Comparative effectiveness of the dome-shaped pessary versus cerclage using the Lubimova technique in the prevention of preterm birth in high-risk women
Objective: To compare the effectiveness of a dome-shaped pessary and cerclage using the Lubimova technique in combination with progesterone in high-risk women to prevent preterm birth.Artymuk N.V., Barinov S.V., Novikova O.N., Beglov D.E.
Materials and methods: This retrospective case-control study included 200 women. Group I (n=100) consisted of women with isthmic cervical insufficiency (ICI) who underwent a dome-shaped obstetric pessary placement; Group II (n=100) included women with ICI who underwent cerclage. The primary outcome was preterm birth (PB) before 37, 34 and 28-weeks’ gestation. Secondary outcomes were anthropometric parameters of the newborn (weight, chest, and abdominal circumference), Apgar score, the proportion of low-birth-weight babies and the proportion requiring transfer to the second stage of nursing, as well as the incidence of hypoxic brain damage in newborns.
Results: The proportion of pregnancies that ended in PB did not differ statistically significantly between the groups and was 43 (43.0%) and 41 (41.0%) in Groups I and II, respectively, p=0.375. No differences were found in PB rates in the study groups up to 28, 34, and 37 weeks of gestation. Group I neonates did not differ statistically significantly from Group II neonates in basic anthropometric indices (body weight, head and chest circumferences), Apgar score, need for respiratory support, and frequency of CNS affection. However, the rate of intraventricular hemorrhage in Group I neonates was twice lower [7 (7.0%) vs. 15 (15.0%)], p=0.071, and transfer to the second stage of nursing was statistically significantly lower [46 (46.0%) vs. 60 (60.0%)], p=0.048.
Conclusion: The use of a dome-shaped pessary and cerclage using the Lubimova technique in combination with progesterone in high-risk patients resulted in that almost half of them carried their pregnancies to full term. The pessary has certain advantages for newborns in terms of a lower incidence of intraventricular hemorrhage and transfer to the second stage of nursing.
Keywords
Isthmic cervical insufficiency (ICI) is a known risk factor for preterm birth (PB), causing about 15% of miscarriages between 16-28 weeks. Asymptomatic onset leads to late diagnosis and untimely treatment. Diagnostic difficulties are associated with the absence of pathognomonic symptoms of ICI before pregnancy [1, 2]. Currently, three strategies are commonly recommended for the treatment of ICI in the clinic, including cervical pessary, cervical cerclage, and progesterone. [3]. There is no doubt that early detection of ICI reduces the risk of PB and increases the likelihood of term birth [4]. However, there is little evidence as to which of these interventions is the preferred treatment [5].
For example, there has been a comparison of birth outcomes with cervical cerclage and the combined use of cerclage and obstetric pessary. The authors did not show differences in both total PB and individual PB categories at less than 28 weeks, 32 weeks, and 37 weeks gestation. However, combined treatment with the cerclage and pessary was associated with a shorter stay in the NICU and a trend toward higher birth weight [6].
The effectiveness of the obstetric pessary in preventing spontaneous PB in women with cervical shortening in the second trimester of pregnancy and singleton pregnancies remains questionable. A 2017 meta-analysis of 1,420 births showed that in singleton pregnancies, a pessary used in patients with a short cervix (≤25 mm) at 20–24+6 weeks gestation did not reduce the rate of spontaneous PB or improve the perinatal outcome; at the same time, it was associated with a high risk of vaginal discharge [7]. D. Herkiloglu et al. (2021), also reported the lack of pessary effect in cases where, in addition to cervical shortening, there was cervical funneling and the need for tocolysis [8]. V. Seravalli et al. (2021) also point out a decrease in the effectiveness of the obstetric pessary in patients with threatened PB, compared to asymptomatic patients [9].
The efficacy of the obstetric pessary in preventing spontaneous PB in twin pregnancy was evaluated in a study by T.K. Lau and R. Conturso (2016). The authors investigated the incidence of spontaneous PB before 34 weeks of gestation, perinatal mortality, and the combination of adverse perinatal outcomes (intraventricular hemorrhage, respiratory distress syndrome, retinopathy of prematurity, necrotizing enterocolitis) and the need for newborn therapy (ventilation, phototherapy, blood transfusion, etc.). The authors did not observe significant differences in the rate of spontaneous deliveries up to 34 weeks of gestation, as well as in other parameters [10]. Similar results were obtained in the studies by J.E. Normal et al. (2021) [11, 12], F. Monari et al. (2021) [13].
A. Zimerman et al. (2018) reported a reduction in PB rate before 28 weeks in a group of women with ICI and twin pregnancies treated with a combination of obstetric pessary and micronized progesterone [14].
In addition, a comparative study of the use of an obstetric pessary and a pessary combined with vaginal progesterone was conducted in patients at risk and women diagnosed with cervical shortening in the second trimester of pregnancy by ultrasound examination. The authors reported no differences in PB rates at 28, 32, 34, and 37 weeks of gestation between the pessary group and the combined pessary and progesterone group. Patients who also received vaginal progesterone had a shorter period of intensive therapy [15].
R.A. Rahman et al (2021) reported a positive effect of the obstetric pessary on the prevention of spontaneous PB in women with a history of spontaneous PB [2]. Besides, the authors noted that in most cases (75.3%) the use of an obstetric pessary had a significantly greater than expected treatment effect, the patients reported a positive experience and motivation to continue treatment under the supervision of experienced physicians [16].
In the works of S.V. Barinov et al. showed that the use of an obstetric pessary in combination with progesterone reduces infectious complications and the bleeding rate during pregnancy, compared to cervical cerclage in combination with progesterone [17]. The authors showed a superiority of cervical cerclage in patients with a poor obstetric and gynecological history, a cervical length of less than 15 mm and large uterine myomas [18].
N. Mouzakiti et al. (2021) reported that the use of obstetric pessary and cerclage had similar effectiveness in terms of PB prevention and was more effective in earlier diagnosed ICI, namely before the onset of cervical funneling. At the same time, pessaries have been observed to have a markedly lower rate of neonatal hospitalization and a shorter duration of their treatment compared to the group that received cervical cerclage [19]. The contradictory data obtained by different authors may be partly related to the use of different pessaries and cerclage techniques.
The present study aimed to compare the effectiveness of a dome-shaped pessary and cerclage using the Lubimova technique in combination with progesterone in high-risk women to prevent preterm birth.
Materials and methods
This is a retrospective case-control study conducted at the Kemerovo Regional Clinical Hospital between 2014 and 2021. The study was reviewed and approved by the Research Ethics Committee of the Kemerovo State Medical University (Ref. No: 225 of November 25, 2019).
The study comprised 200 women divided into two groups. Group I (n=100) consisted of women with ICI who underwent a dome-shaped obstetric pessary placement; Group II (n=100) included women with ICI who underwent cerclage. Follow-up continued from the diagnosis of ICI (18-21 weeks) until delivery.
The sample size was determined using a formula for calculation when comparing two unpaired groups; namely, we assumed to compare the PB rate of women with a short cervix at 18–21 weeks of gestation with the PB rate of women with normal cervical length at the second screening study. According to statistical data, the incidence of PB in Kemerovo region is 6.8% [20]. To obtain the results of qualitative comparison with a significance level of 0.05, the sample size of the study group should be 84 women:
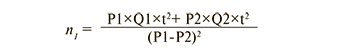
where
References
- Жабченко И.А., Занько С.Н. Истмико-цервикальная недостаточность: классификация, этиопатогенез, диагностика, методы профилактики и коррекции. Охрана материнства и детства. 2020; 1: 64-77. [Zhabchenko I.A., Zanko S.N. Isthmic-Cervical Insufficiency: Classification, Etiopathogenesis, Diagnostocs, Prevention and Correction Methods. Maternal and Child Health. 2020; (1): 64-77. (in Russian)].
- Rahman R.A., Atan I.K., Ali A., Kalok A.M., Ismail N.A.M., Mahdy Z.A. et al. Use of the Arabin pessary in women at high risk for preterm birth: long-term experience at a single tertiary center in Malaysia. BMC Pregnancy Childbirth. 2021; 21(1): 368. https://dx.doi.org/10.1186/s12884-021-03838-x.
- Boelig R.C., Berghella V. Current options for mechanical prevention of preterm birth. Semin. Perinatol. 2017; 41(8): 452-460. https://dx.doi.org/10.1053/j.semperi.2017.08.003.
- Борщева А.А., Перцева Г.М., Алексеева Н.А. Истмико-цервикальная недостаточность в структуре причин невынашивания беременности. Медицинский вестник Юга России. 2020; 11(1): 34-40.https://dx.doi.org/10.21886/2219-8075-2020-11-1-34-40. [Borscheva A.A., Pertseva G.M., Alekseeva N.A. Isthmic-cervical insufficiency in the structureof the causes of miscarriage. Medical Herald of the South of Russia. 2020; 11(1): 34-40. (in Russian)]. https://dx.doi.org/10.21886/2219-8075-2020-11-1-34-40.
- Баринов С.В., Артымук Н.В., Новикова О.Н., Шамина И.В., Тирская Ю.И., Белинина А.А., Лазарева О.В., Кадцына Т.В., Фрикель Е.А., Атаманенко О.Ю., Островская О.В., Степанов С.С., Беглов Д.Е. Опыт ведения беременных группы высокого риска по преждевременым родам с применением акушерского куполообразного пессария и серкляжа. Акушерство и гинекология. 2019; 1: 140-8. https://dx.doi.org/10.18565/aig.2019.1.140-148. [Barinov S.V., Artymuk N.V., Novikova O.N., Shamina I.V., Tirskaya Yu.I., Belinina A.A., Lazareva O.V., Kadtsyna T.V., Frikel E.A., Atamanenko O.Yu., Ostrovskaya O.V., Stepanov S.S., Beglov D.E. Experience in managing pregnant women at high risk for preterm birth, by using a dome-shaped obstetric pessary and cerclage. Obstetrics and Gynecology. 2019; 1: 140-8. (in Russian)].https://dx.doi.org/10.18565/aig.2019.1.140-148.
- Wolnicki B.G.,von Wedel F., Mouzakiti N., Naimi A.A., Herzeg A., Bahlmann F. et al. Combined treatment of McDonald cerclage and Arabin-pessary: a chance in the prevention of spontaneous preterm birth? J. Matern. Fetal Neonatal Med. 2020; 33(19): 3249-57. https://dx.doi.org/10.1080/14767058.2019.1570123.
- Saccone G., Ciardulli A., Xodo S., Dugoff L., Ludmir J., Pagani G. et al. Cervical pessary for preventing preterm birth in singleton pregnancies with short cervical length: a systematic review and meta-analysis. J. Ultrasound Med. 2017; 36(8): 1535-43. https://dx.doi.org/10.7863/ultra.16.08054.
- Herkiloglu D., Ayvacı H., Pekin O., Tarhan N., Karateke A., Sahin S. Pessary use in patients diagnosed with short cervix and cervical insufficiency. J. Matern. Fetal. Neonatal. Med. 2022; 35(10): 1834-40. https://dx.doi.org/10.1080/14767058.2021.1875209.
- Seravalli V., Campana D., Strambi N., Vialetto D., Di Tommaso M. Effectiveness of cervical pessary in women with arrested preterm labor compared to those with asymptomatic cervical shortening. J. Matern. Fetal. Neonatal. Med. 2022; 35(25): 8141-6. https://dx.doi.org/10.1080/14767058.2021.1962844.
- Lau T.K., Conturso R. Cervical pessary placement for prevention of preterm birth in unselected twin pregnancies: a randomized controlled trial. Am. J. Obstet. Gynecol. 2016; 214(1): 3.e1-9. https://dx.doi.org/10.1016/j.ajog.2015.08.051.
- Norman J.E., Norrie J., MacLennan G., Cooper D., Whyte S., Chowdhry S. et al. The Arabin pessary to prevent preterm birth in women with a twin pregnancy and a short cervix: the STOPPIT 2 RCT. Health Technol. Assess. 2021 Jul; 25(44): 1-66. https://dx.doi.org/10.3310/hta25440.
- Norman J.E., Norrie J., MacLennan G., Cooper D., Whyte S., Chowdhry S. et al. Evaluation of the Arabin cervical pessary for prevention of preterm birth in women with a twin pregnancy and short cervix (STOPPIT-2): An open-label randomised trial and updated meta-analysis. PLoS Med. 2021; 18(3): e1003506. https://dx.doi.org/10.1371/journal.pmed.1003506.
- Monari F., Salerno C., Torcetta F., Po' G., Facchinetti F. Intrapartum stillbirth for sepsis complicating Arabin cervical pessary placement in a twin pregnancy. Minerva Obstet. Gynecol. 2021; 73(3): 384-7. https://dx.doi.org/10.23736/S2724-606X.20.04721-8.
- Zimerman A., Maymon R., Viner Y., Glick N., Herman A., Neeman O. Prevention of preterm birth in twins with short mid-trimester cervical length less than 25 mm – combined treatment with Arabin,s cerclage pessary and intravaginal micronized progesterone compared with conservative treatment. Harefuah. 2018; 157(5): 301-4.
- Stricker N., Timmesfeld N., Kyvernitakis I., Goerges J., Arabin B. Vaginal progesterone combined with cervical pessary: A chance for pregnancies at risk for preterm birth? Am. J. Obstet. Gynecol. 2016;214(6): 739.e1-739.e10.https://dx.doi.org/10.1016/j.ajog.2015.12.007.
- Seravalli V., Strambi N., D’Arienzo A., Magni F., Bernardi L., Morucchio A.et al. Patient's experience with the Arabin cervical pessary during pregnancy: A questionnaire survey. PLoS One. 2022; 17(1): e0261830.https://dx.doi.org/10.1371/journal.pone.0261830.
- Barinov S.V., Shamina I.V., Lazareva O.V., Tirskaya Y.I., Ralko V.V., Shkabarnya L.L. et al. Comparative assessment of Arabin pessary, cervical cerclage and medical management for preterm birth prevention in high-risk pregnancies. J. Matern. Fetal. Neonatal. Med. 2017; 30(15): 1841-6.https://dx.doi.org/10.1080/14767058.2016.1228054.
- Barinov S.V., Artymuk N.V., Di Renzo G.C. Analysis of risk factors and predictors of pregnancy loss and strategies for the management of cervical insufficiency in pregnant women at a high risk of preterm birth. J. Matern. Fetal. Neonatal. Med. 2021; 34(13): 2071-9. https://dx.doi.org/10.1080/14767058.2019.1656195.
- Mouzakiti N., Sierra F., Herzeg A., Naimi A.A. The impact of a short cervix and funneling on the outcome in singleton pregnancies treated with an Arabin-pessary or a McDonald cerclage. J. Matern. Fetal. Neonatal. Med. 2021; 34(15): 2491-7. https://dx.doi.org/10.1080/14767058.2019.1668923.
- Чернецова А.С. Профилактика преждевременных родов. В кн.: XXXII Международный конгресс с курсом эндоскопии «Новые технологии в диагностике и лечении гинекологических заболеваний». Москва, 4-7 июня 2019: 85-6. [Chernetsova A.S. Prevention of preterm labor. In: XXXII International Congress with Endoscopy Course “New Technologies for Diagnosis and Treatment of Gynecologic Diseases”. Moscow, June 4-7, 2019: 85-6 (in Russian)].
- Наркевич А.Н., Виноградов К.А. Методы определения минимально необходимого объема выборки в медицинских исследованиях. Социальные аспекты здоровья населения [сетевое издание]. 2019; 65(6): 6-10. https://dx.doi.org/10.21045/2071-5021-2019-65-6-10. [Narkevich A.N.,Vinogradov K.A. Methods for determining the minimum required sample size in medical research. Social’nye aspekty zdorov’a naselenia/Social aspects of population health [serial online] 2019; 65(6): 6-10. (in Russian)].https://dx.doi.org/10.21045/2071-5021-2019-65-6-10.
- Министерство здравоохранения Российской Федерации. Клинические рекомендации (протокол лечения) «Истмико-цервикальная недостаточность». М.; 2018. 42c. [Ministry of Health of the Russian Federation. Clinical guidelines (treatment protocol) "Istmico-Cervical Insufficiency". М.; 2018. 42p. (in Russian)].
- Мамедалиева Н.М., Ким В.Д., Мустафазаде А.Т., Жунусова Д.Е., Абилханова Г.М., Б.Ж., Отешова Ф.М.Н., Сабденова С.С., Ахмадулина С.Л. Истмико-цервикальная недостаточность: современные аспекты диагностики и тактики ведения (обзор литературы). Вестник Казахского национального медицинского университета. 2018; 2: 10-3. [Mamedaliyeva N.M., Kim V.D., Mustafadze A.T., Zhunusova D.E., Abilhanova G.M., Oteshova B.Zh. et al. Cervical Insufficiency: Modern aspects of diagnostics and tactics of management. Bulletin of the Kazakh National Medical University. 2018; 2:10-13. (in Russian)].
- Care A., Nevitt S.J., Medley N., Donegan S., Good L., Hampson L. et al. Interventions to prevent spontaneous preterm birth in women with singleton pregnancy who are at high risk: systematic review and network meta-analysis. BMJ. 2022; 376: e064547. https://dx.doi.org/10.1136/bmj-2021-064547.
- Sperling J.D., Dahlke J.D., Gonzalez J.M. Cerclage use: a review of 3 national guidelines. Obstet. Gynecol. Surv. 2017; 72(4): 235-41. https://dx.doi.org/10.1097/OGX.0000000000000422.
- Shor S., Zimerman A., Maymon R., Kovo M., Wolf M., Wiener I. et al. Combined therapy with vaginal progesterone, Arabin cervical pessary and cervical cerclage to prevent preterm delivery in high-risk women. J. Matern. Fetal Neonatal Med. 2021; 34(13): 2154-8. https://dx.doi.org/10.1080/14767058.2019.1659771.
- Melcer Y., Kovo M., Maymon R., Bar J., Wiener I., Neeman O. et al. Arabin cervical pessary with vaginal progesterone versus vaginal progesterone for preventing preterm delivery. J. Matern. Fetal Neonatal Med. 2020; 33(20): 3439-44. https://dx.doi.org/10.1080/14767058.2019.1573894.
Received 17.08.2022
Accepted 20.09.2022
About the Authors
Natalia V. Artymuk, Dr. Med. Sci., Professor, Head of the G.A. Ushakova Department of Obstetrics and Gynecology, Kemerovo State Medical University, Ministry of Healthof Russia, +7(3842)73-48-56, artymuk@gmail.com, https://orcid.org/0000-0001-7014-6492, 22a Voroshilova str., Kemerovo, 650056, Russian Federation.
Sergey V. Barinov, Dr. Med. Sci., Professor, Head of the Department of Obstetrics and Gynecology No. 1, Omsk State Medical University, Ministry of Health of Russia, +7(3913)633-80-48, barinov_omsk@mail.ru, https://orcid.org/0000-0002-1727-7554, 12 Lenina str., Omsk, 644099, Russian Federation.
Oxana N. Novikova, Dr. Med. Sci., Professor at the G.A. Ushakova Department of Obstetrics and Gynecology, Kemerovo State Medical University, Ministry of Health of Russia, +7(3842)73-48-56, oxana777_07@mail.ru, https://orcid.org/0000-0001-5570-1988, 22a Voroshilov str., Kemerovo, 650056, Russian Federation.
Dmitriy E. Beglov, Postgraduate Student at the G.A. Ushakova Department of Obstetrics and Gynecology, Kemerovo State Medical University, Ministry of Health of Russia, +7(3842)73-48-56, beglik@gmail.com, https://orcid.org/0000-0003-3871-5450, 22a Voroshilov str., Kemerovo, 650056, Russian Federation.
Corresponding author: Oxana N. Novikova, oxana777_07@mail.ru
Authors' contributions: Artymuk N.V., Barinov S.V. – conception and design of the study; Beglov D.E., Novikova O.N. – data collection and analysis; Beglov D.E. – statistical analysis; Artymuk N.V., Novikova O.N. – manuscript drafting; Barinov S.V. – manuscript editing.
Conflicts of interest: The authors have no conflicts of interest to declare.
Funding: There was no funding for this study.
Ethical Approval: The study was reviewed and approved by the Research Ethics Committee of the Kemerovo State Medical University (Ref. No: 225 of November 25, 2019).
Patient Consent for Publication: All patients provided informed consent for the publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available on request from the corresponding author after approval from the principal investigator.
For citation: Artymuk N.V., Barinov S.V., Novikova O.N., Beglov D.E.
Comparative effectiveness of the dome-shaped pessary versus cerclage using the Lubimova technique in the prevention of preterm birth in high-risk women.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2022; 12: 75-82 (in Russian)
https://dx.doi.org/10.18565/aig.2022.193