Management strategy for full-term labor complicated by prelabor rupture of membranes and group B streptococcus colonization
Relevance: Group B streptococcus (GBS) is the leading cause of perinatal infections. Despite measures implemented to prevent vertical transmission of GBS from mother to child, not all cases of early neonatal infections caused by GBS have yet been prevented. One of the reasons may be the admission of women to labor with unknown GBS colonization status.Olenev A.S., Konoplyannikov A.G., Vlasov I.S., Stetsyuk O.V.
Objective: To investigate the management of full-term labor complicated by prelabor rupture of membranes (PROM) and GBS colonization.
Materials and methods: The study enrolled 124 pregnant women with PROM and unknown GBS colonization status. Of these, 27/124 pregnant women were tested positive for GBS by real-time PCR. In this study group, only active management of full-term labor with intrapartum antibiotic prophylaxis for early neonatal GBS infection was included. In the remaining 97/124 pregnant women with PROM and negative GBS, two management strategies for full-term labor were used: active (n=39/97) and expectant (n=58/97). Active management approaches were similar in the group with GBS colonization, and expectant management. They consisted of observation of labor progression for 24–72 h and antibiotic prophylaxis of infectious and inflammatory complications when the duration of ruptured membranes reached 18 h. The study analyzed predictors of GBS colonization, pregnancy course characteristics, frequency and nature of labor complications, and perinatal outcomes in the study groups, taking into account the chosen management for full-term labor complicated by PROM.
Results: Labor complicated by PROM in women with GBS colonization is associated with the highest risk of chorioamnionitis, even with intrapartum antibiotic prophylaxis, compared with expectant approach to labor management in GBS-negative women. Nevertheless, despite the high risk of chorioamnionitis in the group with active labor management against the background of GBS colonization, no neonates had early neonatal GBS infection according to clinical and laboratory data.
Conclusion: Active management strategy for full-term labor complicated by PROM and GBS colonization prevents the development of early neonatal GBS infection.
Keywords
According to the literature, the incidence of prelabor rupture of membranes at term ranges from 2.7% to 17% and has no decreasing trend [1].
To date, there are different concepts regarding the etiology of preterm PROM. According to several authors, the most significant factor that increases the risk of PROM is the ascending group B streptococcus (GBS) infection [2–8]. Based on this theory, it is assumed that a decrease in the strength and elasticity of fetal membranes occurs in response to inflammatory changes [9, 10]. This pathology contributes to an increased number of maternal and fetal complications during labor, resulting in an increased incidence of operative delivery, obstetric trauma, postpartum complications, and perinatal infections [1].
According to the Normal Pregnancy Clinical Guidelines, dated February 13, 2020, microbiological screening for GBS antigen should be performed in all women at 35–37 weeks gestation [11]. However, despite the current clinical guidelines, the Moscow City Clinical Hospital No. 24 in Moscow continues to admit pregnant women with PROM and unknown colonization status, which requires the development of an algorithm for treatment in this clinical situation.
This study aimed to investigate the management of term prelabor rupture of membranes (PROM) and GBS colonization.
Materials and methods
The present clinical study was conducted at the Perinatal Center of the City Clinical Hospital No. 24 of the DSM from November 2018 to July 2019. The study analyzed the rate and nature of labor complications in 124 women according to the labor management strategy, as well as their perinatal outcomes.
The study inclusion criteria were term PROM, singleton pregnancy, cephalic presentation, absence of regular labor, and unknown GBS colonization status.
The study exclusion criteria were severe somatic and extragenital pathology of the pregnant woman and absolute indications for surgical delivery (abnormal fetal position and presentation, two or more uterine scars after cesarean section, grade III cervical scar deformity, and intrauterine fetal malformations).
Blood pressure, pulse, and body temperature were measured in pregnant women in the emergency room according to inclusion criteria. Baseline clinical, laboratory and instrumental examinations included full blood count on admission and 18 hours later, an ultrasound examination with determination of the amniotic fluid index (AFI). The clinical diagnosis of PROM was confirmed based on complaints, speculum examination, and amniocentesis to determine amniotic fluid leakage during speculum examination. Cervical ripening was assessed by vaginal examination using a modified Bishop's score. The presence of GBS colonization was diagnosed using the GeneXpert GBS (Cepheid) rapid test, the result of which was evaluated in less than 50 minutes.
The study group consisted of 27/124 pregnant women with PROM and GBS colonization. In this cohort of pregnant women, only active full-term labor with intrapartum antibiotic prophylaxis for early neonatal GBS infection was used. On admission to the delivery room, a single 2 g intravenous ampicillin was given, followed by intravenous administration every 6 hours throughout labor. In women with an allergy to penicillin antibiotics, an alternative regimen was used including cefazolin 2 g administered intravenously once on admission to the delivery room, followed by 1 g intravenously every 8 hours during labor.
Taking into account cervical ripening, active management implied the following algorithm:
- Patients with a ripe cervix according to the modified Bishop cervical maturity score of 6 or more points, underwent medically induced labor with oxytocin in the absence of spontaneous labor after 6 hours from the moment of PROM;
- If the cervix was considered unripe according to the modified Bishop's score (0–5 points), 200 mg of oral mifepristone was administered on admission to the delivery room and 6 hours later in the absence of labor activity.
The control group consisted of 97/124 pregnant women with PROM and a negative rapid GBS test. This cohort of pregnant women was managed using an active or expectant management strategy for full-term labor. Active management of full-term labor was similar to that of the study group and was used in 39/97 pregnant women. The remaining 58/97 pregnant women underwent expectant management. The expected approach consisted of observation of labor progression for 24–72 h and antibiotic prophylaxis of infectious and inflammatory complications when the duration of the ruptured membranes reached 18 h. Informed consent to choose active or expectant management for the term PROM was signed by each pregnant woman.
During labor, dynamic fetal and maternal monitoring was performed. Pulse, blood pressure, body temperature, uterine activity, cervical opening, and fetal progression through the birth canal were assessed. The labor was performed under continuous cardiac monitoring and was displayed in the form of a graph on a partogram.
At birth, the newborn's condition was assessed using the Apgar score and blood acid-base balance. Newborns at risk for intrauterine infection were examined by bacteriological blood culture to detect GBS.
Statistical analysis
Statistical analysis was performed using Statistica Version 12.0 software, StatSoft (USA) and MedCalc Version 19.1.7, Softwa (Belgium). The normality of the distribution was tested by the Shapiro–Wilk test. Quantitative variables that show normal distribution were expressed as means (M) and standard deviation (SD) and presented as M (SD); otherwise, medians (Me) with interquartile range (Q1; Q3) were reported. Categorical variables were presented as counts and percentages. Continuous variables were compared with a nonparametric Mann–Whitney test. Pearson's χ2 test was used to compare categorical variables. The Fisher exact test was used when the expected frequency of one or more cells was less than five. When the expected frequencies were between 5 and 10, Yates' correction was used. Differences were considered significant at p<0.05.
Results and discussion
We found that 21.8% (27/124) of the patients tested positive for GBS by PCR. Taking into account the objective of the study, the rate and nature of birth complications depending on the labor management strategy were analyzed in the study groups. The analysis of birth complications is presented in Table 1.
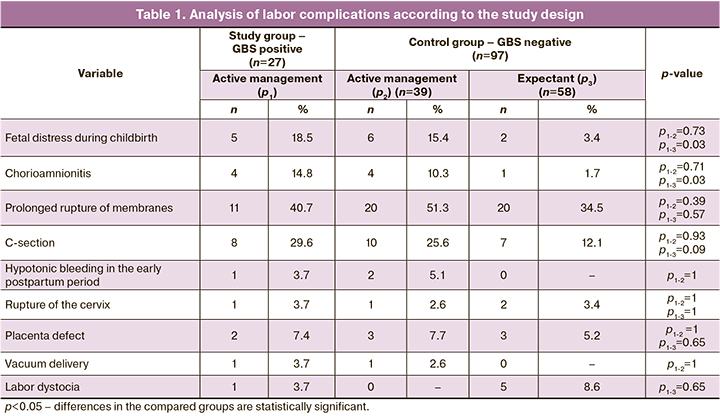
The clinical analysis of the course of labor revealed that the highest incidence of chorioamnionitis was registered in the group with active labor management against the backdrop of GBS colonization, which was 14.8% (4/27). This figure was statistically significant compared to the control group with the choice of mode of labor (14.8% (4/27) and 1.7% (1/58), p1-3=0.03) and statistically insignificant compared to the control group with active labor management (14.8% (4/27) and 10.3% (4/39), p1-2=0.71). Manifestations of acute fetal hypoxia expressed as changes in amniotic fluid or cardiotocographic parameters were statistically significant in the analysis compared with the GBS-negative group and the expectant management, which was 18.5% (5/27) versus 3.4% (2/58), p1-3=0.03. When comparing the study group to the control group with active labor management, the difference in the rate of fetal distress was statistically insignificant, which was 18.5% (5/27) versus 15.4% (6/39), p1-2=0.73.
The incidence of labor dystocia in the study group with active labor management was half of that in the control group patients who underwent expectant management, but the difference was not statistically significant (3.7% (1/27) and 8.6% (5/58), p1-3=0.65).
According to the findings presented in Table 1, the group of GBS positive women undergoing active labor management had the highest percentage of cesarean deliveries, which was 29.6% (8/27). This rate was not statistically significantly different from the control group regardless of the labor management strategy (29.6% (8/27) versus 25.6% (10/39), p1-3=0.93) and (29.6% (8/27) versus 12.1% (7/58), p1-3=0.09).
Differences in early postpartum complications, such as cervical rupture, placental defect, and hypotonic bleeding, were not statistically significant.
To assess the quality of labor management and according to the objective to improve perinatal outcomes in the group with active labor management tactics in GBS positive women, a comparative analysis was performed according to the study design; the data are presented in Table 2.
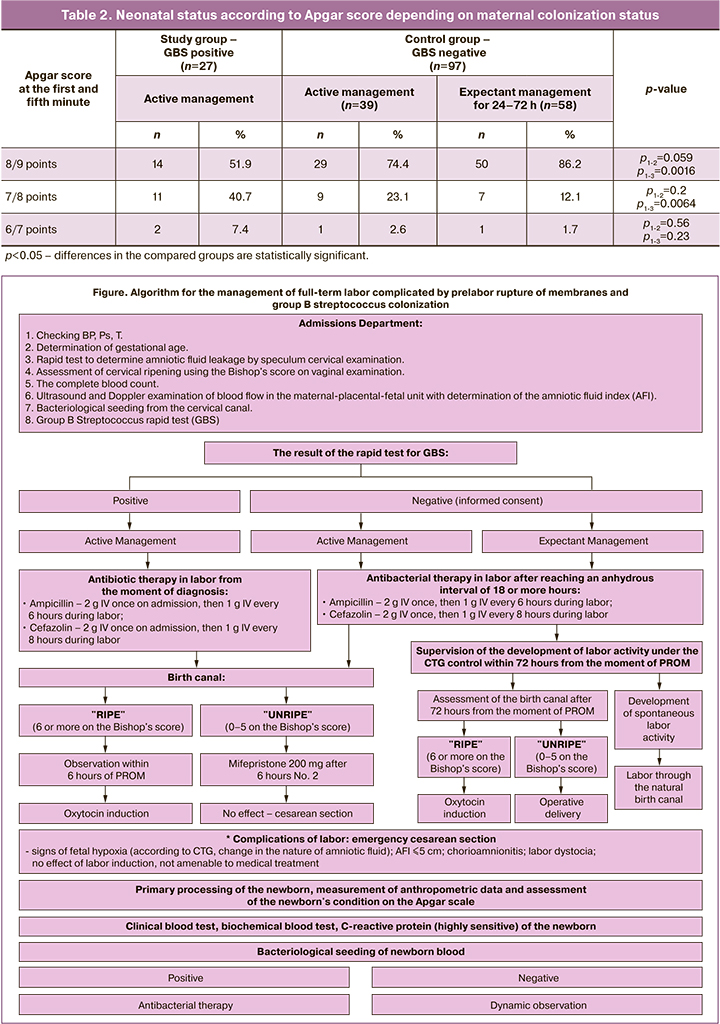
The analysis showed that the newborns were born full-term, with a birth weight of 2570 to 4250 g and body length ranging from 49 to 55 cm. There was statistically significant difference in Apgar scores of 8 and 9 points, respectively, in the GBS positive group undergoing active labor management compared to the control group with expectant labor management in 24–72 hours, which was 51.9% (14/27) compared to 86.2% (50/58), p1-3=0.0016. However, when comparing active labor management in both groups with and without GBS colonization, perinatal outcomes were not statistically significant (51.9% (14/27) versus 74.4% (29/39), p1-2=0.59.
In the early neonatal period, 8.9% (11/124) of the newborns had grade II jaundice, 7.3% (9/124) of the newborns registered toxic erythema, and 0.8% (1/124) of the newborns developed dacryocystitis concurrently with congenital nasolacrimal pathology. According to clinical and laboratory data, none of the neonates developed early neonatal GBS infection. Bacteriological blood tests in the study risk group for fetal intrauterine GBS infection in all neonates diagnosed with negative blood cultures for GBS. The neonates were discharged on the 3rd–5th day without complications.
Conclusions
1. The incidence of GBS colonization in pregnant women with PROM and unknown colonization status according to the clinical study is 21.8% (27/124).
2. PROM-complicated labor in women with GBS colonization carries the highest risk of chorioamnionitis even with intrapartum antibiotic prophylaxis, compared to expectant labor management in women with negative GBS status.
3. Expectant labor management in GBS-negative women with PROM reduces the risk of acute fetal hypoxia during labor.
4. The developed active management strategy (Figure) of full-term labor complicated by PROM and GBS colonization prevents the development of early neonatal GBS infection.
References
- Болотских В.М., Рухляда Н.Н., Афанасьева М.Х. Преждевременное излитие околоплодных вод: этиология, патогенез, диагностика, тактика ведения беременности и родов, прогнозирование. СПб.: Эко-Вектор; 2019. 32с. [Bolotskikh V.M., Rukhlyada N.N., Afanas'eva M.Kh. Premature rupture of amniotic fluid: etiology, pathogenesis, diagnosis, management of pregnancy and childbirth, prognosis. Eco-Vector. 2019: 32. (in Russian)].
- Князева Т.П. Причины и факторы риска преждевременного разрыва плодных оболочек. Дальневосточный медицинский журнал. 2016; 2: 128-35. [Knyazeva T.P. Causes and risk factors for premature rupture of membranes. Far Eastern Medical Journal. 2016; 2: 128-35. (in Russian)].
- Тошева И.И., Ихтиярова Г.А. Исходы беременности при преждевременном разрыве плодных оболочек. РМЖ. Мать и дитя. 2020; 3(1): 16-9. [Tosheva I.I., Ikhtiyarova G.A. Pregnancy outcomes in premature rupture of membranes. RMJ. Mother and child. 2020; 3(1): 16-9. (in Russian)]https://dx.doi.org/10.32364/2618-8430-2020-3-1-16-19.
- Обоскалова Т.А., Максимяк О.В. Преждевременный разрыв плодных оболочек в доношенном сроке беременности. Российский вестник акушера-гинеколога. 2021; 21(1): 54-60. [Oboskalova T.A., Maksimyak O.V. Premature rupture of membranes in full-term pregnancy. Russian Bulletin of the Obstetrician-Gynecologist. 2021; 21(1): 54-60. (in Russian)]. https://dx.doi.org/10.17116/rosakush20212101154.
- Prevention of group B Streptococcal early-onset disease in newborns: Committee opinion number 797. Obstet. Gynecol. 2020; 135(2): e51-e72. https://dx.doi.org/10.1097/AOG.0000000000003668.
- Fullston E.F., Doyle M.J., Higgins M.F., Knowles S.J. Clinical impact of rapid polymerase chain reaction (PCR) test for group B Streptococcus (GBS) in term women with ruptured membranes. Ir. J. Med. Sci. 2019; 188(4):1269-74.https://dx.doi.org/10.1007/s11845-019-01977-x.
- Vornhagen J., Waldorf K.A., Rajagopal L. Perinatal Group B Streptococcal infections: virulence factors, immunity, and prevention strategies. Trends Microbiol. 2017; 25(11): 919-31. https://dx.doi.org/10.1016/j.tim.2017.05.013.
- Wang M., Keighley C., Watts M., Plymoth M., McGee T.M. Preventing Early-Onset Group B Streptococcus neonatal infection and reducing antibiotic exposure using a rapid PCR test in term prelabour rupture of membranes. Aust. N. Z. J. Obstet. Gynaecol. 2020; 60(5): 753-9. https://dx.doi.org/10.1111/ajo.13159.
- Vanderhoeven J.P., Bierle C.J., Kapur R.P., McAdams R.M., Beyer R.P., Bammler T.K. et al. Group B Streptococcal infection of the choriodecidua induces dysfunction of the cytokeratin network in amniotic epithelium: a pathway to membrane weakening. PLoS Pathog. 2015; 10(3): e1003920.https://dx.doi.org/10.1371/journal.ppat.1003920.
- Weed S., Armistead B., Coleman M., Liggit H.D., Johnson B., Tsai J. et al. MicroRNA signature of epithelial-mesenchymal transition in Group B Streptococcal infection of the placental chorioamniotic membranes. J. Infect. Dis. 2020; 222(10): 1713-22. https://dx.doi.org/10.1093/infdis/jiaa280.
- Министерство здравоохранения Российской Федерации. Клинические рекомендации. Нормальная беременность. М.; 2020. 80с. [Ministry of Health of the Russian Federation. Clinical guidelines. Normal pregnancy. M.; 2020. 80 p. (in Russian)].
Received 18.05.2022
Accepted 14.06.2022
About the Authors
Anton S. Olenev, PhD, Deputy Chief Physician, Head of Perinatal Center – Branch of City Clinical Hospital No. 24; Head Specialist in Obstetrics and Gynecology,Moscow City Healthcare Department, OlenevAS@zdrav.mos.ru, https://orcid.org/0000-0001-9632-6731, 127287, Russia, Moscow, 4th Vyatsky lane, 39.
Aleksandr G. Konopliannikov, Dr. Med. Sci., Professor, Department of Obstetrics and Gynecology, Faculty of Pediatrics, Pirogov Russian National Research Medical University, Ministry of Health of Russia, konoplyannikov@yandex.ru, https://orcid.org/0000-0001-9923-8833, 117997, Russia, Moscow, Ostrovityanova str., 1.
Igor S. Vlasov, Head of the Organizational and Methodological Department for Obstetrics and Gynecology, Research Institute for Health Organization and Medical Management, Moscow City Health Department, VlasovIS@zdrav.mos.ru, https://orcid.org/0000-0002-8233-2759, 115184, Russia, Moscow, Bolshaya Tatarskaya str., 30.
Olga V. Stetsyuk, MD, Clinical Resident, Department of Obstetrics and Gynecology, Faculty of Medicine, Pirogov Russian National Research Medical University,
Ministry of Health of Russia, stetsyuko@list.ru, https://orcid.org/0000-0001-8600-7112, 117997, Russia, Moscow, Ostrovityanova str., 1.
Authors' contributions: Olenev A.S. – conception and design of the study, data collection and analysis, manuscript drafting; Konoplyannikov A.G. – conception and design of the study, data collection and analysis, manuscript drafting; Vlasov I.S. – data collection and analysis, manuscript drafting; Stetsyuk O.V. – data acquisition and statistical analysis, review of the relevant literature, manuscript drafting.
Conflicts of interest: The authors have no conflicts of interest to declare.
Funding: There was no funding for this study.
Ethical Approval: The study was reviewed and approved by the Research Ethics Committee of the Pirogov RNRMU,
Ministry of Health of Russia.
Patient Consent for Publication: All patients provided informed consent for the publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available on request from the corresponding author after approval from the principal investigator.
For citation: Olenev A.S., Konoplyannikov A.G., Vlasov I.S., Stetsyuk O.V.
Management strategy for full-term labor complicated by prelabor rupture
of membranes and group B streptococcus colonization.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2022; 7: 43-49 (in Russian)
https://dx.doi.org/10.18565/aig.2022.7.43-49