Contrast-enhanced ultrasound imaging in the diagnosis of adenomyosis
Objective. To identify the most informative qualitative and quantitative diagnostic criteria for adenomyosis according to the data of transvaginal contrast-enhanced ultrasound (TV CEUS).Sencha A.N., Arakelyan A.S., Bykov A.G., Adamyan L.V.
Materials and methods. Forty-eight patients (a study group) with adenomyosis and 36 women (a control group) with the unchanged myometrium were examined. All the patients underwent TV CEUS using the ultrasound contrast agent (USCA) SonoVue. The investigation was conducted in the V.I. Kulakov National Medical Research Center of Obstetrics, Gynecology, and Perinatology, Ministry of Health of Russia, in 2018–2019.
Results. There were differences in the qualitative parameters of TV CEUS of the myometrium in health and adenomyosis in terms of the intensity and homogeneity of enhancement, the rate and type of contrasting, and the uniformity of USCA washout. The best diagnostic informative value indicators of adenomyosis are heterogeneous contrasting (sensitivity – 100%, specificity – 83.33%, and AUC – 0.917), uneven washout (sensitivity – 85.42%, specificity – 83.33%, and AUC – 0.844), slow accumulation (sensitivity – 81.25%, specificity – 88.89%, and AUC – 0.851), and low contrasting (sensitivity – 72.92%, specificity – 88.89%, and AUC – 0.809). There were differences between the groups in the quantitative parameters of TTR, PI, AT, AS, and DS. With a threshold value of TTP > 19.52 s, sensitivity, specificity, and AUC were 87.0%, 83.3%, and 0.895, respectively; with a threshold value of PI ≤ 36.1 dB, these were 95.7%, 83.3%, and AUC 0.941.
Conclusion. TV CEUS revealed the most informative qualitative and quantitative diagnostic criteria for adenomyosis.
Keywords
Endometriosis is a pathological process characterized by benign growth of tissue beyond the uterine cavity; morphological and functional properties of this tissue are similar to those of the endometrium [1, 2]. In terms of prevalence among gynecological pathologies, endometriosis occupies the third place after inflammatory diseases of the genitals and uterine fibroids. Endometriosis results in structural and functional changes, reduces the quality of life of patients, and it is associated with infertility and early reproductive failure [3]. The search for reliable, available, non-invasive methods of early diagnosis of endometriosis is an important problem of medical imaging. This is due to an increase in the incidence of endometriosis in young patients, as well as the lack of effective methods of conservative therapy [4]. On average, it takes 7.5 years from the onset of the first symptoms to the moment when endometriosis is diagnosed [5]. Adenomyosis, or endometriosis of the uterine body, is the presence of endometrial glands and stroma implanted in the muscle tissue of the body and isthmus of the uterus. There are four forms of adenomyosis: diffuse, focal, nodular and cystic [6]. Depending on the degree of severity of pathological changes, there are four stages of adenomyosis [6]:
- stage I refers to the pathological process limited by the submucosa of the uterine body;
- stage II refers to the pathological process that spreads to the muscle layers;
- stage III refers to the pathologic process that spreads to the entire thickness of the uterine muscle membrane to its serous cover;
- stage IV refers to the pathological process involving parietal peritoneum and pelvic organs in addition to the uterus.
Multiparametric ultrasound imaging is a fast and widely available method for diagnosing diseases of the pelvic organs in women. The most significant sonographic signs of adenomyosis are the increased size and spherical shape of the body of the uterus, and its heterogeneous echostructure. According to meta-analysis performed by Dartmouth K. (2014), sensitivity and specificity of traditional transvaginal ultrasound in the diagnosis of adenomyosis are 57–87% and 60–97%, respectively [7]. Tellum T. et al. (2019) demonstrated that three-dimensional transvaginal ultrasound has better diagnostic characteristics in comparison with traditional transvaginal ultrasound: sensitivity, specificity, and AUC of 2D transvaginal ultrasound were 74%, 76%, 0.700 versus 84%, 84%, and 0.830 of 3D ultrasound, respectively [8]. According to Demidov V.N. et al., the sensitivity of transvaginal ultrasound depends on the form of adenomyosis: 21% in case of focal form, and up to 80% in case of nodular form; its sensitivity also correlates with the severity of adenomyosis, and demonstrates 65.4%, 75.0%, and 90.0% in cases of stage I, II, and III, respectively [9]. Doppler ultrasound assessment of vascularization plays an additional role in the diagnosis of adenomyosis. In order to improve the diagnostic accuracy of ultrasound in adenomyosis, mathematical algorithms are developed for evaluating the results of transvaginal ultrasound [10]. Magnetic resonance imaging is used as a method for clarifying diagnosis and is not recommended for routine diagnosis of endometriosis [6].
Transvaginal contrast-enhanced ultrasound (TV CEUS) has a higher diagnostic accuracy than color flow imaging or power Doppler in the assessment of microvascularization of organs and systems [11]. However, the role of TV CEUS in the diagnosis of diseases of the female reproductive system remains underestimated, understudied, and has certain prospects. According to the EFSUMB Guidelines and Recommendations for the Clinical Practice of Contrast-Enhanced Ultrasound in Non-Hepatic Applications (updated in 2017), there are no recommended gynecological clinical indications for the use of TV CEUS, despite the finding that the absence of any enhancement in ovarian masses corresponds to benign lesions [12]. Nowadays, most of the available studies on the use of TV CEUS in adenomyosis are devoted to the differential diagnosis of adenomyosis and uterine fibroids and the assessment of adenomyosis after ablation [13–15]. There are some individual studies describing the qualitative parameters of contrast enhancement of the uterus in adenomyosis when performing TV CEUS before ablation, but their diagnostic accuracy in adenomyosis has not been evaluated [16].
The aim of the study was to identify the most informative qualitative and quantitative diagnostic criteria for adenomyosis according to the data of transvaginal contrast-enhanced ultrasound.
Materials and methods
The study was performed in the National Medical Research Center for Obstetrics, Gynecology and Perinatology, Moscow, Russia, in 2018–2019. The results of contrast-enhanced transvaginal ultrasound of the uterus with ultrasound contrast agent (USCA) SonoVue (Bracco Swiss SA, Switzerland) were evaluated. The study included 84 patients aged 19–53 years (average age is 6.6 (7.3) years). The main group of the study consisted of 48 patients aged 23-53 years (average age is 37.4 (6.8) years) and diagnosed with adenomyosis; they were operated in the National Medical Research Center for Obstetrics, Gynecology and Perinatology. The diagnosis of adenomyosis was confirmed histologically. The control group consisted of 36 patients aged 19–48 years (average age is 34.5 (8.6) years), who had no myometrial pathology according to the results of additional bimanual examination and MRI. TV CEUS was performed using the Resona-7 and DC-8 ultrasound systems (Mindray, China) with linear multi-frequency probes; operating frequency range was 7.5–15.0 MHz, contrast imaging mode with a low mechanical index (MI<0.10) was chosen. Sulfur hexafluoride agent SonoVue (SonoVue, Bracco, Italy) was used as ultrasound contrast agent which was administered intravenously in a volume of 2.4 ml.
The study included two stages.
At the first stage, all patients underwent multiparametric transvaginal ultrasound assessment using standard 2D echography, color-coded sonography and compression elastography. The state of the myometrial structure was evaluated and interpreted using a combination of echographic characteristics (echogenicity, uniformity, severity of vascularization, stiffness (elasticity)).
At the second stage, TV CEUS was performed according to the uniform principles of asepsis in minimally invasive manipulations, after obtaining the written consent of the patient. The patients were given 4.8 ml of USCA as an intravenous bolus injection into the cubital vein through a peripheral venous catheter 20G, which was followed by the administration of 5 ml of 0.9% NaCl solution. Timing, video recording (at least 120 seconds), and data archiving began simultaneously with the injection of USCA.
In all cases, we evaluated the following characteristics of the contrast enhancement:
- intensity of contrast enhancement (intense, non-intense);
- homogeneity of contrast enhancement (homogeneous, inhomogeneous)
- rate of contrast enhancement (fast, slow);
- type of contrast enhancement (diffuse, radial);
- rate of washing out USCA (fast, slow);
- uniformity of washing out USCA (uniform, uneven).
The quantitative assessment of the contrast enhancement parameters was carried out on the basis of the ratio of the time and intensity of the accumulation and distribution of USCA in the myometrium. The region of interest (ROI) was placed on the zone of the myometrium, the function of motion tracking allowed the ROI to move simultaneously with the area of interest depending on the possible movements of the patient. The time–intensity curves were modeled and analyzed automatically, and the obtained values of quantitative indicators were displayed on the screen in the form of tables.
When the quantitative indicators of TV CEUS were analyzed, the following parameters were evaluated:
- Basic intensity (BI, dB) is the intensity of the reflected signal prior to the administration of the contrast agent;
- Arrival time of contrast (AT, c) is the time of the onset of contrast enhancement in the region of interest;
- Rate of accumulation of contrast enhancement (AS, dB/s) is the rate of increase in the intensity of the reflected signal;
- Time-to-peak (TTP, s) is the time at which contrast concentration reaches its maximum;
- Peak intensity (PI, dB) is the maximum intensity of the reflected echo signal;
- Half-life (DT/2, s) is the time of reducing the contrast enhancement to ½ of the maximum in the region of interest;
- Slow rate of contrast enhancement (DS, dB/s) is the rate of decrease in the intensity of the reflected signal per unit of time.
Mathematical data processing was performed using the programs STATISTICA (Data Analysis Software System, StatSoft, Inc. 2014) version 12.5, MedCalc Statistical Software version 18.2.1 (MedCalc Software bvba, Ostend, Belgium) for Windows.
 Results and discussion
Results and discussion
The patients did not have any adverse reactions and disorders during the study and after it.
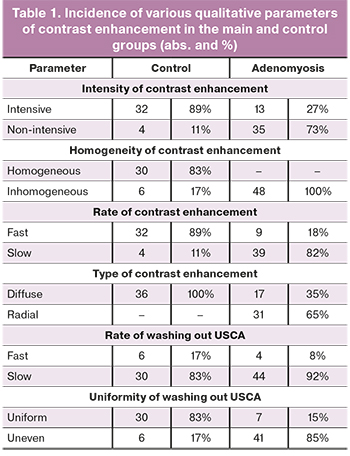
Absolute and relative incidence of various qualitative parameters of contrast enhancement in the main and control groups are presented in Table 1.
There were differences between the main and control groups in terms of intensity, homogeneity, speed, type of contrast enhancement and uniformity of washing out contrast agent. But there were no differences in the speed of washing out the contrast agent from the region of interest.
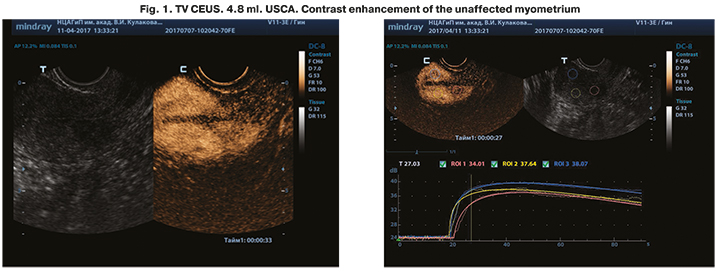
Unaffected myometrium was characterized by intense, rapid homogeneous contrasting in the arterial phase with diffuse filling with contrast and slow uniform washing out the contrast agent in the venous phase. When assessing the dynamics of the intake and distribution of USCA in the myometrium during the review of dynamic fluoroscopic sequences (Fluoro Loop), it was noted that filling of the myometrium with contrast agent occurs from the periphery to the center quite homogeneously (Figure 1). This type of contrasting is due to the characteristics of the uterine blood supply with the formation of an arterial arch on the periphery of the uterus between the leaves of the broad ligament, and the arcuate plexus formed by branches of the uterine artery located in the myometrium and numerous smaller radial arteries which extend deep into the myometrium and continue into the spiral arteries of the inner muscular layer.
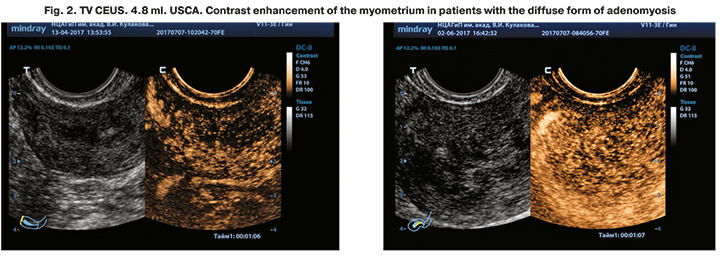
Patients with adenomyosis demonstrated a slower uneven contrast enhancement of the myometrium (due to areas of decreased contrast enhancement and lack of contrast enhancement) in the arterial phase with a radial type of contrast filling of uneven areas and with a slow uneven washing out contrast agent in the venous phase (Figure 2). Contrast enhancement was considered inhomogeneous, even in cases when this uneven contrasting was observed only for a short period of time, and then was replaced by a homogeneous contrasting of the myometrium.
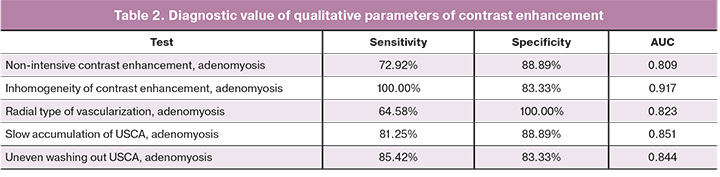
The diagnostic value of each qualitative parameter of contrast enhancement was determined. The results are presented in Table 2.
In order to increase the diagnostic value of TV CEUS, the quantitative parameters of time–intensity curves were evaluated. The values of quantitative indicators in patients with unaffected myometrium and adenomyosis were determined. The results are presented in Tables 3 and 4.
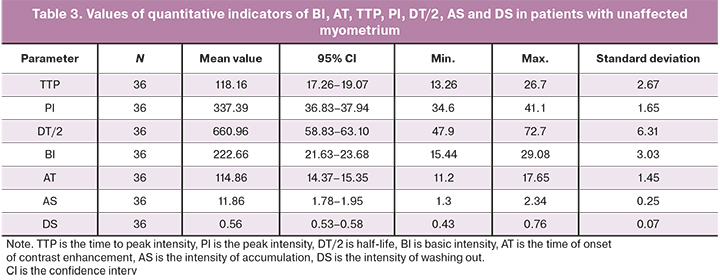
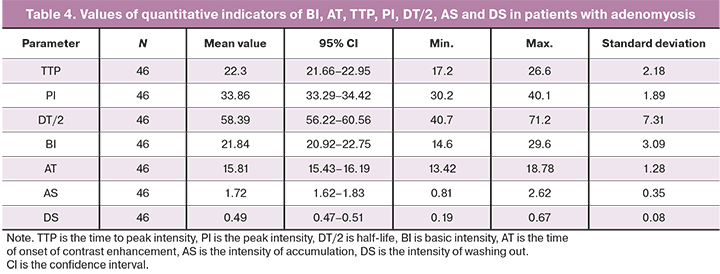
Thus, adenomyosis is characterized by a longer time to peak intensity (TTR, s) and a lower intensity of contrast enhancement (PI, dB), which objectively confirm the results of the analysis of the qualitative characteristics of TV CEUS. There were differences in the decreased rate of contrast enhancement (DS, dB/s) and there were no differences in the half-life of USCA (DT/2, s). This is probably due to the higher peak intensity of contrast enhancement in patients with unaffected myometrium in case of the same basic intensity of the echo signal.
Time to peak intensity (TTP) and peak intensity (PI) were of the greatest importance in the diagnosis of adenomyosis. Such indicators as the time of onset of contrast enhancement (AT), the intensity of accumulation of contrast enhancement (AS) and the rate of decrease of contrast enhancement (DS) were less important.
Threshold values of quantitative indicators of TV CEUS in patients with adenomyosis were revealed (Table 5).
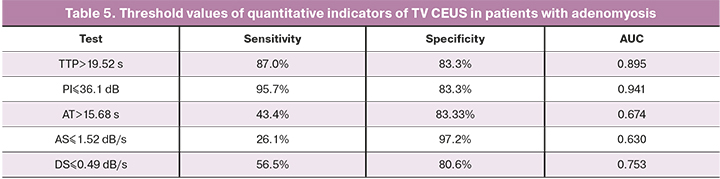
The results of the study showed that the best indicators in the diagnosis of adenomyosis are those that characterize the accumulation of USCA in the pathological focus and in the unaffected myometrium. Slower and less intensive contrast enhancement, both in diffuse and focal forms of adenomyosis, is associated with changes in uterine blood flow. These changes are accompanied by an increase in blood flow resistance along the radial, arcuate and spiral arteries compared to unaffected myometrium [17]. Patients with adenomyosis also have a 1.5–2-fold decrease in the arterial perfusion index compared to healthy controls [17, 18]. Moreover, prolonged hypoxia of the myometrium in adenomyosis contributes to the formation of fibrous tissue. Compact sclerosed areas in the myometrium, in the form of small hyperechoic inclusions, are detected in 65% of patients with adenomyosis. Myometrial cysts are detected in half of patients with adenomyosis, and are a pathognomonic sign of internal endometriosis [18]. Cystic cavities, regardless of their size, do not have contrast enhancement during TV CEUS and, like sclerosed areas, lead to inhomogeneity of contrasting of the myometrium. The findings of the qualitative analysis of TV CEUS were confirmed by the results of quantitative analysis, which demonstrated the highest diagnostic accuracy of TTP and PI indicators; the latter was characterized by high indicators of sensitivity with comparable specificity.
Conclusion
On the basis of the revealed differences in the qualitative and quantitative indicators of TV CEUS, it is possible to state the fact that there are reference points for constructing a differential between unaffected myometrium and adenomyosis. The place of TV CEUS in the diagnostic algorithms for the examination of patients with myometrial pathology is currently not determined. Further studies are necessary to clarify the identified differences.
References
- Адамян Л.В., Андреева Е.Н. Генитальный эндометриоз: клиника, диагностика, лечение. Методические рекомендации. М.; 1997. 31с. [Adamyan L.V., Andreeva E.N. Genital endometriosis: clinic, diagnosis, treatment. Methodological guidelines. M.: 1997. 31 p. (in Russian)].
- Буланов М.Н. Ультразвуковая гинекология. Курс лекций. М.: Видар. 2017; 1. 560с. [Bulanov M.N. Ultrasound gynecology. Lecture course. M.: Vidar. 2017; l. 560 p. (in Russian)].
- Поморцев А.В., Грушевская Ю.В., Макухина Т.Б. Спорные вопросы лучевой диагноcтики аденомиоза при репродуктивных потерях. Кубанский научный медицинский вестник. 2019; 26(2): 173-90. [Pomortsev A.V., Grushevskaya Yu.V., Makukhina T.B. Controversial issues of radiation diagnosis of adenomyosis during reproductive losses. Kuban Scientific Medical Bulletin. 2019; 26(2): 173-90. (in Russian)].
- Адамян Л.В., Сонова М.М., Тихонова Е.С., Зимина Э.В., Антонова С.О. Медицинские и социальные аспекты генитального эндометриоза. Проблемы репродукции. 2011; 17(6): 78-81. [Adamyan L.V., Sonova M.M., Tikhonova E.S., Zimina E.V., Antonova S.O. Medical and social aspects of genital endometriosis. Reproduction problems. 2011; 17(6): 78-81. (in Russian)].
- Endometriosis UK. Annual Report. 2013. Available at: http://endometriosis-uk.org/sites/default/riles/files/Annual-Report-2013.pdf
- Министерство здравоохранения Российской Федерации. Клинические рекомендации. Эндометриоз. МКБ 10: N80. 2020. Available at: https://mosgorzdrav.ru/ru-RU/professional/scientific-activity/clinical.html [Ministry of Health of the Russian Federation. Clinical guidelines. Endometriosis. 2020. Available at: https://mosgorzdrav.ru/ru-RU/professional/scientific-activity/clinical.html. (in Russian)].
- Dartmouth K. A systematic review with meta-analysis: the common sonographic characteristics of adenomyosis. Ultrasound. 2014; 22(3): 148-57. https://dx.doi.org/10.1177/1742271X14528837.
- Tellum T., Nygaard S., Lieng M. Noninvasive diagnosis of adenomyosis: a structured review and meta-analysis of diagnostic accuracy in imaging. J. Minim. Invasive Gynecol. 2020; 27(2): 408-18.e3. https://dx.doi.org/10.1016/j.jmig.2019.11.001.
- Демидов В.Н., Гус А.И. Современные принципы ультразвуковой диагностики генитального эндометриоза (в помощь практическому врачу). Гинекология. 2002; 4(2): 48-52. [Demidov V.N., Gus A.I. Modern principles of ultrasound diagnostics of genital endometriosis (in aid of a practical doctor). Gynecology. 2002; 4(2): 48-52. (in Russian)].
- Поморцев А.В., Лобанов К.А., Зубахин А.Г., Макухина Т.Б. Ультразвуковая диагностика аденомиоза. Кубанский научный медицинский вестник. 2015; 2: 116-22. [Pomortsev A.V., Lobanov K.A., Zubakhin A.G., Makukhina T.B. Ultrasound diagnosis of adenomyosis. Kuban Scientific Medical Bulletin. 2015; 2: 116-22. (in Russian)].
- Сенча А.Н., Могутов М.С., Патрунов Ю.Н., Пеняева Э.И., Кашманова А.В., Сенча Е.А. Ультразвуковое исследование с использованием контрастных препаратов. М.: Видар; 2015. 144 с. [Sencha A.N., Mogutov M.S., Patrunov Yu.N., Penyaeva E.I., Kashmanova A.V., Sencha E.A. Ultrasound using contrast drugs. M.: Vidar; 2015. 144 p. (in Russian)].
- Sidhu P.S., Cantisani V., Dietrich C.F., Gilja O.H., Saftoiu A., Bartels E. et al. The EFSUMB guidelines and recommendations for the clinical practice of Contrast-Enhanced Ultrasound (CEUS) in non-hepatic applications: update 2017 (Long Version). Ultraschall Med. 2018; 39(2): e2-44. https://dx.doi.org/10.1055/a-0586-1107.
- Cheng C.Q., Zhang R.T., Xiong Y., Chen L., Wang J., Huang G.H. et al. Contrast-enhanced ultrasound for evaluation of high-intensity focused ultrasound treatment of benign uterine diseases: retrospective analysis of contrast safety. Medicine (Baltimore). 2015; 94(16): e729. https://dx.doi.org/10.1097/MD.0000000000000729.
- Lou W. OP30.03: Evaluation of effects of ultrasound‐guided radiofrequency ablation on adenomyosis by using contrast enhanced ultrasonography. Ultrasound Obstet. Gynecol. 2016; 48(Suppl. 1): 150-1. https://dx.doi.org/10.1002/uog.16449.
- Serafini G., Prefumo F., Gandolfo N.G., Crocetti L., Gandolfo N.M. OC75: Differential diagnosis of uterine myomas and adenomyosis by color Doppler (CD) and Сontrast‐Enhanced Ultrasound (CEU). Ultrasound Obstet. Gynecol. 2006; 28(4): 380. https://doi.org/10.1002/uog.2935.
- Xu C., Tang Y., Zhao Y., Li Y., Feng Q. Use of contrast-enhanced ultrasound in evaluating the efficacy and application value of microwave ablation for adenomyosis. J. Cancer Res. Ther. 2020; 16(2): 365-71. https://dx.doi.org/10.4103/jcrt.JCRT_769_18.
- Сенча А.Н., ред. Ультразвуковое исследование с применением контрастных препаратов. От простого к сложному. М.: МЕДпресс-информ; 2021. 296с. [Sencha A.N., ed. Ultrasound using contrast drugs. From simple to complex. M.: MEDPress-inform; 2021. ISBN 978-5-00030-862-2. 296 p. (in Russian)].
- Озерская И.А. Эхография в гинекологии. М.: Видар-М; 2020. 704 с. [Ozerskaya I.A. Echography in gynecology. M.: Vidar-M; 2020. 704 p. (in Russian)].
Received 17.12.2020
Accepted 01.06.2021
About the Authors
Alexander N. Sencha, MD, PhD, Head of Radiology Department, Professor at the Department of Obstetrics and Gynecology (Additional Vocational Education), V.I. Kulakov National Medical Research Center of Obstetrics, Gynecology and Perinatology, Ministry of Health of the Russian Federation. Tel.: +7(905)130-52-23.E-mail: asencha@yandex.ru. ORCID: 0000-0002-1188-8872. 117997, Russia, Moscow, Ac. Oparina str., 4.
Alek S. Arakelyan, PhD, Senior Researcher of the Gynecological Department, V.I. Kulakov National Medical Research Center of Obstetrics, Gynecology and Perinatology, Ministry of Health of the Russian Federation. E-mail: а_arakelyan@oparina4.ru. ORCID: 0000-0003-3655-7938. 117997, Russia, Moscow, Ac. Oparina str., 4.
Anatoliy G. Bykov, PhD, obstetrician gynecologist of the Department of Operative Gynecology, V.I. Kulakov National Medical Research Center of Obstetrics, Gynecology and Perinatology, Ministry of Health of the Russian Federation. E-mail: a_bykov@oparina4.ru. ORCID: 0000-0002-0359-9510. 117997, Russia, Moscow, Ac. Oparina str., 4.
Leyla V. Adamyan, Dr. Med. Sci., Academician of the RAS, Professor, Head of the Department of Gynecology, Deputy Director for Science, V.I. Kulakov National Medical Research Center of Obstetrics, Gynecology and Perinatology, Ministry of Health of the Russian Federation. E-mail: Adamyanleila@gmail.com. ORCID: 0000-0002-3253-4512.
117997, Russia, Moscow, Ac. Oparina str., 4.
For citation: Sencha A.N., Arakelyan A.S., Bykov A.G., Adamyan L.V. Contrast-enhanced ultrasound imaging in the diagnosis of adenomyosis.
Аkusherstvo i Ginekologiya/Obstetrics and Gynecology. 2021; 6: 115-121 (in Russian)
https://dx.doi.org/10.18565/aig.2021.6.115-121



