A strategy to reduce the recurrence rate of vaginal candidiasis in women with weakened immunity
Objective. To investigate the clinical efficacy of triazole antifungal agents in the treatment of recurrent vulvovaginal candidiasis.Khashukoeva A.Z., Agaeva Z.A., Agaeva M.I.
Material and methods. The study comprised 40 patients aged from 33 to 50 years, who were treated at the gynecology department for various diseases of the reproductive system and underwent clinical and laboratory examination. The study group included 30 patients with exacerbation of chronic recurrent vulvovaginal candidiasis (HRVVC). Ten patients without clinical and laboratory evidence of candidal infection were enrolled in the control group. Diagnostic evaluation included a standard clinical examination, bacterioscopic, bacteriological and immunological investigations of the genital tract discharge, determination of the levels of pro- and anti-inflammatory cytokines in cervical secretions and phagocytic activity of neutrophils as one of the indicators of local immunity. Patients in the study group received systemic antimycotic therapy concurrently with an immunobiological agent modulating the immune system.
Results. All patients in the study group reported a significant improvement in the subjective symptoms. At baseline, the leukocyte phagocytic activity of the cervical secretion in the patient with HRVVC was lower than that among the patients in the control group. After the treatment, the patients in the study group were found to have a 61.2% increase in the phagocytic activity (p < 0.05) and a significant decrease in the concentration of pro-inflammatory cytokines compared with baseline levels.
Conclusion. Systemic antimycotic therapy administered concurrently with immunomodulatory agents not only produces an etiotropic effect aimed at the eradication of the pathogen but also helps maintain the post-treatment activity of immunocompetent cells.
Keywords
Fungi of the genus Candida are the leading cause of urogenital infections, especially among women. Currently, vulvovaginal candidiasis (VVC) is the most common condition encountered in obstetric and gynecological practice, with increasing incidence rates of both acute and recurrent forms of the disease [1]. In recent years, the problem of chronic recurrent VVC has attracted increasing attention of obstetrician-gynecologists; according to various authors, the annual incidence of more than four recurrences of VVC is 10–20% [2, 3]. An estimated 50% of women with chronic recurrent VVC experience recurrence in the range from several days to 3 months after successful treatment of a VVC episode [4]. Currently, there are 196 known species of Candida, of which 27 can cause human infections [1]. Over the past ten years, the incidence of VVC has more than doubled. Candida albicans is the most common human fungal pathogen constituting 60-95% of all cases [2, 3]. Despite being a part of the normal vaginal microflora, the candidal infection can transform into a highly pathogenic organism causing pathological conditions, disorders of the vaginal microbiocenosis and impair local immunity of the female genital organs. Despite past and ongoing research, the exact cause of the emergence of recurrent forms of chronic VVC is not fully understood because recurrence may occur in women who do not have well-known risk factors that contribute to an exacerbation of the disease [4].
Taking into consideration currently accumulated data about the mechanisms of resistance to Candida infection, researchers investigating chronic recurrent VVC have been increasingly focused on the functioning and regulation of local immunity subsystems, in particular on the mucosal immunity [1, 5–8]. Based on this, a reasonable approach is the use of immunotropic agents in treatment regimens for chronic recurrent VVC [9, 10]. However, attempts to include some immunotropic agents in the comprehensive management of chronic recurrent VVC therapeutic measures, though being somewhat effective did not completely solve the problem [1, 5]. This lack of effectiveness may be attributed to insufficient administration of these agents, the diversity and ambiguity of concepts about immune reactions of the mucous membranes in Candida-associated infections [6, 7]. At the same time, taking into account the capabilities of some drugs to interact at the level of subpopulations of immunoregulatory cells, it may be possible to identify treatments for chronic recurrent VVC, aimed, on the one hand, at the most complete microbiological reorganization, and on the other - at normalizing local immunoreactivity of the cells of vaginal biotope. The drug of choice for etiotropic therapy of VVC is fluconazole. Diflucan, which was originally synthesized by the Pfizer laboratory, is a new subclass of synthetic triazole antifungal agent containing the active ingredient fluconazole. Considering that the dominant causative agent of VVC is C. albicans, Diflucan has been widely used in the management of this fungal infection. Thus, Diflucan is an original drug in the treatment of VVC [3, 8, 9].
This study aimed to investigate the clinical efficacy of triazole antifungal agent Diflucan in the treatment of recurrent VVC.
Material and methods
The study comprised 40 patients aged from 33 to 50 years, who were treated at the gynecology department for various diseases of the reproductive system and underwent clinical and laboratory examination. The study group included 30 patients with exacerbation of chronic recurrent VVC. Ten patients without clinical and laboratory evidence of candidal infection were enrolled in the control group. Diagnostic evaluation included a standard clinical examination, bacterioscopic, bacteriological and immunological investigations of the genital tract discharge, and determination of the levels of pro- and anti-inflammatory cytokines. Cytokines profile, including interleukins 4 (IL-4), tumor necrosis factor –α (TNF-α) and interferon gamma (IFN-γ) in cervical mucus was determined by enzyme immunoassay using the Cytokine reagent kit. The neutrophil phagocytic activity was assessed in a test with Staphylococcus aureus live culture; phagocytic index and the phagocytic number of neutrophils were calculated by V.M. Berman and E.M. Slavskoy. All patients in the study group received systemic antimycotic therapy with Diflucan 150 mg single dose, followed by a course of anti-relapse therapy (Diflucan 150 mg once weekly for 4-6 months). Concurrently with the fungicidal agent, all patients of the study group were administered vaginal suppositories of a combined immunobiological preparation kipferon (1 suppository twice daily for 10 days). Patients in the study group were subjected to three culture and microscopic examinations of the genital tract discharge (at baseline, at 14 days and 6 months after the initiation of therapy). Concentrations of pro- and anti-inflammatory cytokines and the analysis of the neutrophil phagocytic activity in cervical secretion in patients of the study group were carried out before starting therapy and 6 months after that.
Statistical analysis was performed using Statistica 8.0 statistical software with the calculation of the arithmetic mean (M), median (M) standard deviation (SD), and confidence interval (CI) for the difference of parametric variables. Differences between the groups were considered statistically significant at p < 0.05.
Results
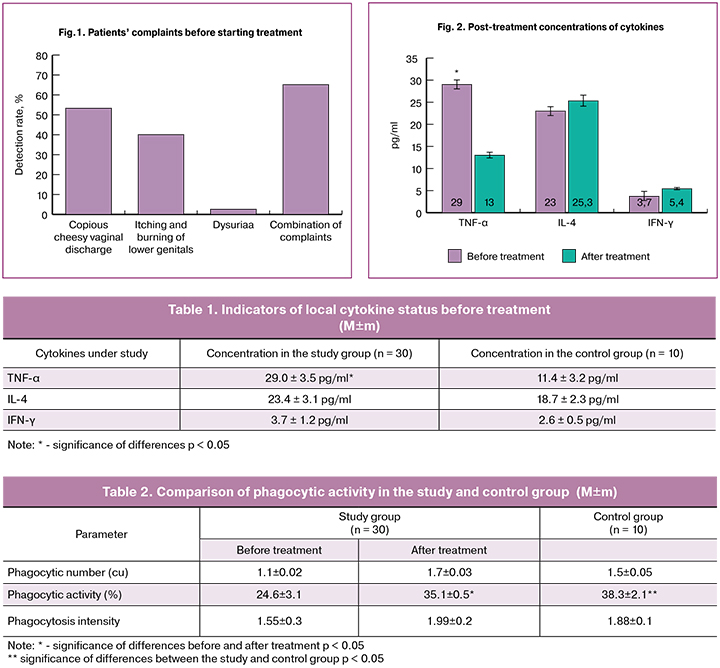
At baseline, patients in the study group reported copious vaginal discharge (n = 16; 53.3%), itching and burning of the external genital organs (n=12; 40.0%), and dysuria (n = 2; 6.6%). Most patients had a combination of several complaints (Fig. 1). Patients in the control group did not have these complaints.
Analysis of complaints during the treatment course showed that by the 4th day of combination therapy 28 (93.3%) patients reported a significant improvement in the subjective symptoms, manifested by a decrease in the amount of vaginal discharge and a decrease in the intensity of genital itching and burning. At the gynecological examination on the 4th day from the start of therapy, slight hyperemia of the labia majora remained only in 2 (6.6%) patients of the study group, while before treatment vulvar and vaginal hyperemia and edema was observed in 76.6% of patients (p < 0.05).
Microbiological examination of the vaginal discharge detected Candida fungi in all patients in the study group while no patients in the control group had this infection. Analysis of species composition of yeast fungi in patients of the study group showed that Candida albicans fungi were VVC causative agents in 25 (83.3%) patients and Candida glabranta in 5 (16.7%) patients.
Analysis of cellular factors of the vaginal secretion showed that at baseline patients with exacerbation of chronic recurrent VVC had significantly higher leukocyte count than patients in the control group (17.1 ± 0.1 vs. 6.6 ± 2.0 WBC per HPF, respectively; p < 0.05). At baseline, neutrophil phagocytic activity and intensity in vaginal secretion was lower among patients in the study group compared with that in the control group (24.1 ± 0.5% vs. 35.4 ± 2.3%, respectively; p < 0.05).
Analysis of local cytokine status at baseline showed that compared with the control group patients with exacerbation of chronic recurrent VVC had a significantly higher levels of pro-inflammatory cytokine TNF-α (p <0.05) and pro-inflammatory IFN-γ in cervical mucus though this difference was not statistically significant (Table 1).
Patients in the study group were found to have an imbalance between anti-inflammatory and pro-inflammatory cytokines with the predominance of the latter. Increased production of pro-inflammatory cytokines is one of the factors of the nonspecific defense of the mucous membranes of the reproductive organs and reflects the activation of the local humoral immunity.
The findings of microbiological examination at day 14 days after treatment initiation revealed that elimination of yeast-like fungi from vaginal discharge was achieved in 29 women (96.7%). Candida albicans were re-isolated from one patient (3.3%) at a low concentration (103 CFU/ml). At the same time, Candida albicans was detected only by culture, while vaginal smear microscopy was within normal range.
At clinical and microbiological follow-up at 6 months after starting the treatment, the disease recurrence was observed in 1 (3.3%) patient. The patients reported that clinical manifestations of the disease recurrence were associated with acute respiratory viral infections. VVC recurrence was confirmed clinically and microbiologically. Identification of the causative agents showed that the recurrence was caused by Candida albicans.
Follow-up examination of cellular factors in vaginal secretion in the course of treatment showed a significant decrease in the leukocyte count to 10.3 ± 3.1 WBC per HPF compared with baseline (p < 0.05). At the second follow-up visit, the phagocytic number in patients of the study group doubled, while in the control group it showed a 1.3 fold increase (Table 2; p < 0.05).
At baseline, the functional activity of vaginal secretion neutrophils in patients with chronic recurrent VVC was lower than the phagocytic activity and intensity in the control group. However, at 6 months from the start of treatment, as presented in Table 2, there was a significant increase in phagocytic activity in the patients of the study group (p < 0.05). Also, the treatment resulted in a tendency to an increase in the phagocytic intensity and phagocytic number, which indicates the important role of the local immunity in the formation of recurrent VVC.
Analysis of changes in cytokine concentration at the local level at 6 months follow-up established a significant decrease in the concentration of pro-inflammatory cytokine TNF-α in a cervical secretion that co-occurred with a slight increase in IFN-γ concentration (Fig. 2)
Treatment of chronic VVC recurrence contributed to the relief of a local inflammatory reaction by reducing the production of pro-inflammatory cytokine TNF-α. It is noteworthy that the concentration IFN-γ in the cervical secretion, which is the main protective factor of mucous membranes, on the contrary, tended to increase, which can be considered a favorable factor in preventing VVC recurrence.
Conclusion
Systemic antimycotic therapy with Diflucan administered concurrently with immunomodulatory agents not only produces an etiotropic effect aimed at the eradication of the pathogen but also helps maintain the post-treatment activity of immunocompetent cells. It should also be noted that during the follow-up period, no treatment-related adverse effects were observed, which makes it possible to recommend the antimycotic agent Diflucan in combination with immunomodulatory drugs in the management of chronic recurrent VVC.
References
1. Байрамова Г.Р., Баранов И.И., Припутневич Т.В., Чернова В.Ф. Вульвовагинальный кандидоз: клинические и терапевтические аспекты в практике акушера-гинеколога. Акушерство и гинекология: новости, мнения, обучение. 2017; 4: 63-9. [Bayramova G.R., Baranov I.I., Priputnevich T.V., Chernova V.F. Vulvovaginal candidiasis: clinical and therapeutic aspects in the practice of an obstetrician-gynecologist. Obstetrics and gynecology: news, opinions, training. 2017; 4: 63-9. (in Russian)]
2. Абакарова П.Р., Прилепская В.Н., Межевитинова Е.А., Байрамова Г.Р., Иванова Е.В. Современные возможности эффективного лечения вульвовагинального кандидоза. Акушерство и гинекология. 2012; 7: 84-6. [Abakarova P.R., Prilepskaya V.N., Mezhevitinova E.A., Bayramova G.R., Ivanova E.V. Modern possibilities of effective treatment of vulvovaginal candidiasis. Obstetrics and gynecology. 2012; 7: 84-6. (in Russian)]
3. Бурменская О.В., Байрамова Г.Р., Непша О.С., Трофимов Д.Ю., Муллабаева С.М., Донников А.Е., Екимов А.Н. Состояние локального иммунитета при хроническом рецидивирующем вульвовагинальном кандидозе. Акушерство и гинекология. 2011; 1: 52-6. [Burmenskaya O.V., Bayramova G. R., Nepsha, O. S., Trofimov D. Yu., Mullabaeva S.M., Donnikov A.E., Ekimov A.N. The state of local immunity in chronic recurrent vulvovaginal candidiasis. Obstetrics and gynecology. 2011; 1: 52-6. (in Russian)]
4. Прилепская В.Н., Мирзабалаева А.К., Кира Е.Ф., Гомберг М.А., Аполихина И.А., Байрамова Г.Р. Федеральные клинические рекомендации. Диагностика и лечение заболеваний, сопровождающихся патологическими выделениями и половых путей женщин. М.: Российское общество акушеров-гинекологов; 2013. [Prilepskaya V.N., Mirzabalaeva A.K., Kira E.F., Gomberg M.A., Apolikhina I.A., Bayramova G.R. Federal clinical guidelines. Diagnosis and treatment of diseases involving pathological secretions and genital tract of women. M .: Russian Society of Obstetricians and Gynecologists; 2013. (in Russian)]
5. Савченко Т.Н., Точиева М.Х., Агаева М.И., Дергачева И., Шмарина Г.В., Кофиади И.А. Цитокиновый статус у женщин с невынашиванием беременности и сопуствующей кандидозной инфекцией. Лечение и профилактика. 2015; 2: 24-7. [Savchenko T.N., Tochieva M.Kh., Agaeva M.I., Dergacheva I., Shmarina G.V., Kofiadi I.A. Cytokine status in women with miscarriage and co-candidal infection. Treatment and prevention. 2015; 2: 24-7. (in Russian)]
6. Frobenius W., Bogdan C. Diagnostic value of vaginal discharge, wet mount and vaginal pH – an update on the basics of gynecologic infectiology. Geburtshilfe Frauenheilkd. 2015; 75(4): 355-66.
7. Workowski K.A., Bolan G.A.; Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm. Rep. 2015; 64(RR-03): 1-137.
8. Goldenberg R.L., Culhane J.F., Iams J.D. Epidemiology and causes of preterm birth. Lancet. 2008; 371(9606): 75-84.
9. Серов В.Н., Тютюнник В.Л. Вульвовагинальный кандидоз: особенности течения и принципы лечения. Фарматека. 2015; 15: 38-43. [Serov V.N., Tyutyunnik V.L. Vulvovaginal candidiasis: features of the course and treatment principles. Farmateka. 2015; 15: 38-43. (in Russian)]
Received 11.07.2018
Accepted 21.09.2018
About the Authors
Khashukoeva, Asiyat Z., MD, professor of the Department of Obstetrics and Gynecology, Faculty of Medicine, Pirogov Russian National Research Medical University.117997, Moscow, Ostrovityanova str. 1. Tel.: +79163403813. E-mail: azk05@mail.ru
Agaeva, Zoya A., MD, associate professor of the Department of Ultrasound Methods of research and mini-invasive methods of treatment using ultrasound, N.V. Sklifosovsky Research Institute of Emergency Medicine. 129090, Russia, Moscow, B. Sukharevskaya Square str. 3, bldg. 21. Tel.: +79528225656. E-mail: zoya466@mail.ru
Agaeva, Madina I., postgraduate student of the Department of Obstetrics and Gynecology, Faculty of Medicine, Pirogov Russian National Research Medical University.
117997, Russia, Moscow, Ostrovityanova str. 1. Tel.: +79260818170. E-mail: madlen1690@mail.ru
For citation: Khashukoeva A.Z., Agaeva Z.A., Agaeva M.I. A strategy to reduce the recurrence rate of vaginal candidiasis in women with weakened immunity. Akusherstvo i Ginekologiya/ Obstetrics and Gynecology. 2018; (12): 88-92. (in Russian)
https://dx.doi.org/10.18565/aig.2018.12. 88-92



