Ультразвуковое исследование (УЗИ) зарекомендовало себя как эффективный, точный и объективный метод диагностики в акушерстве и гинекологии. Снижение перинатальной смертности в последние годы в значительной степени обусловлено широким внедрением в клиническую практику УЗ-методов оценки состояния плода и связанной с этим ранней диагностикой различных аномалий развития плода, особенностей его функционального состояния и своевременной разработкой тактики ведения беременных. Помимо эхографического определения динамики формирования системы мать-плацента-плод, диагностики пороков развития, детальной оценки анатомии плода с выявлением маркеров хромосомной патологии, допплерометрии кровотока в сосудах маточно-плацентарной системы, в последнее время важным представляется УЗИ в родах, проводимое для решения различных клинических ситуаций [1–4].
В последние годы особую актуальность получило определение положения и позиции плода для прогнозирования исхода родов, формирования клинического несоответствия таза матери и головки плода, возможности применения с благоприятным исходом влагалищных родоразрешающих операций [3, 4]. Традиционно оценка положения и позиции плода проводится с помощью приемов Леопольда и вагинального исследования, которые очень субъективны и зависят от опыта врача [4]. Современные исследования предоставляют информацию о высокой частоте ошибок при определении положения головки плода с помощью вагинального исследования по сравнению с УЗИ [5–9]. По данным литературы, оценка положения головки плода с помощью вагинального исследования была достоверной в 31,28% случаев в первом периоде родов и в 65,7% – во втором [1]. Совпадение результатов оценки положения плода с помощью вагинального исследования с УЗИ составило 35% в первом и 70% – во втором периоде родов [6]. Кроме того, УЗИ и вагинальное исследование одинаково эффективны для оценки степени раскрытия шейки матки [6, 8]. Использование УЗИ в родах позволит повысить точность правильного определения позиции головки плода, а также снизить риск инфицирования, особенно при преждевременном разрыве плодных оболочек [10, 11].
В работе P. Rozenberg et al. [5] было установлено, что для обучения студента определению положения головки с помощью вагинального исследования требуется самостоятельно обследовать 82 пациентки для достижения минимального уровня ошибок, а с помощью трансабдоминального УЗИ – 32.
Согласно рекомендациям Международной организации ультразвуковой диагностики в акушерстве и гинекологии (2018) [4], показаниями для УЗИ в родах являются:
- слабость родовой деятельности или ее прекращение в первом периоде родов;
- слабость родовой деятельности или ее прекращение во втором периоде родов;
- определение положения и предлежания головки плода перед влагалищными родоразрешающими операциями;
- необходимость объективной оценки неправильного предлежания плода.
При УЗИ необходимо оценить следующие параметры [4]:
- жизнеспособность плода и частоту его сердечных сокращений;
- положение (косое, поперечное) и предлежание (головное, тазовое) плода;
- измерение затылочно-позвоночного угла [3];
- наличие плаценты между предлежащей частью и шейкой матки.
Во втором периоде родов необходимо определение дополнительных показателей во время схваток и в паузах между ними (в состоянии покоя), особенно перед влагалищными родоразрешающими операциями:
- угол прогрессии (AoP) – это угол между длинной осью лобкового симфиза и линией, опущенной по касательной от нижнего края симфиза к головке плода;
- направление (вектор) головки плода (HD) относительно лобкового симфиза (рис. 1);
- расстояние между головкой плода и промежностью (HPD) (рис. 2);
- срединный угол (MLA) – это угол между срединной линией головки плода и прямым размером таза женщины (рис. 3) [4].
УЗИ в первом периоде родов
Неправильные положения и предлежания нередко встречаются в современном акушерстве и могут иметь неблагоприятные клинические последствия как для матери, так и для плода. Точное определение положения и предлежания плода важно в первую очередь для выбора оптимального метода родоразрешения [12].
 Ультразвуковые признаки затылочного предлежания при трансабдоминальном сканировании:
Ультразвуковые признаки затылочного предлежания при трансабдоминальном сканировании:
- при переднем виде спереди визуализируются затылочная кость, мозжечок и таламус; сзади – полость прозрачной перегородки, лобная кость, теменная кость, носовая кость, орбиты, глазодвигательные мышцы и хрусталик;
- при поперечном положении стреловидного шва позвоночник и глаза визуализируются латерально (справа или слева), в поперечном размере таза расположены мозжечок, таламус, затылочная и теменная кости [13].
По данным H. Phipps et al. [14], риск кесарева сечения (КС) при поперечном положении стреловидного шва больше, чем при переднем виде затылочного предлежания, но меньше, чем при заднем виде. Так, при переднем виде частота КС составила 5%, при поперечном положении стреловидного шва – 11%, при заднем виде – 28%.
При заднем виде затылочного предлежания спереди визуализируются полость прозрачной перегородки, лобная кость, теменная кость, носовая кость, орбиты, глазодвигательные мышцы и хрусталик; сзади – затылочная кость, мозжечок и таламус [10, 13].
По данным S.K. Choi et al. [15], частота КС при заднем виде затылочного предлежания составляет 37,5%, а при переднем – 8,5% в первом периоде родов. Кроме того, было замечено, что при заднем виде затылочного предлежания, по сравнению с передним видом, выше частота неонатальных осложнений в первом (28,6 и 16,0%) и во втором периодах родов (50,0 и 17,2%).
Разгибательные вставления (переднеголовное, лобное и лицевое) относятся к патологическим вариантам головного предлежания, при которых чаще отмечается развитие клинического несоответствия головки плода и таза матери. Более того, при нормальных размерах плода роды через естественные родовые пути в лобном и заднем виде лицевого предлежания невозможны [16]. Клиническая диагностика разгибательного предлежания и варианта вставления осуществляется при влагалищном исследовании путем определения расположения швов и родничков относительно костей таза, но проведение УЗИ делает диагностику более точной и, соответственно, более точным прогноз исхода родов, что обеспечивает своевременный выбор оптимальной тактики [3, 4, 16].
УЗ-признаки разгибательных предлежаний головки при трансперинеальном сканировании [4, 13]:
- при переднеголовном вставлении возможна визуализация третьего желудочка и мозолистого тела, сосудистые сплетения расположены сзади;
- при лобном вставлении орбиты визуализируются на уровне лобкового симфиза (продольное положение датчика);
- при лицевом вставлении орбиты визуализируются ниже лобкового симфиза (продольное положение датчика).
УЗ-признаками асинклитизма при трансперинеальном сканировании считаются:
- отклонение срединной линии головки плода относительно таза матери кзади (передний асинклитизм) или кпереди (задний асинклитизм);
- визуализация преимущественно передней (передний асинклитизм) или задней (задний асинклитизм) теменной кости [13].
 При латеральном асинклитизме визуализируются асимметричный профиль лица, латеральное скручивание головки плода, сагиттальный шов расположен латерально, но направлен не к лобку или крестцу, а вправо или влево (относительно прямого размера таза) [10, 17].
При латеральном асинклитизме визуализируются асимметричный профиль лица, латеральное скручивание головки плода, сагиттальный шов расположен латерально, но направлен не к лобку или крестцу, а вправо или влево (относительно прямого размера таза) [10, 17].
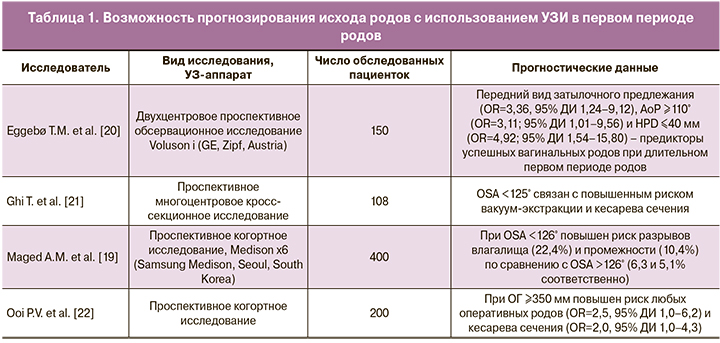
Современные исследования предполагают использование УЗИ для прогнозирования успешных вагинальных родов или большой вероятности КС уже в первом периоде [18–20]. В работе T.M. Eggebø et al. [20] было установлено, что передний вид затылочного предлежания, угол прогрессии (AoP) больше 110° и расстояние между головкой плода и промежностью (HPD) меньше 40 мм являются предикторами успешных вагинальных родов при длительном первом периоде. В исследовании T. Ghi et al. [21] был описан новый УЗ-параметр – затылочно-позвоночный угол (OSA), угол между затылком и шейным отделом позвоночника плода при переднем виде затылочного предлежания, измеряемый трансабдоминально при открытии шейки матки 3-6 см (рис. 4).
Было замечено, что при затылочно-позвоночном угле менее 125° роды чаще заканчиваются оперативно: вакуум-экстракцией плода и операцией КС [21]. Кроме того, в группе с затылочно-позвоночным углом менее 126° повышен риск разрывов влагалища (22,4 и 6,3%) и промежности (10,4 и 5,1%) по сравнению с группой, в которой затылочно-позвоночный угол больше 126° [19]. Следует отметить, что окружность головки плода больше 350 мм в 2,5 раза увеличивает риск любых оперативных родов и в 2 раза – КС из-за дистоции [22]. Возможность прогнозирования исхода родов при использовании ультразвуковой оценки ряда размеров плода и параметров пространственных взаимоотношений головки и таза матери в первом периоде родов представлена в таблице 1.
УЗИ во втором периоде родов
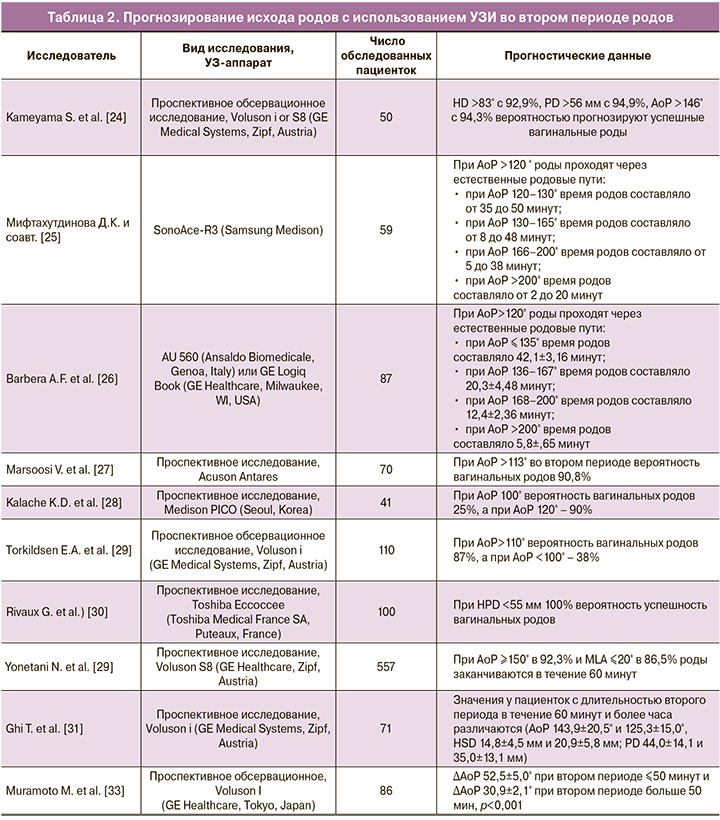
По мнению многих авторов, использование трансперинеального УЗИ во втором периоде родов может помочь в прогнозировании исхода вагинальных родов [23–30]. В исследовании S. Kameyama et al. [24] сообщалось, что направление (вектор) головки (HD) больше 83°, расстояние прогрессии (PD) больше 56 мм и угол прогрессии (AoP) больше 146°, измеренные после полного раскрытия шейки матки, являются предикторами успешных вагинальных родов. По данным Д.К. Мифтахутдиновой и соавт. [25] и A.F. Barbera et al. [26], при угле прогрессии (AoP) больше 120° роды проходят через естественные родовые пути, каждый последующий измеренный угол бывает больше предыдущего, что говорит об успешной динамике родов. При AoP меньше 120° и отсутствии его увеличения в динамике роды через естественные родовые пути невозможны, что указывает на необходимость КС [25]. В исследовании V. Marsoosi et al. [27] сообщалось, что при переднем виде затылочного предлежания и AoP больше 113° во втором периоде родов вероятность вагинальных родов 90,8%. K.D. Kalache et al. [28] установили, что при AoP 100° вероятность вагинальных родов 25%, а при АоР 120° – 90%. По данным другого исследования, при АоР больше 110° вероятность вагинальных родов 87%, а при АоР меньше 100° – лишь 38% [29]. Кроме того, A.M. Dückelmann et al. [23] обнаружили, что достоверность измерения AoP не зависит от положения головки плода или уровня навыков врача ультразвуковой диагностики.
В работе G. Rivaux et al. [30] была продемонстрирована связь между расстоянием от головки плода до промежности (HPD) меньше 55 мм и 100% вероятностью вагинальных родов.
Современные исследования также предполагают использование значения AoP для прогнозирования длительности второго периода родов.
Согласно данным, полученным A.F. Barbera et al. [26]:
- при AoP меньше 135° время родов – 42,1±3,16 минут;
- при AoP 136–167 ° время родов – 20,3±4,48 минут;
- при AoP 168–200° время родов – 12,4±2,36 минут;
- при AoP больше 200° время родов – 5,8±1,65 минут.
По данным Д.К. Мифтахутдиновой и соавт. [25]:
- при AoP 120–130° время родов составляло от 35 до 50 минут;
- при AoP 130–156° время родов составляло от 8 до 48 минут;
- при AoP 166–200° время родов составляло от 5 до 38 минут;
- при AoP больше 200° время родов составляло от 2 до 20 минут.
T. Ghi et al. [31] обнаружили различия показателей (измеренных в начале второго периода родов) у пациенток с длительностью второго периода 60 минут (первая группа) и более 60 минут (вторая группа). AoP составил 143,9±20,5° и 125,3±15,0°, расстояние между головкой плода и симфизом (HSD) 14,8±4,5 мм и 20,9±5,8 мм; расстояние прогрессии (PD) 44,0±14,1 и 35,0±13,1 мм соответственно. В этом исследовании авторами было проведено сравнение тех же данных УЗИ, полученных в начале второго периода родов (T1) и через 40-минутные интервалы после него до родов (T2, T3) у плодов со стабильным задним видом (ЗВ) затылочного предлежания, по сравнению с этими же параметрами при переднем виде (ПВ). При стабильном ЗВ КС было значительно более частым, чем при ПВ (n=5 (50,0%) против n=2 (3,1%), р=0,001). При ЗВ, по сравнению с ПВ, значительно отличались AoP в T1 (122±17° против 138±20°, р=0,016), HD и HSD в T1 (HD 112±17 мм против 86±19 мм, р<0,001; HSD 16,5±5,4 мм против 22,8±6,6 мм, р=0,008) и при T2 (HD 120±16 против 82±27 мм, р=0,008; HSD 12,6±3,4 мм против 18,5±5,4 мм, р=0,038). Таким образом, ультразвуковые параметры являются одними из значимых предикторов длительности активной второй стадии. Кроме того, у плодов в ЗВ по сравнению с теми, которые рождаются в ПВ, опускание головки, по-видимому, отличается на ранних фазах второго периода.
В 2017 г. в исследовании [32], проведенном в Японии с участием 557 женщин, была проанализирована взаимосвязь между значениями AoP и среднего угла (MLA) с продолжительностью второго периода родов. Установлено, что при АоР больше 150° в 92,3% и MLA меньше 20° в 86,5% роды заканчиваются в течение 60 минут. В работе M. Muramoto et al. [33] продемонстрировано, что продолжительность второго периода родов составляла меньше 50 минут при Δ AoP (разница между углами прогрессии, измеренными во время схваток и в покое) 52,5±5,0° и больше 50 минут – при Δ AoP 30,9±2,1°. Полученные различными авторами данные представлены в табл. 2.
По мнению ряда авторов, возможно использование трансперинеального УЗИ для прогнозирования вакуум-экстракции или КС при длительном втором периоде родов [34, 35]. T. Ghi et al. [34] было установлено различие между AoP во втором периоде у группы с вагинальными родами и группы с вакуум-экстракцией и КС в начале второго периода (140,0±20,2° и 122,9±16,7°) и через 20 минут (149,7±20,7° и 126,9±17,5°). По данным A. Youssef et al. [35], HSD больше 17 мм в начале второго периода – предиктор оперативных родов (чувствительность 92,3%).
В последние полвека все чаще используется вакуум-экстракция. Риск неудачных попыток при вакуум-экстракции выше, чем при операции наложения щипцов [36]. Если вакуум-экстракцию провести не удается, то роды заканчивают операцией наложения акушерских щипцов или КС. Оба метода связаны с неблагоприятным материнским и неонатальным исходом, когда выполняются после неудачных попыток вакуум-экстракции. В работе T. Bultez et al. [36] было показано, что AoP больше 145° прогнозирует успешную вакуум-экстракцию. В исследовании J.A. Sainz et al. [37] было установлено, что AoP больше 150° – предиктор успешной вакуум-экстракции, а AoP меньше 105°, PD меньше 25 мм и MLA больше 45° –неудачной. В 2016 г. опубликовано исследование [38], в котором сообщалось, что при расстоянии между бипариетальным размером головки плода и инфрапубикальной линией меньше 1,2 см вероятность успешной влагалищной родоразрешающей операции 90%, а при расстоянии больше 3,3 см вероятность КС – 90%. Чем большая часть головки прошла через инфрапубикальную линию, тем труднее выполнить КС, но выше вероятность успешной родоразрешающей влагалищной операции [38].
В ретроспективном когортном исследовании 635 женщин O. Barak et al. [39] было выявлено, что использование УЗИ во втором периоде родов снижает количество неудачных вакуум-экстракций и частоту операций КС. В группе с использованием УЗИ (US+) не было ни одной неудачной попытки вакуум-экстракции, а в группе без использования УЗИ (US–) – 3,6%. Кроме того, в группе US+ частота КС меньше по сравнению с группой US–(20,2% и 27,8% соответственно). Возраст матери, индекс массы тела, доля первородящих, гестационный возраст при родах и масса тела при рождении, а также краткосрочные исходы у новорожденных существенно не различались между двумя группами. По данным S. Kasbaoui et al. [40], HPD больше 40 мм связано с возникновением сложности вакуум-экстракции.
Также следует отметить, что АоР больше 128° прогнозирует легкую вакуум-экстракцию (количество тракций ≤3) в 85% случаев [41]. Однако если до размещения чашечки вакуум-экстрактора на головке плода АоР меньше 120° при направлении головки горизонтально или вниз, а MLA больше 35°, существует 85% вероятность, что потребуется более 4 тракций [42].
При HPD больше 55 мм в 16,7% случаев наблюдались осложнения при влагалищных родоразрешающих операциях [43].
АоР, измеренный во время схватки, 153,5° и PD во время схватки 58,5 мм прогнозируют осложнения, такие как разрывы промежности 3-й и 4-й степеней, обильное кровотечение во время эпизиотомии, значительные травмы новорожденных в ходе влагалищных родоразрешающих операций [44]. По данным другого исследования, вышеперечисленные осложнения могут наблюдаться при АоР между схватками 138° и при PD 4,8 см в ходе операции наложения акушерских щипцов [45–46] (табл. 3).

Y. Gilboa et al. [47] обнаружили, что визуальная обратная связь с помощью трансперинеального УЗИ во втором периоде родов позволяет увеличить эффективность потуг, снизить риск травматизации промежности. Кроме того, пациентки, у которых роды вели с использованием трансперинеального УЗИ, имели более короткий второй период, по сравнению с женщинами с традиционным ведением (30 минут и 45 минут), и большее увеличение AoP за первые 20 минут (13,5° и 5°) [48].
УЗИ в третьем и раннем послеродовом периодах
Прекращение кровотока между плацентой и миометрием является УЗ-признаком нормального отделения плаценты. Стойкий кровоток между плацентой и миометрием свидетельствует о placenta accreta [49, 50].
В раннем послеродовом периоде положение матки retroversio в 98,3%, структура миометрия гетерогенна в 96,6%, полость матки заполнена эхогенным содержимым в 72,9% наблюдений [50]. Наличие анэхогенного содержимого в полости матки в первые 24 ч после родов при отсутствии аномальных клинических признаков и симптомов считается нормой и не связано с развитием послеродовых кровотечений и инфекционных заболеваний [51–54]. Однако визуализация эхогенного содержимого в матке с размером полости >10 мм свидетельствует о задержке плаценты (чувствительность 93,8% и специфичность 73,9%) [55].
При разрыве матки свободная жидкость визуализируется в брюшной полости; кроме того, наличие свободного внутрибрюшного эхопространства может служить прогностическим маркером разрыва [55].
По данным T. Weissbach et al. [56], УЗИ после операции ручного отделения последа не только не влияло на прогноз, но и увеличивало число ненужных вмешательств, таких как кюретаж, повторное ручное обследование полости матки, утеротоническая терапия.
Заключение
Таким образом, УЗИ позволяет уточнить и дополнить данные, полученные при клиническом обследовании. В первом периоде родов возможны достоверное определение положения и предлежания плода, прогнозирование вагинальных и оперативных родов. Во время потужного периода проводятся оценка динамики и предполагаемой продолжительности второго периода, а также прогнозирование сложностей при вакуум-экстракции и наложении акушерских щипцов. А в третьем и раннем послеродовом периодах УЗИ дает возможность определить потенциальную причину кровотечения и оценить состояние стенок матки при вагинальных родах с рубцом после КС или миомэктомии.




