Пролапс тазовых органов (ПТО) является хроническим состоянием, при котором органы малого таза (мочевой пузырь, тело и шейка матки, влагалище и передняя стенка прямой кишки) образуют грыжевое выпячивание в просвет влагалища, выходящее на поздних стадиях за пределы половой щели [1]. Рост заболеваемости ПТО, наблюдаемый в последние годы во всем мире, по мнению большинства исследователей, приобретает масштаб скрытой и молчаливой эпидемии [2–4].
Главной причиной ПТО является несостоятельность мышц тазового дна и брюшной стенки, возникающая после родов через естественные родовые пути [5]. При влагалищных родах травма тазового дна встречается у 10–40% родильниц, причем у первородящих в 70% случаев, а при проведении акушерских родоразрешающих операций – более чем в 90%. При этом спонтанные роды через естественные родовые пути повышают риск развития ПТО в будущем более чем в три раза, а инструментальные вагинальные роды – в пять раз по сравнению с кесаревым сечением [6].
Успех лечения ПТО напрямую зависит от своевременной и правильной диагностики имеющихся нарушений. Оценку состояния осуществляют на основании комплекса клинических, уродинамических и ультразвуковых методов исследования. На первом этапе тщательно оценивают жалобы и качество жизни женщины. Пациентки, страдающие ПТО, чаще всего предъявляют жалобы на заметный анатомический дефект, приводящий к изменению положения окружающих органов, чаще мочевого пузыря и прямой кишки. Это может приводить к нарушению мочеиспускания (учащенное мочеиспускание, затрудненное мочеиспускание, непроизвольное выделение мочи) и дефекации (запоры, недержание кала и газов). Их беспокоят также ноющие боли (чувство тяжести внизу живота), ощущение инородного тела во влагалище, нарушение сексуальной функции, выделения из влагалища. Интенсивность ощущений усиливается в течение дня и во время физической активности, а в горизонтальном положении или когда пролапс вправлен постепенно уменьшается [7].
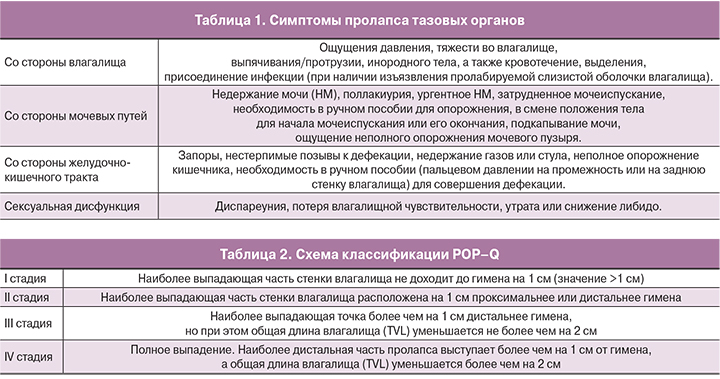
Международная урогинекологическая ассоциация (IUGA) выделяет следующие группы симптомов (табл. 1).
Для оценки качества жизни пациенток, страдающих ПТО, используются специальные вопросники, такие как PFIQ-7 (Pelvic Floor Impact Questionnaire), PFDI-20 (Pelvic Floor Distress Inventory), FSFI (Female Sexual Function Index).
Оценка гинекологического статуса включает в себя осмотр наружных половых органов, выявление максимального «выпячивания» в покое и при сильном натуживании пациентки (в положении лежа и стоя), определение степени ПТО.
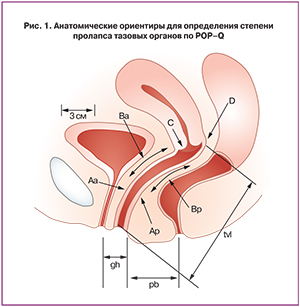 В настоящее время для классификации опущения тазовых органов применяют современную высокоинформативную шкалу POP-Q (Pelvic Organ Prolapse Quantification), предложенную Международным обществом по недержанию мочи (ICS, 1996) [8]. Анатомическую позицию шести точек (Аа, Ар, Ва, Вр, С, D) измеряют выше или проксимальнее гимена, при этом получают отрицательное значение (в сантиметрах). При расположении данных точек ниже или дистальнее гимена фиксируют положительное значение. Плоскость гимена соответствует нулю. Параметр TVL (10 см) соответствует общей длине влагалища, GH (2 см) – длине половой щели, PB (3 см) – длине сухожильного центра промежности (рис. 1).
В настоящее время для классификации опущения тазовых органов применяют современную высокоинформативную шкалу POP-Q (Pelvic Organ Prolapse Quantification), предложенную Международным обществом по недержанию мочи (ICS, 1996) [8]. Анатомическую позицию шести точек (Аа, Ар, Ва, Вр, С, D) измеряют выше или проксимальнее гимена, при этом получают отрицательное значение (в сантиметрах). При расположении данных точек ниже или дистальнее гимена фиксируют положительное значение. Плоскость гимена соответствует нулю. Параметр TVL (10 см) соответствует общей длине влагалища, GH (2 см) – длине половой щели, PB (3 см) – длине сухожильного центра промежности (рис. 1).
Стадию пролапса устанавливают по наиболее дистально расположенной части влагалищной стенки. Может быть опущение передней стенки (точка Ва), апикальной части (точка С) и задней стенки (точка Вр) (табл. 2).
Мобильность шейки мочевого пузыря оценивают с помощью Q-Tip теста, кашлевой пробы, пробы с натуживанием (проба Вальсальвы). Q-тип тест проводится с использованием стерильной ватной палочки, один конец которой способен фиксироваться в области шейки мочевого пузыря. При гипермобильности уретры разница в положении дистального конца ватной палочки в покое и при натуживании >30°. Для пробы Вальсальвы пациентке необходимо сделать глубокий вдох и потужиться, не выпуская воздух. При этом пролапс визуально станет более выраженным, а при НМ из уретры выделится моча, характер потери которой сопоставляют с силой и временем натуживания. Для кашлевой пробы пациентке надо покашлять 3–4 раза. Нужен полный вдох в промежутках между кашлевыми толчками. При положительной пробе при кашле подтекает моча, свидетельствуя о стрессовом НМ (Pves.>Pur.). Этому способствует кратковременное повышение внутрибрюшного давления во время кашля/чихания/смеха/поднятия тяжести. При наличии ПТО необходимо выполнение данных проб с репозицией пролапса с помощью пессария.
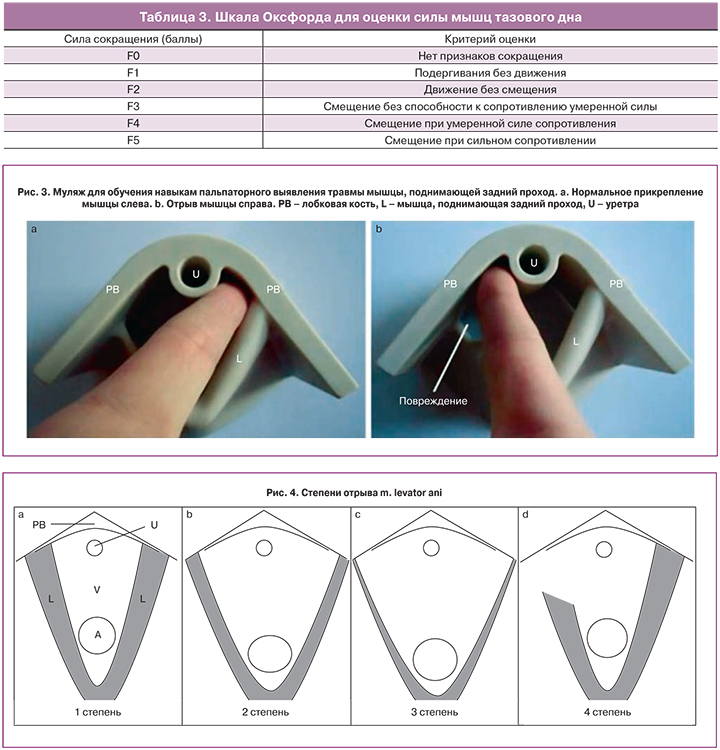
Далее определяют степень силы мышц тазового дна (МТД) по оксфордской шкале (табл. 3) [9].
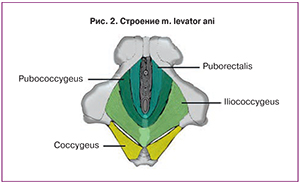 Особое значение имеет пальпация мышцы, поднимающей задний проход (m. levator ani), имеющей форму раскрытого веера. M. levator ani состоит из m. iliococcygeus, m. pubococcygeus и m. рuborectalis (последние две составляют m. pubovisceralis) (рис. 2).
Особое значение имеет пальпация мышцы, поднимающей задний проход (m. levator ani), имеющей форму раскрытого веера. M. levator ani состоит из m. iliococcygeus, m. pubococcygeus и m. рuborectalis (последние две составляют m. pubovisceralis) (рис. 2).
Щель диафрагмы таза, ограниченная ножками m. рuborectalis, представляет собой самые большие грыжевые ворота в женском организме. Расширение ее приводит к значительным нарушениям функции нескольких систем органов. Удивительно, что такая важная структура, так легко доступная для пальпации, до сих пор игнорируется врачами, занимающимися дисфункцией тазового дна [10].
Повреждение мышцы, поднимающей задний проход, означает нарушение связи между m. puborectalis и нижней ветвью лобковой кости [11]. Для выявления отрыва мышцы необходимо пальпировать щель между уретрой и m. puborectalis, куда в норме помещается один указательный палец. Его необходимо перемещать латерально по отношению к уретре, попросив пациентку сократить мышцы тазового дна. Если палец смещается вдоль нижней ветви лобковой кости на 2–3 см и при этом не пальпируются мышечные сокращения, это свидетельствует о полном отрыве мышцы [10] (рис. 3).
Повреждение m. puborectalis является наиболее распространенным следствием родов через естественные родовые пути [12, 13], оказывающее наибольшее влияние на целостность и функцию тазового дна, особенно если травма двусторонняя [14]. В некоторых случаях подобные дефекты становятся очевидными и диагностируются еще в родильном зале у женщин с крупными разрывами влагалища, но зачастую они остаются незамеченными [15, 16].
На рис. 4 представлено схематическое изображение различных степеней отрыва m. levator ani: (а) 1-я степень – в щель между уретрой и мышцей помещается один указательный палец; (b) 2-я степень – более одного пальца, с четко пальпируемой мышцей, как в покое, так и во время сокращения; (c) 3-я степень – более одного пальца, без различимой мышцы в покое или при сокращении; (d) 4-я степень – нет связи между мышцей и лобковой костью (справа). А – прямая кишка; РВ – лобковая кость; V – влагалище.
Существенную помощь в оценке состояния тазового дна оказывает ультразвуковое исследование (УЗИ). В силу неинвазивности данного метода его проведение возможно при любой степени пролапса. Значение эхографии заключается в возможности выявлении степени нарушений, что определяет дальнейшую тактику ведения пациентки. Для оценки структур тазового дна и дисфункции нижних отделов мочевого тракта используют промежностное 2D УЗИ. Снимки получают в покое, при сокращении МТД и во время пробы Вальсальвы (с натуживанием).
При стрессовом НМ важное значение имеет оценка подвижности шейки мочевого пузыря, так как гипермобильность играет ключевую роль в патофизиологии этого состояния. Положение оценивают в срединно-сагиттальной плоскости. Необходимо измерить расстояние от шейки мочевого пузыря до нижнезаднего края лона в покое и во время пробы Вальсальвы [17]. Измерения ниже лона – негативны, выше – позитивны. Далее вычисляют разницу и получают значение, равное опущению шейки мочевого пузыря. Опущение шейки мочевого пузыря более 10 мм принимают за гипермобильность [18–20].
При стрессовом НМ во время максимальной пробы Вальсальвы проксимальная уретра (она же шейка мочевого пузыря) может вращаться в задненижнем направлении. Степень вращения может быть оценена с помощью измерения позадипузырного угла между проксимальной уретрой и треугольником. Опущение шейки мочевого пузыря и вращение уретры тесно связаны со стрессовым НМ [21, 22]. Нормальными считаются значения 90–120°. При НМ угол может увеличиваться до 160–180° [23].
Наличие на снимке воронки свидетельствует об открытии проксимальной трети уретры во время кашля или пробы Вальсальвы, а иногда даже в покое. Происхождение ее связывают с низким давлением закрытия уретры [24, 25]. Воронка внутреннего отверстия уретры может наблюдаться у женщин со стрессовым НМ, но также описаны случаи и у женщин с ургентным типом НМ [26].
Таким образом, промежностное УЗИ выявляет характерные признаки для НМ: опущение шейки мочевого пузыря, увеличение позадипузырного угла >120°, воронку внутреннего отверстия уретры при пробе Вальсальвы [21].
Промежностное УЗИ может использоваться для оценки функции МТД, особенно у женщин со стрессовым НМ, как до, так и после родов [27]. Доказательством эффективного сокращения мышц является смещение органов малого таза в краниовентральном направлении в срединно-сагиттальной плоскости и смещение внутреннего отверстия мочеиспускательного канала относительно задненижнего края лона. Другим признаком мышечной активности является уменьшение расстояния между лобковым симфизом и мышцей, поднимающей задний проход в срединно-сагиттальной плоскости, то есть сокращение переднезаднего размера щели диафрагмы таза [28, 29]. Сужение щели без смещения шейки мочевого пузыря свидетельствует о том, что пациентка во время сокращения МТД одновременно сокращает мышцы передней брюшной стенки, тем самым увеличивая внутрибрюшное давление. В связи с этим пациенток необходимо обучать правильной технике сокращения МТД при помощи тренировок под контролем УЗИ [30].
Также при УЗИ определяют дефекты наружного и внутреннего сфинктеров ануса. Повреждения анального сфинктера связаны с родами, возрастом, оказанием оперативного пособия в родах, что в конечном итоге может привести к недержанию кала [31, 32]. Промежностное УЗИ является легко осуществимым и неинвазивным методом визуализации анального сфинктера [33–35]. На снимке слизистая прямой кишки визуализируется в форме «звезды», образованной складками пустого ануса, внутренний анальный сфинктер (IAS) визуализируется в виде гипоэхогенного кольца, внешний сфинктер (EAS) – в виде гиперэхогенного кольца вокруг внутреннего анального сфинктера [33].

Размеры щели диафрагмы таза могут быть определены с помощью 3D УЗИ. Для этого необходимо измерить расстояние от заднего края симфиза до m. puborectalis, поперечный размер диафрагмы таза и рассчитать площадь щели диафрагмы таза, коррелирующей со степенью тяжести пролапса.
Для диагностики подвижности тазовых органов также могут проводиться такие методы, как проктография, метод динамической магнитно-резонансной томографии и аноманометрии.
Женщинам с ПТО, сочетающимся с нарушением мочеиспускания, рекомендовано проведение урофлоуметрии с определением остаточной мочи в качестве рутинного скрининга. Урофлоуметрия – неинвазивный метод, не требующий специальной подготовки и предварительного обследования пациентки. При проведении данного метода пациентке необходимо мочиться в специальный мочеприемник. Моча через воронку поступает в урофлоуметр, который регистрирует ее объем в единицу времени. В результатах урофлоуметрии регистрируют функциональное состояние детрузора и замыкательного аппарата уретры. Урофлоуграмма оценивается по следующим показателям: общее время мочеиспускания, максимальная и средняя скорость потока мочи, суммарный объем мочеиспускания, время ожидания начала мочеиспускания, объем выделенной мочи и объем остаточной мочи [16] (рис. 5а, б).
Особого внимания заслуживает метод тренировки мышц тазового дна под контролем УЗИ, который является методом первой линии консервативного лечения недержания мочи [36, 37]. Ультразвук может быть использован в качестве инструмента для оценки физиологической и патологической подвижности мочевого пузыря, а также в качестве биологической обратной связи для лучшего понимания функционирования тазового дна во время кашля. Пациентку можно научить предварительному сжатию мышц тазового дна до кашля [38, 39]. Благодаря этому во время кашля шейка мочевого пузыря стабилизируется и не происходит подтекания мочи. Особенно важно исключить вовлечение косых мышц живота.
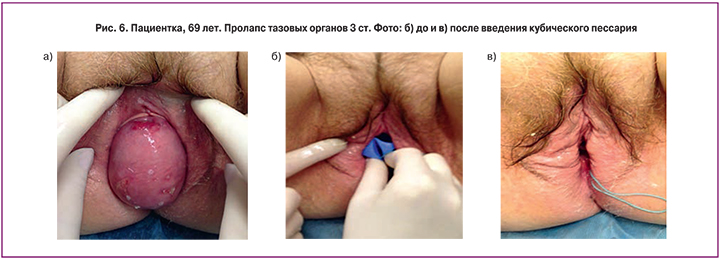
Лечение ПТО до 2-й стадии по классификации POP-Q необходимо начинать с консервативного метода лечения, одним из которых является использование пессариев, эффективность применения которых по данным 1 рандомизированного контролируемого исследования составляет 60% (1b-A), а по данным когортных исследований достигает 92% [40, 41].
Показаниями к использованию пессариев являются: пролапс гениталий любой степени с наличием или без ассоциированных симптомов, стрессовое НМ на фоне пролапса, наличие симптоматического пролапса, в случаях, когда проведение хирургического вмешательства невозможно. Абсолютных противопоказаний для применения пессариев нет. Относительные противопоказания: вагинит, декубитальные язвы, когнитивные расстройства, пролапс IV степени.
Целью применения пессариев являются [42]:
- Восстановление анатомического положения тела и шейки матки, что препятствует опущению стенок влагалища;
- Предотвращение непроизвольного мочеиспускания при напряжении, кашле, чихании и поднятии тяжестей, так как некоторые виды пессариев обеспечивают возможность фиксации уретровезикального угла в правильном анатомо-физиологическом положении;
- Предупреждение дальнейшего прогрессирования опущения тазовых органов;
- Возможность отсрочить время операции.
Главная задача врача – совместно с пациенткой правильно подобрать пессарий оптимальной формы. При незначительных или средних степенях опущения применяются кольцевые или чашечные пессарии с поддерживающим механизмом действия, при более выраженных – грибовидные и кубические – поддерживающие и заполняющие внутреннее пространство, при сопутствующем НМ выбирают урогинекологические пессарии с леватором, наличие которого оказывает запирающее действие вследствие давления на уретро-везикальный угол – уретральный и чашечно-уретральный пессарии.
Не менее важно и определение оптимального размера пессария, для чего в первую очередь применяются адаптационные кольца. Во время вагинального исследования ориентировочно определяется размер кольца для тестирования. Выбранное кольцо вводится во влагалище и пациентке предлагается встать, походить, покашлять. Через 10–15 минут определяют положение кольца и оценивают жалобы. Если не произошло смещения кольца вниз и пациентку не беспокоит дискомфорт, то выбранный размер можно считать подходящим. Для облегчения установки пессария и купирования симптомов генитоуринарного синдрома рекомендуется смазать его кремом, содержащим эстриол.
После подбора размера и формы пессария врач обучает пациентку технике самостоятельного введения и извлечения.
Необходимость регулярного наблюдения за пациентками очевидна. После установки пессария последующую консультацию необходимо назначить через 2 недели, затем через 3 месяца, далее 1 раз в 3–5 месяцев. В ходе контрольных визитов врач извлекает и обрабатывает пессарий, оценивает состояние слизистой вульвы, влагалища и шейки матки, регистрирует динамику симптомов заболевания, оценивая ощущения пациентки на фоне пессария.
Замена пессария может потребоваться при возникновении следующих симптомов: дискомфорт во влагалище, выпадение пессария, патологические выделения из половых путей, затруднение мочеиспускания или дефекации, появление симптомов НМ (при скрытом НМ).
Факторами, снижающими возможность использования пессария, являются: короткая длина влагалища (<6 4="" p="">
Редко пессарии способны вызвать серьезные осложнения (пузырно-влагалищный свищ, фекальная закупорка, гидронефроз и уросепсис), которые могут быть вызваны отсутствием контроля и наблюдения со стороны женщин или забытыми после введения пессариями.
В связи с этим, пациенткам необходимо придерживаться рекомендаций по использованию пессариев:
- Извлечение и обработка пессария производится 1 раз в 3 недели (кроме кубических и грибовидных, которые необходимо извлекать из влагалища ежедневно);
- После извлечения пессарий промывают проточной водой с мылом и кладут в контейнер или пакет;
- При уретровагинальной атрофии пессарии используются на фоне локальной терапии эстрогенами;
- Каждые 3–5 месяцев пациентка осуществляет визиты в клинику.
После длительного использования пессария в связи с улучшением состояния может потребоваться его замена на пессарий меньшего размера.
Критерии эффективности использования пессариев и вопросники:
- Отсутствие жалоб или их уменьшение на 50% (по опроснику PFDI-20).
- Отсутствие прогрессирования или уменьшение степени пролапса по классификации POP-Q.
- Правильное положение тазовых органов при установленном пессарии (объективно).
- Отсутствие эпизодов недержания мочи или кала (PFDI-7).
- Улучшение сексуальной функции (FSFI).
- Улучшение качества жизни (SF-36).
Таким образом, несмотря на высокую эффективность и безопасность хирургического лечения, пессарии продолжают занимать ведущую роль в лечении ПТО у определенной группы пациенток (отказ от оперативного вмешательства, предоперационная подготовка и послеоперационная реабилитация, профилактика прогрессирования данного заболевания и др.).
Разнообразие форм и размеров пессариев дает возможность индивидуального подбора необходимого вида для каждой пациентки. Пессарии почти не имеют противопоказаний, что позволяет их рекомендовать практически всем пациенткам с ПТО.