Ultrasound diagnosis of metastases was confirmed by histological examination.
In cases of the pronounced malignant process in the pelvic tumor and its penetration into the surrounding tissues, ultrasound examination of the renal pelvicalyceal system showed, that both ureters and renal pelvis were expanded depending on the side of the lesion. Ultrasound imaging created this picture in 10 (9.8%) patients.
Conclusion
Therefore, ultrasound examination, both in grayscale mode and using other advanced ultrasound technologies detected specific ultrasound signs, that were specific for local recurrences of CC and UR in patients after surgical and/or complex treatment. These signs enabled at least to suspect or identify progression of the disease before clinical manifestations and refer the patients for further examination. This certainly increased the survival rate in this category of patients.
In addition to the described signs, we performed a differential diagnosis taking into account the postoperative changes, as well as assessed the normal ultrasound picture of the unchanged wall in the vaginal cuff. This helped the specialists to decrease the rate of false positive results.
With local recurrences of CC and UC thickness of the vaginal cuff increased over 5 mm. At the same time, a hypoechoic solid mass with irregular contours was found, and color Doppler imaging showed hypervascularization.
Elastotype 5 was specific for recurrences. Stiffness coefficient assessed by elastography was 3.5–5.6.
Hypoechoic inclusions (granulations) in the thickened vaginal cuff or volumetric masses (isolated or anechoic) in the adjacent region (cysts with transparent and dense contents ) represented typical postoperative changes. Color Doppler ultrasonography showed avascular changes. Assessment with elastography mode showed that they were mapped as elastotype II, stiffness coefficient was 0.9–1.2.
The unchanged vaginal wall thickness did not exceed 4.6 mm. Isolated vessels were identified using color Doppler imaging mode, that showed elastotype 2, stiffness coefficient 0.9–1.2.
The specific features of regional metastases include rounded shape, hypoechoic structure, impaired differentiation between anatomical layers (the cortex and medulla). When these changes are visualized, it is recommended to clarify diagnostic assessment using an additional imaging technique (magnetic resonance imaging with intravenously administered contrast agents).
Thus, complex dynamic ultrasound monitoring in grayscale mode every 3 months within 2 years after surgical treatment including CDI, EG and elastometry is a reliable way to improve the quality of preclinical diagnosis of local recurrences and regional metastases of cervical and uterine cancers.
References
- Axel E.M. Morbidity and mortality from malignant neoplasms of the female reproductive system in Russia. Oncogynecology. 2015; 1: 8-9. (in Russian).
- Nechushkina V.M., Morkhov K.Yu., Kuznetsov V.V. Surgical treatment of uterine body cancer. Journal of Malignant Tumors. 2014; 3: 72-80. (in Russian).
- Manfredi R., Baltieri S., Tognolini A., Graziani R., Smaniotto D., Cellini N., Bonomo L. Reccurrent uterine cancer after surgery: magnetic resonance imaging patterns and their changes after concomitant chemoradiation. Radiol. Med. 2008; 113(8): 1143-56. https://dx.doi.org/10.1007/s11547-008-0312-3.
- Chissov V.I., Davydov M.I. Oncology. National Guidance. M.: GEOTAR-Media; 2014. (in Russian).
- Kiss M.Z., Hobson M.A., Varghese T., Harter J., Kliewer M.A., Hartenbach E.M., Zagzebski J.A. Frequency-dependent complex modulus of the uterus: preliminary results. Phys. Med. Biol. 2006; 51(15): 3683-95. https://dx.doi.org/10.1088/0031-9155/51/15/006.
- Gazhonova V.E., Belozerova I.S., Vorontsova N.A., Titov D.S. Sonoelastography in the diagnosis of endometrial cancer. Obstetrics and Gynecology. 2014; 1: 54-8. (in Russian).
Received 08.09.2021
Accepted 11.11.2021
About the Authors
Marina A. Chekalova, Dr. Med. Sci., Professor of the Department of Radiology and Ultrasound Diagnostics, Federal Scientific and Clinical Center for Specialized Types of Medical Care and Medical Technologies of the FMBA of Russia, +7(903)199-50-96, ch2me@yandex.ru, 115682, Russia, Moscow, Orekhov Boulevard, 28.Varvara S. Kryazheva, PhD, doctor of ultrasound diagnostics, Loginov MCSC of Moscow Department of Health, branch No. 1, Women's Health Clinic, +7(916)468-71-87, salvaje2005@yandex.ru, 109240, Russia, Moscow, Goncharnaya str., 23.
Authors’ contributions: Chekalova M.A. - the design of the study; Kryazheva V.S. - writing the manuscript, review of publications on the topic of the study.
Conflicts of interest: The authors declare that they have no conflict of interests.
Funding: The study was carried out without any sponsorship.
Patients’ Consent for Publication: The patients have signed informed consent for publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available on request from the corresponding author after approval from the principal investigator.
For citation: Chekalova M.A., Kryazheva V.S. Ultrasound monitoring of the surgical treatment effectiveness in patients with cervical and uterine cancers.
Akusherstvo i Gynecologia/Obstetrics and Gynecology. 2022; 1:107-112 (in Russian)
https://dx.doi.org/10.18565/aig.2022.1.107-112