Патология прикрепления плаценты является одной из наиболее сложных и нерешенных проблем акушерства, ассоциированной с самыми тяжелыми жизнеугрожающими ситуациями, увеличивающими перинатальные и материнские риски заболеваемости и смертности [1, 2]. Известны три морфологические формы нарушения инвазии ворсин хориона: их приращение к миометрию – placenta accreta, прорастание мышечной оболочки – placenta increta, а при достижении серозного слоя или даже соседних органов – placenta percreta. В последние годы прослеживается тенденция к значительному увеличению частоты данного заболевания на основании мировых данных с 1960 года по настоящее время: с 1 на 93 000 беременностей до 1 случая на 322, что составляет почти 300-кратное увеличение за 5 десятилетий [3]. Так, в Российской Федерации в 90-е годы частота кесарева сечения по стране приближалась к 13% всех родоразрешений, а уже через 20 лет в 2015 году данный показатель вырос двукратно до 27,5%. Децидуализация области рубца в нижнем маточном сегменте или в шейке матки в сочетании с другим фактором риска – предлежанием плаценты значительно увеличивает риск врастания плаценты [4].
Основными диагностическими методами являются ультразвуковое исследование (УЗИ) и магнитно-резонансная томография (МРТ) органов малого таза, которые имеют схожую чувствительность и специфичность и хорошо дополняют друг друга для более детальной оценки патологии в дооперационном периоде. Существуют два основных подхода, реализуемых при родоразрешении данных пациенток: выполнение одномоментной или отсроченной гистерэктомии и более прогрессивная тактика – выполнение органосохраняющего лечения. Последняя подразумевает выполнение метропластики, при которой иссекается участок стенки матки с вросшей плацентой, и требует применения особых методик, минимизирующих кровопотерю в ходе ее выполнения. Экстирпация матки дискредитирует функцию репродуктивной системы и тазового дна, что связано с локальным изменением кровотока, иннервации и лимфодренажа, приводящих к развитию полисистемных синдромов. Имеется противоречивый опыт применения эндоваскулярных методов остановки кровоснабжения матки на различных уровнях во время оперативного родоразрешения. При этом лишь единичные работы являлись рандомизированными, выполненными в соответствии с критериями классического клинического исследования. Наиболее изучена в этом смысле остановка кровоснабжения по руслу внутренней подвздошной артерии (ВПА). В работе 2017 года Yoon Jin с соавт. проводили профилактическое билатеральное введение катетера в ВПА, в результате чего авторам удалось добиться снижения кровопотери до 1950 мл, гистерэктомия была выполнена в 3 из 18 случаев [5]. Однако существующие анастомозы сосудов матки мобилизуют поиск более оптимального уровня окклюзии, одним из которых является общая подвздошная артерия (ОПА). Одно из немногих исследований, придерживающихся органосохраняющей тактики, было выполнено в 2016 году Sinan Al-Hadethi на сравнительно большой выборке (по 25 человек в основной и контрольной группах). Авторам не удалось выявить статистически значимого различия у пациенток, которым проводилось баллонирование ОПА по сравнению с контрольной группой. Средняя кровопотеря в исследуемой группе составила 2455 (±1444) мл, а частота гистерэктомии – 64% [6]. Катетеризация сопровождалось у двух пациенток серьезными осложнениями: тромбозом и повреждением стенки крупных артерий. Предлагающиеся методы рентгено-интервенционных эндоваскулярных технологий требуют специального дорогостоящего оборудования, а также соответствующего профиля и квалификации врачей, способных выполнить данный этап.
В настоящем исследовании проведена оценка различных методов хирургического гемостаза без применения специального оборудования с сохранением прочих аспектов протокола операции неизменными в каждом случае. Поиск оптимальных способов и подходов определил цель настоящей работы.
Цель исследования: оценить результаты применения различных методов хирургического гемостаза (перевязки ВПА, временной окклюзии ОПА и комплексного компрессионного гемостаза) во время кесарева сечения у пациенток с врастанием плаценты.
Материал и методы исследования
С января 2015 года по июнь 2017 года были родоразрешены 56 беременных с диагнозом врастание плаценты, подписавших информированное согласие на участие в контролируемом клиническом исследовании, в котором были разъяснены все риски, связанные с ходом операции и послеродового периода. Все пациенты были предварительно обследованы посредством 2D и 3D УЗИ, а также путем МРТ-диагностики. Подобная комбинация методов является наиболее оправданной и позволяет более детально оценить синтопию органов, степень и площадь врастания, а также вовлеченность соседних тканей в патологический процесс.
Для оценки эффективности методов хирургического гемостаза во время кесарева сечения были выделены три группы в зависимости от выполненной методики остановки кровоснабжения. Критерии включения: женщины со сроком гестации 28–38 недель с морфологически верифицированным врастанием плаценты. Первую группу составили 17 пациенток, которым было выполнено кесарево сечение, метропластика с билатеральной перевязкой ВПА. Однако два случая были исключены из исследования: в одном – ввиду развившегося кровотечения с последующим экстренным родоразрешением; в другом имело место существенное изменение хода операции.
Во второй группе (n=18) был выполнен схожий протокол, однако точкой гемостаза являлись ОПА, на которые были наложены сосудистые зажимы Сатинского. Предварительно профилактически вводится 2500 ЕД гепарина, фиксируется время пережатия таким образом, чтобы время остановки кровоснабжения по сосудам не превышало 40 минут. Данная методика выполнялась под контролем сатурации нижних конечностей посредством пульсоксиметра, датчик которого крепится на ногтевой фаланге большого пальца стопы слева и справа. Непосредственно сразу после окончания операции производится ультразвуковая допплерография вен нижних конечностей.
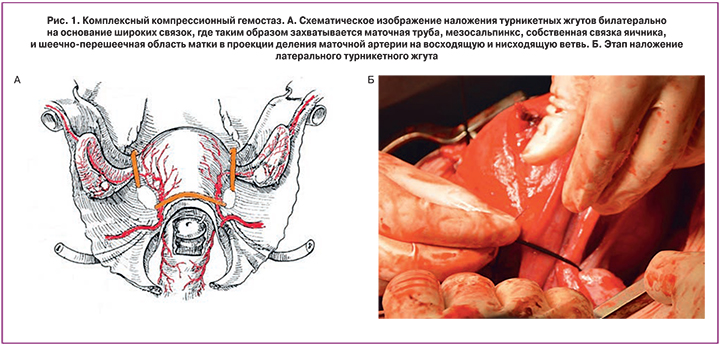
Третью группу составила 21 пациентка, которой был выполнен комплексный компрессионный гемостаз, включающий наложение турникетных жгутов билатерально на основание широких связок и шеечно-перешеечную область, дополненный управляемой баллонной тампонадой матки. В широких связках матки, на уровне перешейка формируются «окна» слева и справа, через которые накладываются турникетные жгуты, после чего затягиваются и фиксируются двумя зажимами. Яичники отводятся латеральнее турникетов, таким образом, в петлю попадают маточная труба, мезосальпинкс, собственная связка яичника, за счет чего пережимаются трубные ветви и коммуниканты, связывающие яичниковую и маточную артерии (рис. 1). Через эти же окна вокруг шейки проводится 3-й турникет, фиксируется зажимом на уровне шейки. Стоит подчеркнуть, что после выполнения основного оперативного этапа все наложенные турникетные жгуты снимаются. Дополнительно всем пациенткам данной группы перед окончательным ушиванием матки выполнялась ретроградная профилактическая управляемая внутриматочная баллонная тампонада матки.
Эффективность лечения оценивалась по следующим критериям: общему объему кровопотери, числу гистерэктомий, объему инфузионно-трансфузионной терапии, изменению уровня гемоглобина, длительности пребывания в стационаре после родоразрешения, времени операции.
Основной этап операции проходит в условиях развернутого аутогемотрансфузиологического обеспечения и включает выполнение стандартной нижнесрединной лапаротомии с последующим донным кесаревым сечением. После извлечения плода пересекается пуповина и ушивается полость матки. Следующим этапом рассекается брюшина пузырно-маточной складки, мочевой пузырь низводится с прицельной коагуляцией сосудов, обнажается передняя поверхность шейки матки. Шейка матки с целью маркировки границ здоровых тканей прошивается викриловой нитью 1/0 П-образным швом на всю ширину в передне-заднем направлении. Концы нитей фиксируются зажимом. Затем выполняется один из методов хирургического гемостаза. Далее производилось иссечение стенки матки в зоне врастания плаценты, с последующим извлечением плаценты из полости матки и ушивание дефекта двурядным швом, включающим П-образный и непрерывный, с последующей перитонизацией.
Консервативный подход при кровопотере включал выполнение инфузионной и трансфузионной терапии с применением свежезамороженной плазмы, эритроцитарной массы, препаратов VII фактора свертывания крови, ингибиторов фибринолиза, утеротоников. В послеоперационном периоде пациенткам всех групп проводилась антибиотикопрофилактика амоксициллином в комбинации с клавуланатом калия и назначались низкомолекулярные гепарины.
Статистическая обработка данных выполнялась на индивидуальном компьютере с помощью электронных таблиц Microsoft Excel и пaкета статистических программ Statistica V10 (США), SPSS Statistics 22 (США) и SAS V8 (США). Для проведения нормального распределения использовали критерии Колмогорова–Смирнова и Шапиро–Уилка. При нормальном виде распределения данных определяли среднее значение со стандартным отклонением, для оценки различий в группах применяли методы параметрической статистики (t-тест для сравнения данных в 2 группах, для множественного сравнения нескольких групп определялся критерий Стьюдента с поправкой Бонферрони и ANOVA). Для описания распределений, не являющихся нормальными, применяли медиану и перцентили (Me (25%; 75%)). Сравнения количественных и порядковых переменных проводили с применением непараматрических критериев Краскела–Уоллиса, Манна–Уитни (U), Уилкоксона (W). Для сравнения категориальных данных в двух и более группах, а также для оценки значимых различий между ними использовали тест χ2. Тест χ2 проводили после построения таблиц сопряженности.
Исследование одобрено этическим комитетом ФГБУ НЦАГиП им. акад. В.И. Кулакова Минздрава России.
Результаты исследования
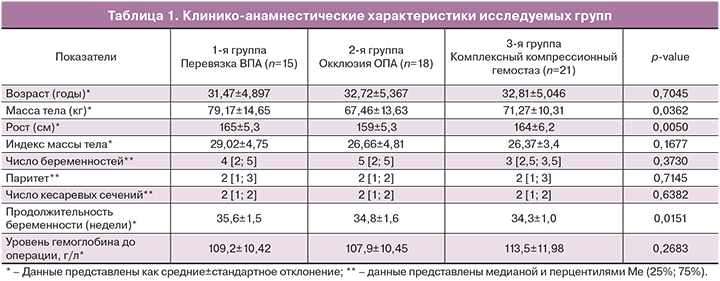
 При оценке клинико-анамнестических характеристик не было выявлено статистически значимых различий по демографическому, акушерскому и соматическому анамнезу, за исключением продолжительности беременности между 1-й (35,6±1,5 недель) и 3-й группой (34,3±1,0 недель) (р=0,0122). При анализе антропометрических данных было выявлено различие в показателях веса в 1-й (79,17±14,65 кг) и во 2-й группе (67,46±13,63 кг) (р=0,0299), а также ростового показателя 165±5,3 см, 159±5,3 см, 164±6,2 см в 1-й, 2-й и 3-й группах соответственно (р=0,0050) (табл. 1). Социально-экономические характеристики (уровень образования, семейное положение, наличие или отсутствие работы) не различались в исследуемых группах. Анализ гемоглобина до операции также не имел статистически значимого различия (в 1-й группе – 109,2±10,42 г/л, во 2-й группе – 107,9±10,45 г/л, в 3-й группе – 113,5±11,98 г/л).
При оценке клинико-анамнестических характеристик не было выявлено статистически значимых различий по демографическому, акушерскому и соматическому анамнезу, за исключением продолжительности беременности между 1-й (35,6±1,5 недель) и 3-й группой (34,3±1,0 недель) (р=0,0122). При анализе антропометрических данных было выявлено различие в показателях веса в 1-й (79,17±14,65 кг) и во 2-й группе (67,46±13,63 кг) (р=0,0299), а также ростового показателя 165±5,3 см, 159±5,3 см, 164±6,2 см в 1-й, 2-й и 3-й группах соответственно (р=0,0050) (табл. 1). Социально-экономические характеристики (уровень образования, семейное положение, наличие или отсутствие работы) не различались в исследуемых группах. Анализ гемоглобина до операции также не имел статистически значимого различия (в 1-й группе – 109,2±10,42 г/л, во 2-й группе – 107,9±10,45 г/л, в 3-й группе – 113,5±11,98 г/л).
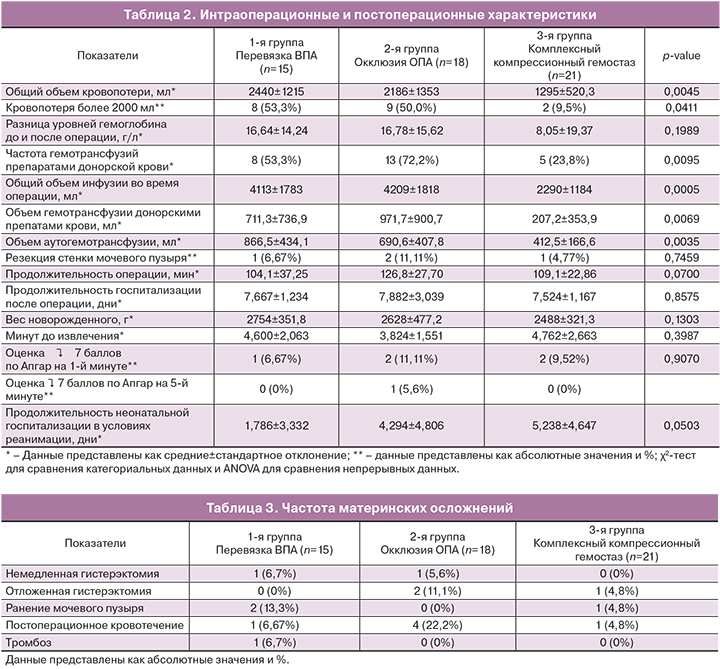
В соответствии с использованными в настоящей работе критериями эффективности наиболее выраженный гемостатический эффект получен в 4-й группе (табл. 2). Общий объем кровопотери у женщин 1-й группы был наибольшим и составил 2440±1215 мл, во 2-й группе – 2186±1353 мл и значительно меньшим оказался в 3-й группе – 1295±520,3 мл (р=0,0045) (рис. 2). Причем при попарном сравнении хирургических методов определяется достоверная разница между 1-й и 3-й группами (р=0,0071), а также 2-й и 3-й группами (р=0,0347), что подтверждает эффективность комплексного компрессионного гемостаза. Более того, в последней группе наблюдалось значительное снижение частоты массивных кровопотерь более 2000 мл (2 случая – 9,5%) в то время как в двух других – имело место более чем у половины пациенток (р=0,0411). Подобный гемостатический эффект безусловно отражался на связанных с кровопотерей характеристиках: снижение объема общей инфузии до 2290±1184 мл, а также инфузии собственными и донорскими препаратами крови (412,5±166,6 и 207,2±353,9 мл соответственно) при комплексном компрессионном гемостазе по сравнению с остановкой кровоснабжения как по руслу ВПА, так и по ОПА.
В клиническом анализе крови в 3-й группе наблюдалась наименьшая разница уровней гемоглобина до и после операции, однако значение достоверности не позволили подтвердить гипотезу о неслучайности подобных изменений (р=0,1989). Продолжительность операции также статистически не различалась во всех группах и была сопоставима, однако у пациенток, которым выполнялась временная окклюзия ОПА, время хирургического вмешательства было несколько больше, что можно объяснить технически более сложным этапом выделения ОПА. Среднее время пережатия данных сосудов составило 24,2±8,2 минуты (р=0,20). Резекция мочевого пузыря в одном случае выполнялась в 1-й и 3-й группах, в двух – при проведении окклюзии ОПА. Проведение данного этапа объяснялось интимным сращением истонченной стенки матки с серозой мочевого пузыря, при котором атравматическая отсепаровка последнего не представлялась возможной. Анализ других интраоперационных характеристик, таких как продолжительность госпитализации, вес новорожденного и оценка по шкале Апгар, длительность пребывания в условиях детской реанимации не показали какого-либо статистически значимого различия.
Частота гистерэктомий не различалась в группах (р=0,7723) и составила 6,7, 16,7 и 4,8% соответственно в 1-й, 2-й и 3-й группах (табл. 3). Немедленная гистерэктомия выполнялась при массивном кровотечении на фоне гипотонии матки и начавшейся некупируемой коагулопатии. В одном случае имело место полное врастание и предлежание плаценты, глубоко пенетрирующее шейку матки. Показаниями к отложенной гистерэктомии стали раннее (n=2) и позднее (n=1) послеродовое, а также внутрибрюшное кровотечения (n=3). В трех случаях имело место ранение мочевого пузыря: у двух пациенток в 1-й группе, в одном – в 3-й. Обращает на себя внимание частота послеоперационных кровотечений: в 1-й группе – 1 (6,67%), во 2-й – 4 (22,2%), в 3-й – 1 (4,8%) (p=0,182). В 1-й группе у одной пациентки послеродовый период осложнился тромбозом суральной вены правой нижней конечности.
Обсуждение результатов
В настоящем исследовании первоочередной задачей, ставящейся перед авторами, являлась возможность имплементации органосохраняющего принципа родоразрешения пациенток с врастанием плаценты. Основная сложность на пути достижения данной цели – это выполнение надежного гемостаза, минимизирующего интра- и постоперационную кровопотерю, приводящие к тяжелым осложнениям. Все описанные методики способны справиться с поставленной задачей, однако наиболее эффективной с позиции снижения общего объема кровопотери является комплексный компрессионный гемостаз. Данный метод способствует минимизации анатомо-функционального ущерба за счет остановки кровоснабжения максимально близко к матке. Более низкая результативность отдельного гемостаза по руслу ВПА и ОПА объясняется большим числом анастомозов, связывающим русла этих артерий между собой, а также с бассейнами магистральных сосудов – аорты, яичниковой артерии, внутренней грудной артерии и нижней брыжеечной артерии.
Анатомо-топографические особенности кровоснабжения матки позволяют выделить три хирургические области, где возможна безопасная и эффективная временная остановка кровоснабжения: шеечно-перешеечную область, в проекции наиболее частого разделения маточных артерий на восходящую и нисходящую ветви, а также участок, в котором происходит коммуникация маточной и яичниковой артерии с двух сторон. Еще Abd Rabbo в 1994 году [7] описал метод ступенчатой деваскуляризации матки при массивном маточном кровотечении в послеродовом периоде, который начинался с односторонней перевязки маточной артерии, затем проводилась двухсторонняя перевязка, при неэффективности последних выполнялось лигирование артерий нижнего маточного сегмента; крайним шагом – прошивание яичниковых артерий.
Научная обоснованность сочетанной остановки кровоснабжения по сосудам матки отводит нас к фундаментальным работам 2013 года J.M. Palacios-Jaraquemada, где он показал различие кровоснабжения секторов S1 (тело матки) и S2 (шейка матки и верхняя порция влагалища). Сектор S1 питают маточные артерии, конечные ветви яичниковых артерий и коллатерали верхней пузырной артерии, а S2 обеспечивается руслами a. pudenda interna и анастомозами, отходящими от внутренней подвздошной артерии, маточной и нижнепузырной артерии [8]. Накопленный хирургический опыт показал, что истончение миометрия наблюдается не только в свойственном нижнем сегменте и рубцовой зоне, но и в более высокой части тела матки, что затрудняет полноценный сосудистый гемостаз после резекции стенки матки. В связи с этим целесообразно применять внутриматочную баллонную компрессию для сдавливания терминальных артерий. По данным С.В. Баринова и Я.Г. Жуковского, это позволяет игнорировать в определенной степени наличие функционирующих коммуникантов [9].
Применение утеротонической терапии в такой ситуации является малоэффективным способом его остановки.
Неонатальный показатель продолжительности пребывания новорожденного в реанимационном отделении во всех трех группах имеет высокую корреляционную зависимость с гестационным сроком родов, а также с весом ребенка (коэффициент корреляции 0,71). Из чего можно сделать закономерный вывод, что применяемое пособие никак не влияет на здоровье детей, однако их функциональная незрелость служит важным подспорьем к раннему родоразрешению, рекомендуемому при врастании плаценты. Тем не менее, данная тема остается дискуссионной, так как нет доказательной базы, позволяющей четко оценивать риски и выбирать оптимальный срок в каждом конкретном случае для оперативного родоразрешения.
Анализ осложнений, в первую очередь кровотечений, возникших как во время операции, так и в послеродовом периоде, приведших к выполнению гистерэктомии, косвенно может свидетельствовать о надежности выполнения методики того или иного метода хирургического гемостаза. Наименее эффективным показал себя метод временной окклюзии ОПА (22,2% кровотечений), что можно объяснить реваскуляризацией тем же минутным объемом крови матки после снятия зажимов. При выполнении комплексного компрессионного гемостаза происходит также восполнение сосудистого микроциркуляторного русла матки, однако профилактирующие свойства внутриматочного баллона, по-видимому, снижают риск возникновения данного осложнения. Другим осложнением являлось повреждение мочевого пузыря в трех случаях, однако достаточно трудно ассоциировать это с тем или иным применяемым методом хирургического гемостаза, так как отсепаровка мочевого пузыря от стенки матки имела место во всех операциях и технически не различалась.
Антропометрические различия в группах при сравнимом индексе массы тела, а также гестационный срок родоразрешения не могли послужить серьезными конфаундерами в «справедливой» интерпретации полученных данных.
Заключение
Результаты данного исследования доказали применимость всех трех методов гемостаза при выполнении органосохраняющего оперативного родоразрешения у пациенток с врастанием плаценты, однако наиболее эффективным способом снижения кровопотери является комплексный компрессионный гемостаз. Полученные данные подтвердили фундаментальные работы, описывающие активно функционирующие анастомотические сети в бассейне конечных ветвей маточных и яичниковых артерий, а также многочисленные коммуниканты в перешеечно-влагалищной области. Несомненно, данная проблема требует дальнейшего изучения особенностей кровоснабжения матки при врастании плаценты, поиска наиболее эффективных методов и уровней выполнения гемостаза, выработки оптимальной тактики ведения и сроков родоразрешения у пациенток с патологической инвазией плаценты.