В настоящее время большая роль в лечении недержания мочи отводится консервативному немедикаментозному лечению: поведенческой терапии, электро- и электромагнитной стимуляции, тренировкам мышц тазового дна (МТД) в самостоятельном режиме, с использованием портативных устройств или стационарного оборудования [1]. В данной парадигме работают специалисты, занимающиеся нарушениями мочеиспускания. Это особенно актуально при выборе метода лечения недержания мочи, одного из самых частых урологических заболеваний у женщин [2]. Каждая третья женщина в мире имеет недержание мочи той или иной степени выраженности [3]. Оно чаще всего возникает вследствие коллагеновой недостаточности, травматичных или многократных родов, занятий тяжелым физическим трудом, профессиональным спортом/фитнесом с высокими физическими нагрузками [4]. Недержание мочи также возникает у женщин после хирургического и лучевого лечения онкогинекологических заболеваний [5]. Избыточный вес является фактором риска возникновения недержания мочи, распространенность которого у женщин растет пропорционально увеличению индекса массы тела [6].
Действительно, недержание мочи является междисциплинарной проблемой. Над совершенствованием известных методов и разработкой инновационных методик лечения работают урологи, гинекологи и реабилитологи во всем мире. Этим, например, обусловлено большое разнообразие оперативных техник лечения стрессового недержания мочи.
В настоящее время имеется 4 алгоритма лечения недержания мочи:
1. консервативная немедикаментозная терапия;
2. фармакологическая терапия;
3. малоинвазивные методы лечения;
4. хирургическое лечение [7].
Рассмотрим предлагаемые методики лечения в обратном порядке, начиная с самой сложной.
Хирургическое лечение
Золотым стандартом лечения недержания мочи остается слинговая уретропексия. Метод заключается в имплантации под уретру свободной синтетической петли и создании удерживающего механизма, частично замещающего сфинктерную функцию. Общая эффективность метода – более 80% [8]. «Слинговые» процедуры имеют ряд осложнений (кровотечение, перфорация мочевого пузыря, повреждение сосудистого нервного пучка в зоне обтураторного отверстия, длительный болевой синдром, нарушение опорожнения мочевого пузыря, эрозия уретры в зоне имплантации, кровотечение, нарушение функции кишечника, рецидив или появление пролапса органов таза, нарушение сексуальной функции), которые по мере совершенствования техники операции встречаются все реже [9]. К хирургической тактике обычно прибегают в случаях, когда консервативное лечение неэффективно. У женщин с пролапсом органов таза III–IV степени консервативные методы лечения применяются редко, так как малоэффективны. В таких случаях уретропексия выполняется одномоментно с хирургической коррекцией пролапса тазовых органов [10].
Малоинвазивные виды лечения
Данный вид лечения относится к 3-й линии терапии. К нему прибегают, если 1-я и 2-я линии лечения неэффективны. Современным методом малоинвазивного лечения является пара- или трансуретральное введение объемообразующих субстанций. Эффективность данного вида лечения при легких формах недержания мочи составляет около 60%. Основным неблагоприятным фактором является временный эффект, связанный с резорбцией введенного вещества. По данным различных авторов, продолжительность эффекта в среднем составляет от 12 до 24 месяцев [11, 12]. Миграция объемообразующего вещества является нежелательным явлением, которое может наблюдаться после манипуляции и в некоторых случаях требует последующего хирургического вмешательства [13]. Также имеются технические сложности при введении и выборе объема вводимого вещества, связанные с необходимостью достижения «равновесного» воздействия, то есть обеспечения удержания мочи без развития механической инфравезикальной обструкции [14].
В качестве объемообразующего вещества не рекомендовано использовать аутологичный жир или гиалуроновую кислоту из-за риска развития абсцесса или эмболии. По данным исследований, самым частым осложнением является инфекция нижних мочевых путей [15].
Фармакологическая терапия
Возможности медикаментозного лечения (2-я линия терапии) при стрессовом недержании мочи ограничены. В систематическом обзоре (Cochrane), проанализировавшем данные 17 исследований, показано, что применение местных эстрогенов у женщин постменопаузального возраста вызывает уменьшение выраженности симптомов недержания мочи в краткосрочном наблюдении [16]. В исследовании Castellani D. et al. (2015) местная терапия эстрогенами уступает тренировкам МТД по уменьшению выраженности недержания мочи [17]. Достижение клинического эффекта возможно при сочетании применения эстрогенов и электростимуляции МТД [18].
В исследованиях с открытым приемом и длительностью наблюдения 1 год и более оценивали влияние препарата «Дулоксетин» на уменьшение выраженности стрессового недержания мочи [19]. Дулоксетин является ингибитором обратного захвата нейротрансмиттеров, серотонина и норадреналина [20]. В обоих исследованиях отмечалась высокая частота прекращения приема препарата в связи с отсутствием эффективности и частыми нежелательными явлениями (тошнота и рвота – 40% и более, сухость во рту, запоры, головокружения, нарушения сна, сонливость и усталость). На территории Российской Федерации дулоксетин не разрешен для лечения стрессового недержания мочи.
Консервативное лечение
Консервативное немедикаментозное лечение относится к 1-й линии терапии. Продолжаются разработки новых высокоэффективных консервативных методов лечения, в том числе путем внесения изменений в «старые» известные технологии. Проведение консервативного немедикаментозного лечения особенно важно при недержании мочи легкой и средней степени, когда выполнение хирургического пособия преждевременно или не имеет абсолютных показаний [21].
В данном обзоре нами проведена оценка современных возможностей консервативного немедикаментозного лечения недержания мочи, в том числе методик с применением биологической обратной связи (БОС).
Поведенческая терапия
Лечение недержания мочи начинают с изменения образа жизни пациентки. Элементами поведенческой терапии являются: изменение питьевого режима, принудительный ритм мочеиспусканий, отказ от курения, отказ от употребления кофеинсодержащих напитков, диетические рекомендации, регуляция стула. Важную роль играет снижение веса. Во многих эпидемиологических исследованиях показано, что избыточный вес является фактором риска недержания мочи. Количество пациенток с ожирением, которым проводится хирургическая коррекция недержания мочи, превышает показатели в общей популяции [22]. Как правило, поведенческую терапию не проводят как самостоятельный вид лечения, ее обычно сочетают с другими методами консервативного лечения.
Тренировки мышц тазового дна
Пациентки, особенно молодого возраста, демонстрируют высокий запрос на нехирургическое лечение и высокую приверженность терапии. Женщины молодого возраста, в силу присущего им выраженного стремления улучшать показатели здоровья и качества жизни, а также по своему функциональному статусу хорошо воспринимают элементы поведенческой терапии и «тренировочные» методики, направленные на улучшение функционального состояния тазового дна.
Тренировка МТД по методу Кегеля (упражнения Кегеля), в том числе с использованием портативных устройств, приборов и влагалищных конусов, является простым способом восстановления удерживающей функции сфинктерного аппарата мочевого пузыря. Однако множество исследований, посвященных обзору данного вида лечения, констатировали, что метод в режиме монотерапии имеет низкую эффективность [23]. При выполнении упражнений Кегеля отсутствует возможность «отключения» мышц-антагонистов. Работа в самостоятельном бесконтрольном режиме не позволяет многим пациенткам выполнять упражнения в полном объеме и необходимом качестве. Тренировки МТД можно использовать для профилактики недержания мочи, в том числе во время беременности или на этапе восстановления после родов или хирургического лечения [24, 25]. В наблюдении, где сравнивали две группы женщин со стрессовым недержанием мочи (в 1-й группе женщины выполняли тренировки МТД, во 2-й группе лечение не проводилось), продемонстрировано, что у женщин, выполнявших тренировки МТД, устранение симптомов наблюдалось в 8 раз чаще [26]. Также опубликованы данные, что применение методики БОС в дополнение к тренировкам МТД увеличивает эффективность последних [27].
По данным многочисленных исследований также показано, что использование влагалищных конусов эффективнее, чем отсутствие лечения. Полученные данные не позволяют сравнивать такие тренировки со структурированными тренировками МТД [28]. В исследованиях также отмечено, что часть пациенток испытывают дискомфорт и проблемы с мотивацией, поэтому их приверженность «тренировочным» методам лечения остается низкой [29].
Электро- и электромагнитная стимуляция
Электростимуляция, в том числе интравагинальная, в лечении стрессового недержания мочи используется долгие годы [30]. В обзоре (Cochrane) 2017 г. показано, что по субъективным оценкам пациенток электростимуляция тазового дна эффективнее, чем отсутствие лечения [31].
Современным методом электромагнитной терапии является экстракорпоральная электромагнитная стимуляция (ЭЭМС) с использованием так называемого «электромагнитного кресла». Метод привлекает интерес специалистов не только благодаря широким возможностям применения и большому спектру воздействия, но и его удобству. Первое многоцентровое клиническое исследование было проведено в 1999 г. коллективом ученых из США. В исследование вошли 83 женщины с установленным диагнозом стрессового недержания мочи. В результате лечения были получены результаты, доказывающие эффективность ЭЭМС: 34% пациенток отказались от использования прокладок, а 32% пациенткам требовалось не более 1 прокладки в день [32, 33]. В 2013 г. Tsia-Shu Lo et al. также оценили эффективность ЭЭМС у женщин со стрессовым и ургентным недержанием мочи. 86,8% пациенток со стрессовым недержанием мочи отметили снижение симптомов недержания [33, 34].
Тренировки мышц тазового дна методом биологической обратной связи
Тренировка мышц тазового дна по методу БОС является эффективным способом консервативного лечения пациенток со стрессовым недержанием мочи. Метод заключается в аппаратном контроле сокращений изолированных групп мышц при тренировке, что позволяет более корректно выполнять упражнения, направленные на восстановление удерживающей функции сфинктерного аппарата мочевого пузыря [35].
Предложенная в 2018 г. в НИИ урологии методика предварительного «пассивного» вовлечения в работу необходимой группы мышц путем проведения ЭЭМС на отдельном аппарате (физиотерапевтический аппарат для проведения экстракорпоральной магнитной стимуляции мышц тазового дна «Авантрон») перед БОС-тренировкой позволяет быстрее включить мышцы в работу и повысить эффективность БОС-терапии. Такое сочетание технологий консервативного лечения применяется как при дисфункциональном мочеиспускании, так и у пациенток с недержанием мочи, что в последнее время становится актуальным [36]. Методика требует обязательного наличия в клинике/отделении двух приборов. Тем не менее для специализированных центров использование технически сложных, но повышающих эффективность методов вполне оправдано.
Имеющиеся методы электромагнитного воздействия или терапия по методу БОС остаются актуальными, но требуют длительного использования с необходимостью сохранения пациентками приверженности лечению [37, 38].
Актуальной задачей для специалистов является разработка консервативного немедикаментозного метода лечения с высоким уровнем эффективности, безопасности и воспроизводимости, что позволит проводить тренировки на качественно новом уровне, сократить время лечения, снизить медико-экономические затраты, получить более благоприятный и длительный функциональный результат.
В настоящее время перспективным направлением является разработка сочетанных методик консервативного немедикаментозного лечения. Большой потенциал для развития этого направления существует в использовании биоуправления, в том числе опорной реакции. БОС применяется не только в чисто урологических методиках. В настоящее время доступны технические решения для проведения эффективных тренировок опорной реакции (опороустойчивости) с БОС [39].
Неврологи и ортопеды также широко применяют устройства, в которых используются элементы БОС. Одним из самых распространенных методов с применением БОС является тренировка на стабилоплатформе [40].
Стабилоплатформа (стабилометрическое устройство, стабилометрическая платформа, стабилограф) – устройство для оценки стабильности позы человека по опорной реакции на специальной платформе [41]. Изначально устройства такого типа были разработаны для того, чтобы с максимально возможной точностью регистрировать и анализировать колебания тела вертикально стоящего человека. Принцип действия приборов похож на принцип действия электронных весов. Но, в отличие от весов, силовые платформы измеряют не только силу, с которой человек воздействует на опору. Также учитываются характеристики того, как эта сила распределяется в плоскости опоры, то есть, как человек взаимодействует с гравитационным полем Земли [42] (рисунок).
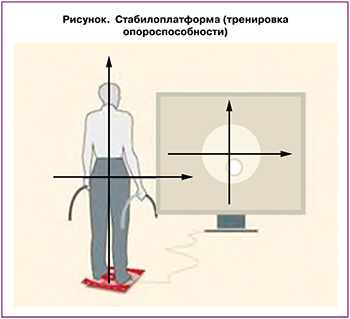
При стабилометрии (биоуправление по опорной реакции) используют возможности визуализации (зрительный анализатор). В целом стабилоплатформа используется для диагностики состояния функций вестибулярного аппарата, заболеваний опорно-двигательного аппарата, а также для нейромышечной реабилитации, для восстановления утраченных двигательных навыков при заболеваниях центральной и периферической нервных систем, в том числе в комплексной терапии постинсультных состояний, для восстановления нарушенного равновесия и чувства координации [43]. В случаях, когда стабилоплатформа используется для тренировки опороустойчивости, в работу вовлекаются мышцы нижних конечностей и таза, в том числе те, которые необходимы для тренировок «на удержание мочи». Тренировка опороустойчивости на стабилоплатформе реализуется в приборах, где для БОС также используется зрительный анализатор, как это происходит при тренировке МТД методом БОС при лечении недержания мочи.
При стандартной БОС-терапии без предварительного физического и интеллектуального вовлечения пациенткам требуется более длительное время на физическое вступление в работу необходимых мышц. Достижение интеллектуальной и психоэмоциональной концентрации при стандартной БОС-тренировке также требует временных затрат, что снижает полноценность и эффективность занятия.
Усовершенствование метода БОС подразумевает не только физическое вовлечение мышц в работу, как этот предложено в методике «ЭЭМС+БОС», но и интеллектуальное, в том числе с использованием зрительного анализатора, что необходимо для последующей БОС-тренировки с визуальным контролем. Для решения этой задачи перспективным направлением является возможность использования предварительной тренировки опороустойчивости на стабилоплатформе с вовлечением МТД и задействованием зрительного анализатора.
Применение сочетания БОС-терапии и короткой стабилотренировки, которые являются интеллектуально и физически затратными и требуют большой концентрации, может позволить быстрее вовлекать пациентку в активную работу, при этом не вызывая утомления. Положительным моментом является прецизионность стабилотренировки в отношении необходимой в последующей работе группы мышц. Повышение эффективности каждого сеанса за счет комбинации стабилоплатформы и БОС также может позволить сократить количество тренировок, необходимых для достижения эффекта.
Заключение
При проведении консервативного лечения, требующего активного участия пациентки, важными факторами являются не только конечная эффективность, но и время возникновения положительной динамики. Раннее снижение выраженности симптомов служит дополнительным стимулирующим фактором и может мотивировать пациентку к продолжению лечения.
Использование сочетанных тренировочных методик и возможность более раннего наступления положительной динамики также может повышать конечный функциональный результат. Методика является несложной в выполнении в техническом плане и может быть доступной на различных уровнях оказания медицинской помощи.