Clinical significance of diagnostic methods of genital endometriosis
Objective. To determine the clinical significance of methods for diagnosing genital endometriosis.Barinov S.V., Lazareva O.V., Ignatyev Y.T., Poluektov V.L., Mozgovoy S.I., Shamina I.V., Ledovskih O.I., Shkabarnya L.L., Poluektov V.V., Ovchinnikova K.G.
Subjects and methods. The study included 114 patients with external genital endometriosis. All patients were divided into two groups according to the results of surgical treatment. The first group consisted of 65 women without signs of deep infiltrative endometriosis, the second group consisted of 49 patients with deep infiltrative endometriosis. The patients were evaluated with clinical and ultrasound examinations, MRI of the pelvis, colonoscopy, biopsies of rectal mucosa.
Results. The prognostic significance of instrumental methods in the diagnosis of various forms of genital endometriosis was determined. The sensitivity of the ultrasound for identifying endometrial cysts was 83.8% and specificity was 76.7%, the accuracy of the method was 95.4%, a positive predictive value was 91.4%, a negative predictive value was 78.7%; all these indicate that it is a sufficiently informative method. To identify infiltration, the sensitivity of the ultrasound was 16.3% and specificity was 56.6%, the accuracy of the method was 7.01%, a positive predictive value was 100%, the negative predictive value of result was 46.8%. The sensitivity of MRI to identify deep infiltrative endometriosis was 90.9% and specificity was 78.2%, the accuracy of the method amounted 76.9 %, a positive predictive value was 95.6%, the negative predictive value of the result was 78.1%.
Conclusion. The diagnosis of genital endometriosis, especially infiltrative forms requires special training of doctors, which could allow them to determine the degree of damage to the pelvic organs and to plan the adequate amount of surgery.
Keywords
Endometriosis is a gynecological disease which adversely affects the quality of woman’s life and has serious consequences for fertility [1, 2]. Deep infiltrative endometriosis is a severe form of external genital endometriosis causing the impairment of functions of the pelvic organs due to the obliteration of anatomical fields [3, 2].
The methods for preoperative diagnostics of endometriosis are of critical importance as they allow estimating the degree of the damage, planning the extent of surgery, forming diversified surgical teams, especially in deep infiltrative endometriosis.
Ultrasound study is used as a method for first line visualization in suspecting endometriosis [4]. However, the high effectiveness of ultrasonography in diagnosing endometriosis, especially deep infiltrative endometriosis, was reached only by experienced specialists [4, 5]. MRI is more accurate in diagnosing endometriosis, especially deep infiltrative endometriosis [3, 4].
Colonoscopy allows studying the large intestine to identify the degree of its involvement in pathological process and to determine the extent of surgery [6].
Materials and Methods
The analysis of clinical observation of 114 reproductive-aged patients with external genital endometriosis was carried out. The patients were performed a laparoscopic operation in Regional Clinical Hospital, Omsk, in the period from 2016 to 2018.
The inclusion criteria were external genital endometriosis confirmed clinically and morphologically, the age of women from 18 to 45 years old, the absence of cancerous and acute inflammatory diseases. All patients were divided into two groups according to the results of surgical treatment. The first group consisted of 65 women without any signs of deep infiltrative endometriosis, the second one enrolled 49 patients with deep infiltrative endometriosis.
At the stage of planning the operation, all women underwent a clinical evaluation; it included taking the patient’s case history, rectovaginal examination, transvaginal ultrasonography on the apparatus «VolusonTME8/E8 Expert». In most cases patients were admitted to the hospital with the results of the studies performed in the prehospital phase. In suspecting deep infiltrative endometriosis, some patients were conducted a transrectal ultrasonic study, filling the vagina with physiological solution and using Foley catheter.
Magnetic-resonance imaging (MRI) of the pelvis was done using the scanner Achieva 1.5T Nova Dual (Philips) with a surface coil. Half an hour before the study the women had to empty the bladder. All patients were injected intravenous contrast agent Gadovist in dose of 0.1 ml per 1 kg of body weight. The study was performed in sagittal, coronal and axial-dipole array projections obtaining T2 and T1 weighted images; and in saggital projection using impulsive sequence with fat signal suppression.
To estimate the state of the lower colon, there was an endoscopic examination and rectum mucosa biopsy in projection of endometrial infiltrate location with the subsequent morphological study. The study was performed with the help of modern videoendoscopic system of expert class Olympus EVIS EXRA 150 and Olympus EVIS EXERA 180, video colonoscope of high resolution CF-150, CF-180.
The extent of operation was due to the type, the disease localization and reproductive plans of the patient. During the surgical treatment, the stage of localization of pathological process was determined using the classification of American Fertility Society (AFS) [7].
All patients were performed the morphological study with fixed material in 10% buffered formalin according to generally accepted method of staining with hematoxylin and eosin.
Statistical analysis of data was carried out with the help of standard methods of mathematical and statistical processing with the program Statistica 7.0.
Results and Discussion
The indications for performing laparoscopic surgery in 114 patients with external genital endometriosis included infertility, 41 women (35.9%), cystic ovarian endometriosis with diameter 38.6±12.2 mm, 98 women (85.9%), pain syndrome, 63 women (55.3%). The age of the operated women was 32.5±4.2 years. The average duration of the disease was 18.8±6.8 months. The beginning of the disease was determined on the basis of revealing the signs of external genital endometriosis with the instrumental methods or according to the clinical picture of the disease (dysmenorrhea, pelvic pain, dyspareunia).
The most frequent complaint of the patients with the external genital endometriosis was dysmenorrhea in 70 women (61.4%), pelvic pain in 47 women (41.2%), dyspareunia in 25 women (21.9%), menstrual disorders, namely menorrhagia and metrorrhagia, in 22 patients (19.3%).
We have analyzed the results of clinical and instrumental methods of study in the patients from both groups. The indications for performing laparoscopic surgery in the women from the first group were infertility in 24 cases, ovarian endometriotic cysts in 62 cases, and pain syndrome in 21 cases; the latter was characterized by dysmenorrhea, pelvic pain, dyspareunia. Another important point to be made is that the presence of deep infiltrative endometriosis was discovered during the operation.
Indications for performing surgery in the patients of the second group were ovarian endometriotic cysts in 36 cases, infertility in 17 cases, pain syndrome in 42 cases.
Besides a pelvic pain, one patient had blood in feces during the menstruation. A segmental rectal resection was performed.
The average age of the patients of the first group was 33 ± 5.8 years, in the second group it was 32.6 ± 4.3 years.
The characteristics of the clinical indications of the patients of both groups are shown in Table 1.
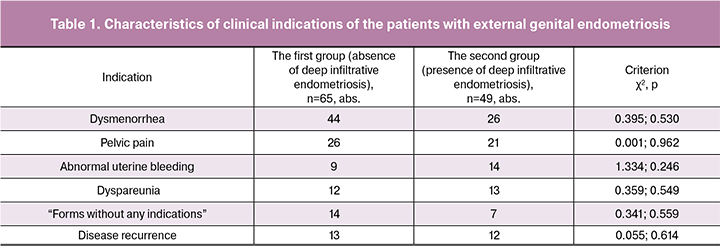
It can be seen from the table that the frequency of occurrence of endometriotic signs was comparable in both groups.
We estimated the duration of the disease in women from both groups. The average duration of the disease in patients without deep infiltrative endometriosis was 11.1±4.5 months, in women with deep infiltrative endometriosis it was 23.7±7.4 months (p=0.160). It was difficult to determine the proper duration of the disease, especially deep infiltrative endometriosis, due to some errors in diagnostic methods, development of clinical manifestations at the advanced stage of the disease.
The recurrence of external genital endometriosis occurred in 13 patients out of 65 from the first group, and in 12 patients out of 49 from the second group. In the first group in nine cases the surgical treatment was the second one, in four cases our surgical treatment was the third operation for ovarian endometriotic cysts. In the second group there were nine patients who had the second operation, and three women who had the third operation. Among twelve patients of the second group only one woman had a recurrence of deep infiltrative endometriosis with sigmoid colon involvement. In other cases of the recurrent forms of the disease, the localization of endometriosis was the ovarian area; for this reason, the initial cystectomy had been performed. There was no clear evidence of infiltrative forms.
This fact is indicative of an actual current problem of surgical treatment of patients with endometriosis. On performing a repeated operation it is difficult to clarify the presence of an infiltrate during the previous surgical treatment that complicates the verification of the underlying or recurrent disease. According to this, it is actual not only to make a detailed description of the operation for endometriosis, but also if it is possible to make a video film of the current surgical treatment. This in turn suggests a qualified training of the surgeon performing the operations of this kind.
Thus, we can say about the recurrent disease in case of presence of ovarian endometriotic cysts only if the ultrasonic study after the previous operation showed the absence of endometriomas.
All patients were performed transvaginal ultrasonography before the operation. We analyzed the frequency of adenomyosis in women of both groups using the ultrasonic study results. In the first group the signs of adenomyosis were revealed in 25 out of 65 cases. In 10 cases the diagnosis suggestive of adenomyosis was made on the basis of asymmetric myometrial walls. According to ultrasonography results, in 24 out of 65 cases there were areas of increased heterogeneous echogenicity of the myometrium. Almost in half cases among the patients of the second group, in 24 out of 49 women, the signs of adenomyosis were revealed on the basis of asymmetric myometrial thickness; it was due to the increase in thickness of one of the uterine walls in 15 out of 49 patients, and due to inhomogeneity of the muscular layer in 19 out of 49 patients. Adenomyosis signs were revealed in all cases of endometriosis infiltrate.
Revealing signs of adenomyosis using the ultrasonography results one may have some difficulties due to the lack of the clear specific criteria and due to subjectivity in interpretation of ultrasonogram. One of the ultrasonic characteristics of adenomyosis is an increase in the size of the transitive zone between the endometrium and myometrium [1].
We did not evaluate the prognostic value of different diagnostic methods of adenomyosis, as the final diagnosis can be made on the basis of the examination of hysterectomy specimens. In our case hysterectomy was not performed. However, literature data and our study show the connection between adenomyosis and deep infiltrative endometriosis [5].
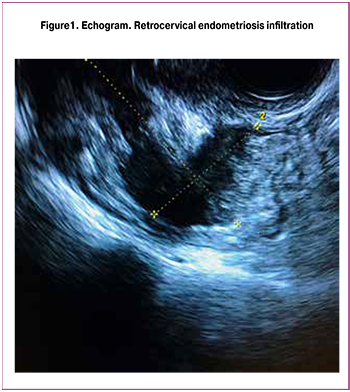 The identification of endometriosis infiltrate on the basis of ultrasonography turned out to be interesting. Only in half cases, in eight out of fourteen women, the presence of infiltrate was revealed using sonography (Fig. 1). It should be noted that seven patients were examined simultaneously by an obstetrician-gynecologist; while according to the preliminary examination of the same patients at the prehospital stage, the signs of infiltrate were not revealed.
The identification of endometriosis infiltrate on the basis of ultrasonography turned out to be interesting. Only in half cases, in eight out of fourteen women, the presence of infiltrate was revealed using sonography (Fig. 1). It should be noted that seven patients were examined simultaneously by an obstetrician-gynecologist; while according to the preliminary examination of the same patients at the prehospital stage, the signs of infiltrate were not revealed.
For diagnosis verification of deep infiltrative endometriosis, a definite experience in diagnosing these forms of the disease is required. It is confirmed by the literature data, according to which the ultrasonography specialist achieves a definite degree of mastership in identifying deep infiltrative endometriosis after minimum 30-40 studies of the this form of the disease [8, 9]. The literature data show that there is no significant difference in using 3D and 4D ultrasonography for diagnosing deep infiltrative endometriosis [10].
Four patients of the second group had the additional transrectal ultrasound study to define the diagnosis of deep infiltrative endometriosis. The given method allows estimating not only the presence of infiltrate, but also the degree of rectum mobility that can be a sign of its involvement in the pathological process.
The standard criterion for calculating the prognostic value of different diagnostic methods was the laparoscopic and anatomy and pathology study results. Calculating the prognostic value of ultrasonography method in the identification of ovarian endometriotic cysts, we obtained the following results: test sensitivity 83.8%, specificity 76.7%, method accuracy 95.4%, predictability of the positive result 91.4%, predictability of the negative result 78.7%. The data show high informativity of the given method for identifying ovarian endometriotic cysts. Using the method in the first phase of the menstrual cycle for the differential diagnostics of endometriomas is of critical importance.
Calculating the prognostic value of ultrasonography in the identification of the infiltration, we obtained the following results in the study: test sensitivity 16.3%, specificity 56.6%, method accuracy 7.01%, predictability of the positive result 100%, predictability of the negative result 46.8%. The ultrasonography method in our study did not have enough prognostic value for revealing endometriosis infiltrate; it confirms the necessity of better training of the ultrasonography specialists to identify different forms of endometriosis disease, especially deep infiltrative endometriosis [8, 9].
In the second group, in eleven cases MRI was performed, in seven cases it was MRI with contrast enhancement of the pelvis. This study was performed with clinical suspicion of deep infiltrative endometriosis. According to MRI results the signs of adenomyosis were revealed in ten patients: asymmetric uterine walls in eight cases, increase in thickness of transition zone in seven cases, diffuse myometrial changes in eleven cases. In seven cases there was an increase in width of the transition zone that is a true sign of endometriosis.
The presence of retrocervical infiltrate was identified in nine patients according to the results of MRI and was confirmed during the operation (Fig. 2). MRI allows estimating the degree of the involvement of the intestines, bladder in the pathological process and the extent of involvement.
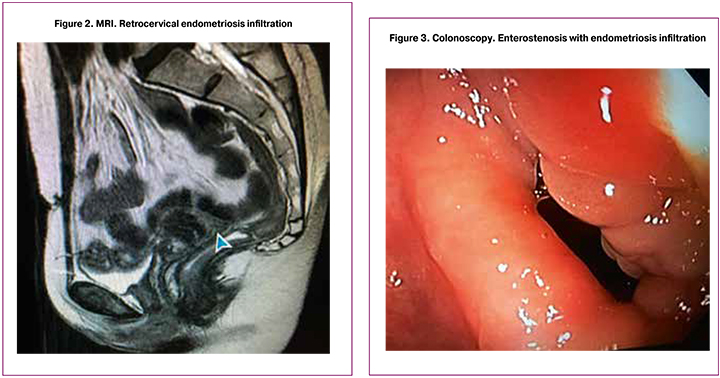
The high accuracy of the diagnostic method is confirmed by most of the studies [11, 6]; therefore, this method is necessary to be implemented when suspecting deep infiltrative endometriosis during the prolonged course of the disease. The sonography is often used as a first-line visual method. However, MRI is more accurate in the identification of the complex disease. MRI is informative in diagnosing deep infiltrative endometriosis; it characterizes the localization of the disease and plays the key role in the planning of the surgical treatment [12, 11].
Defining the prognostic value of the MRI method in revealing the infiltrate, the following results were obtained: test sensitivity 90.9%, specificity 78.2%, method accuracy 76.9%, predictability of the positive result 95.6%, predictability of the negative result 78.1%.
The importance of MRI method is that the obstetrician-gynecologist has an opportunity to estimate the degree of involvement in case of endometriosis disease by analyzing photos or video of the study.
Colonoscopy was performed in ten cases of the patients from the second group. The most frequent sign while performing colonoscopy is the deformation of the front wall of the rectum in the projection of the infiltrate location. It should be noted that in fixed location of uterus in retroposition, what usually occurs in deep infiltrative endometriosis, the deformation of the intestine circuit can be due to the projection of the uterine body. Colonoscopy allows estimating the deformation and the degree of enterostenosis (Fig. 3). Seven patients with deep infiltrative endometriosis were performed colonoscopy. All patients had the change of the front circuit of the rectum in place of infiltration localization. These patients had biopsy of the rectal mucosa. One of the factors for performing the biopsy can be the mobility of intestinal mucosa in comparison with the muscular one while extracting it with the biopsy forceps.
According to anatomy and pathology study, in one case there was medical evidence, namely focal endometriosis, that confirms the data of some authors about endometriosis involvement of the intestine wall which remains visually unchanged [13]. In other cases even involving the intestine wall in pathological process with the significant diminution, the result of the histological assessment was within the normal range. According to the results of the surgical treatment, 65 patients of the first group had ovarian endometriotic cysts and/or peritoneal endometriosis. Both ovaries were affected by endometriosis in 22 out of 65 cases, one ovary was involved in 35 out of 65 cases (24 – left, 22 – right). The average cyst size was 48.9±21.4 mm. In 8 out of 65 cases, patients had peritoneal endometriosis. In 25 out of 65 cases there was a combination of peritoneal endometriosis and ovarian endometriosis.
All patients of the second group had deep infiltrative endometriosis. Sacrouterine ligament involvement was noticed in 29 out of 49 cases. Both ligaments were affected in half of the cases. The intestine was involved in the pathological process in 29 out of 49 cases, but only two women had the involvement of the sigmoid colon, others had the rectum affected. One patient underwent the resection of the rectum due the spread of the process on the muscular coat and enterostenosis by 70–80% (the patient complained of the blood in feces during the menstruation). In other cases, shaving was performed during the operation. In 14 out of 49 cases endometriosis infiltrate with the size from 10 to 50 mm was revealed. The presence of the ovarian endometriotic cysts in 38 out of 49 patients of this group was identified during the operation. In 14 cases the involvement of both ovaries with endometriomas was revealed. The average size of the cysts was 39.1 ± 3.6 mm.
Conclusion
To sum up, while planning the adequate medical tactics and the extent of surgical treatment for patients suggesting deep infiltrative endometriosis, it is necessary to perform the complex of diagnostic measures, such as ultrasonography, MRI, colonoscopy.
The special training of diagnosticians is also of critical importance, especially in the specialized hospitals [14]. This allows determining the level of damage to the pelvic organs from endometrioid disease and planning the adequate extent of surgical treatment by multi-field surgery team.
References
1. Адамян Л.В. Эндометриоз: диагностика, лечение, реабилитация. Клинические рекомендации. М.; 2013. 86с. [Adamyan L.V.Endometriosis: diagnosis, treatment, rehabilitation. Clinical recommendations. Moscow; 2013. 86p. (in Russian)].
2. Попов А.А., Слободянюк Б.А., Мананникова Т.Н., Федоров А.А., Чантурия Т.З., Барто Р.А. Роль ретроцервикального эндометриоза в генезе бесплодия. Клинический случай и обзор литературы. Русский медицинский журнал. 2014; 229140: 1070-1. [Popov A.A., Slobodyanyuk B.A., Manannikova T.N., Fedorov A.A., Chanturia T.Z., Barto R.A. The role of retrocervical endometriosis in genesis of infertility. Case report and literature review. Russian medical journal. 2014 22(14): 1070-1. (in Russian)].
3. Alborzi S., Rasekhi A., Shomali Z., Madadi G., Alborzi M., Kazemi M., Hosseini Nohandani A. Diagnostic accuracy of magnetic resonance imaging, transvaginal, and transrectal ultrasonography in deep infiltrating endometriosis. Medicine (Baltimore). 2018; 97(8): e9536.
4. Bazot M., Daraï E. Diagnosis of deep endometriosis: clinical examination, ultrasonography, magnetic resonance imaging, and other techniques. Fertil. Steril. 2017; 108(6): 886-94.
5. Chapron C., Tosti C., Marcellin L., Bourdon M., Lafay-Pillet M.C., Millischer A.E. et al. Relationship between the magnetic resonance imaging appearance of adenomyosis and endometriosis phenotypes. Hum. Reprod. 2017; 32(7): 1393-401.
6. Perandini A., Perandini S., Montemezzi S., Bonin C., Bellini G., Bergamini V. Defining probabilities of bowel resection in deep endometriosis of the rectum: Prediction with preoperative magnetic resonance imaging. J. Obstet. Gynaecol. Res. 2018; 44(2): 292-7.
7. The American Fertility Society. Classification of endometriosis. Fertil. Steril. 1979; 32(5-6): 633-4.
8. Piessens S., Healey M., Maher P., Tsaltas J., Rombauts L. Can anyone screen for deep infiltrating endometriosis with transvaginal ultrasound? A.N.Z. J. Obstet. Gynecol. 2014; 54(5): 462-8.
9. Eisenberg V.H., Alcazar J.L., Arbib N., Schiff E., Achiron R., Goldenberg M., Soriano D. Applying a statistical method in transvaginal ultrasound training: lessons from the learning curve cumulative summation test (LC-CUSUM) for endometriosis mapping. Gynecol. Surg. 2017; 14(1): 19. doi: 10.1186/s10397-017-1022-4.
10. Guerriero S., Alcázar J.L., Pascual M.A., Ajossa S., Perniciano M., Piras A. et al. Deep infiltrating endometriosis: comparison between 2-dimensional ultrasonography (US), 3-dimensional US, and magnetic resonance imaging. J. Ultrasound Med. 2018; 37(6): 1511-21.
11. Thalluri A.L., Knox S., Nguyen T. MRI findings in deep infiltrating endometriosis: A pictorial essay. J. Med. Imaging Radiat. Oncol. 2017; 61(6): 767-73. doi: 10.1111/1754-9485.12680.
12. Donnez O., Roman H. Choosing the right surgical technique for deep endometriosis: shaving, disc excision, or bowel resection? Fertil. Steril. 2017; 108(6): 931-42. doi: 10.1016/j.fertnstert.2017.09.006.
13. Badescu A., Roman H., Barsan I., Soldea V., Nastasia S., Aziz M. et al. Patterns of bowel invisible microscopic endometriosis reveal the goal of surgery removal of visual lesions only. J. Minim. Invasive Gynecol. 2018; 25(3): 522-7. e9.
14. Daraï E., Bendifallah S., Chabbert-Buffet N., Golfier F. Creation of expert centers on endometriosis. Presse Med. 2017; 46(12, Pt 1): 1218-22.
Received 11.04.2018
Accepted 20.04.2018
About the Authors
Barinov, Sergej V., MD, professor, head of the Department of Obstetrics and Gynecology № 2, Omsk State Medical University of Ministry of health of the Russian Federation.644043, Russia, Omsk, Lenina str. 12. Tel.: +73812240658. E-mail: barinov_omsk@mail.ru
Lazareva, Oksana V., PhD, assistant of the department of obstetrics and gynecology №2, Omsk State Medical University of Ministry of health of the Russian Federation.
644043, Russia, Omsk, Lenina str. 12. Tel.: +73812240658. E-mail: lazow@mail.ru
Ignatyev, Yuri A., MD, professor, head of the Department of Radiodiagnosis, Omsk State Medical University of Ministry of health of the Russian Federation.
644043, Russia, Omsk, Lenina str. 12. Tel.: +73812359324. E-mail: ogma.ray@rambler.ru
Poluektov, Vladimir L., MD, professor, head of the Department of Surgery, Omsk State Medical University of Ministry of health of the Russian Federation.
644043, Russia, Omsk, Lenina str. 12. Tel.: +73812359130. E-mail: 4izzy@mail.ru
Mozgovoy, Sergey I., MD, professor of the Department of Pathological anatomy with the course of clinical pathology, Omsk State Medical University of Ministry of health of the Russian Federation. 644043, Russia, Omsk, Lenina str. 12. Tel.: +73812234830. E-mail: simozgovoy@yandex.ru
Shamina, Inna V., PhD, docent, assistant of professor at the Department of Obstetrics and Gynecology № 2, Omsk State Medical University of Ministry of health of the Russian Federation. 644043, Russia, Omsk, Lenina str. 12. Tel.: +73812240658. E-mail: innadocsever@rambler.ru
Ledovskih, Inna O., doctor of ultrasonic diagnostics of the Department of Reproductive and Perinatal Medicine, Omsk Regional Clinical Hospital.
644011, Russia, Omsk, Beresovaya str. 3. Tel.: +73812251578. E-mail: innaledo@mail.ru
Shkabarnya, Lyudmila L., head of the вepartment of gynecology, Omsk Regional Clinical Hospital.
644011, Russia, Omsk, Beresovaya str. 3. Tel.: +73812251578. E-mail: l_shka@mail.ru
Poluektov, Vladimir V., doctor-proctologist of the Department of Proctology, Omsk Regional Clinical Hospital.
644011, Russia, Omsk, Beresovaya str. 3. Tel.: +73812233337. E-mail: 4izzy@mail.ru
Ovchinnikova, Ksenia G., doctor resident of the department of obstetrics and gynecology №2, Omsk State Medical University of Ministry of health of the Russian Federation.
644043, Russia, Omsk, Lenina str. 12. Tel.: +73821240658. E-mail: ksyu.ov4innikova.90@mail.ru
For citations: Barinov S.V., Lazareva O.V., Ignatyev Y.T., Poluektov V.L., Mozgovoy S.I., Shamina I.V., Ledovskih O.I., Shkabarnya L.L., Poluektov V.V., Ovchinnikova K.G. Clinical significance of diagnostic methods of genital endometriosis. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2018; (12): 75-81. (in Russian)
http://dx.doi.org/10.18565/aig.2018.12.75-81



