The risk of pelvic organ prolapse in women after obstetric traumas
Aim. Assessment of the risk of pelvic organ prolapse in women after obstetrical traumas.Askerova M.Sh.
Materials and methods. This was a prospective observational study. It included the women aged 45–74 years. The study was conducted in the Antenatal Clinic of Maternity hospital No. 7 in Baku. Initially, a list of all female patients (17,814) aged 45–75 years, who were assigned to the Antenatal Clinics was prepared. The research sample included consistently every 25th woman from this list. The sample size (710 women) was determined taking into account the probable prevalence of pelvic organ prolapse in women and maximum permissible sampling error (3%). The sample population was divided into groups according to the degree of prolapse, the age, number of pregnancies and childbirths in medical history, body weight and body mass index, the employment, educational level and severity of comorbidity. The differences between the groups were assessed using χ2 test. Statistical data processing was carried out using qualitative data analysis method.
Results. The prevalence of pelvic organ prolapse was 59.9% among all assessed women, and it was low in the group of women without obstetric traumas in history (26.5%), and in women with obstetric traumas of different degrees it was 67.2–100%. Assessment of risk factors in women showed that only a small proportion of them did not have risk factors for pelvic organ prolapse (50/710; 7%). Most of women had 2 and 3 risk factors in history (32.5 and 27.0%, respectively).
Conclusion. The prevalence of pelvic organ prolapse was 59.9% and varied ranging from 26.5% (in the absence of obstetric traumas) to 100% (with third- and fourth-degree perineal tears in medical history). Among the risk factors for genital prolapse (age, dysplasia of connective tissue, burdened family history and others), obstetric traumas prevail. A combination of risk factors and obstetric traumas increase the risk of pelvic organ prolapse.
Keywords
Pelvic organ prolapse (POP) is widespread among older women worldwide [1–3]. According to Barber M.D., Maher C. [1] the peak of detection of this condition reaches 50% at the age of 60–69 years. In Pakistan, 10.3% of rural women had severe forms of pelvic organ prolapse [2]. Women with four or more children had the highest percentage of pelvic organ prolapse (75%). According to Korean researchers, the incidence of POP was 71±1 per 100,000 population in all age groups and 180±4 per 100,000 women over 50 years old [3]. The pronounced differences in the incidence of POP among populations are primarily due to the methodology used for detection of this condition. The diagnosis of POP was established in 59.9% of cases during comprehensive examination of women aged 45–74 years in Baku [4]. Prolapse of the uterus and vagina was most commonly detected (41.3%); cystocele, enterocele, rectocele and other types of prolapse were less often found. Young women (aged 15 years and over) were examined in Pakistan. POP detection rate depended on age and varied in the range of 1.3–18.0% [1]. The percentage of severity of POP varied in some studies [1, 4]: pelvic organ prolapse stage IV was in 20.7% and 0.7% of women, stage III was in 17.1% and 8.5%. Currently, there are many publications on the development of new methods of treatment of POP, and the methods of surgical treatment are constantly being improved [5, 6]. Some studies reported risk factors for POP [7–10]. It is believed, that risk of POP development is increases multiple folds in multiparous women on the background of connective tissue dysplasia [11]. The role of obstetric traumas in medical history of women in formation of the risk factors of POP both depends on the type and severity of traumas, and this issue requires in-depth study.
Aim of the study: assessment of the incidence of POP in women after obstetrical traumas of various severity associated with other risk factors for pelvic organ prolapse.
Materials and methods
This report is a continuation of our previously published research [4]. Comprehensive gynecological examination covered 710 women. The sampling was based on selection of every 25th woman assigned to the Antenatal Clinic of Maternity Hospital No.6 at the place of residence in Baku. To assess the presence of POP, questionnaires for women with pelvic floor disorders (PFDI-20 and PFIQ-7) were used [11]. Information about obstetric traumas was obtained by studying the primary records in the hospital obstetric settings. The criteria of POP–Q system were used to detect the stage of POP [9]: Aa and Ba – the distal and proximal parts of the anterior vaginal wall; Ap and Bp – the distal and proximal parts of the posterior vaginal wall; С – the lowest edge of the cervix; D – topmost point of the posterior vaginal wall; GH – genital hiatus; PB – the perineal body; TVL – the total vaginal length.
- Stage 0: no prolapse. Points Аа, Ар, Ва, Вр area ll 3 cm. Points С and D range from TVL to TVL-2 cm (negative number of TVL).
- Stage I: the most distal portion of the prolapse is more than 1 cm above the level of the hymen (> -1 см).
- Stage II: the most distal portion of the prolapse is 1 cm or less proximal or distal to the hymenal plane (≤ -1 cm, but not ≤ +1 cm).
- Stage III: the most distal portion of the prolapse protrudes more than 1 cm below the hymen but protrudes no farther than 2 cm less than the total vaginal length (TVL-2 cm), (≥ -1 cm, but ≤ +1cm).
- Stage IV: complete genital prolapse. The most distal portion of the prolapse protrudes more than TVL-2 cm.
Information about chronic diseases for the last 3 years, the course and outcomes of childbirth, as well as delivery methods and surgery for pelvic organs was taken from the medical records and birth histories.
Statistical analysis
The purpose of the analysis was to assess the statistical significance of the prevalence of POP among the women with obstetric traumas of various severity on the background of other risk factors for prolapse.
Total sample number of women was divided into groups depending on the presence of prolapse (285 women had no prolapse, and 425 women had prolapse of various stages), the age (45–49 years; 50–54 years; 55–59 years; 60–64 years; 65–69 years; 70–74 years), the number of pregnancies and births in history, body weight and body mass index, employment status, educational level and comorbidity. Each group was divided into 6 subgroups depending on the type of childbirth and the type of obstetric trauma. The first subgroup included nulliparous women and parous women without obstetric traumas (n=230). The second subgroup included women who had forceps delivery or vacuum extractor delivery (n=81). The subgroups 3–6 included the women who had first-degree, second-degree and third- or fourth degree perineal tear, as well as underwent perineotomy or episiotomy (n=123, n=98, n=53 and n=125, respectively). In these subgroups, the percentage of women with POP was calculated per 100 patients.
Confidence interval was computed according to Wilson's formula [12] using a free online calculator.
Statistical significance of intergroup differences in the number of women with POP was assessed using χ2 test. The significance level of p=0.05 was considered critical in interpretation of the statistical analysis results. Statistical analysis of the qualitative characteristics was performed using Excel 2010 for Data Analysis.
Results
Distribution of women with different medical and demographic characteristics according to the types of obstetric traumas in medical history is shown in Table 1. A significant proportion of women (32.4%) had no obstetric traumas in history. Depending on the medical and demographic characteristics, the proportion ranged from 14.3% (the group of women with POP) to 59.3% (the group of women without POP). Severe obstetric traumas of the third- or fourth-degree were in 7.5% of women, and this rate ranged between 5.8% and 12.5% depending on the medical and demographic characteristics of women.
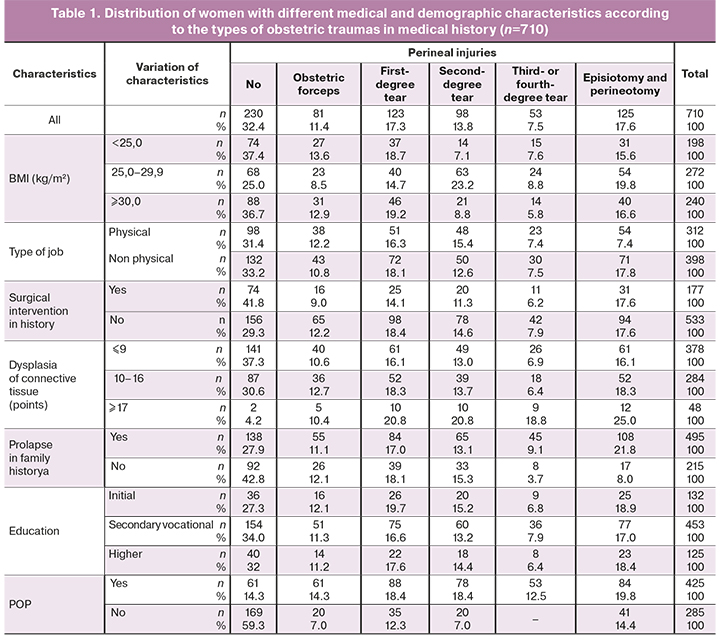
The prevalence of POP was 59.9% among all examined women: the lowest rate was in group without obstetric traumas in history (26.5%), with obstetric traumas it ranged from 67.2% to 100%.
Table 2 shows the prevalence of POP associated with various obstetric traumas among women with different medical and demographic characteristics.
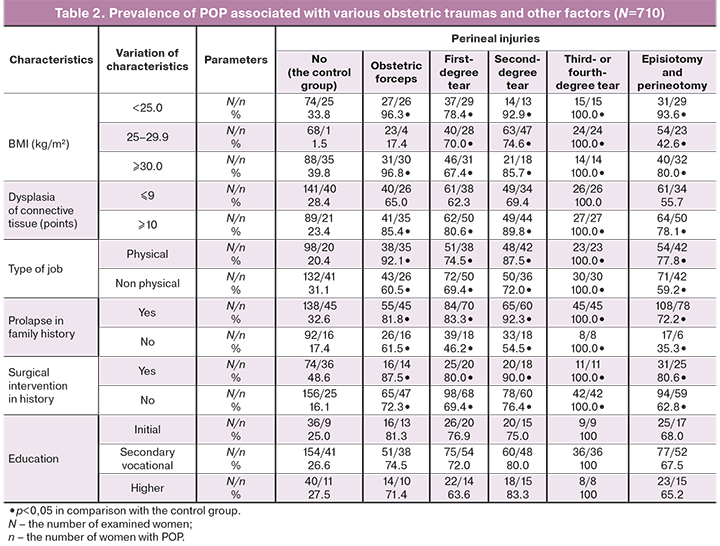
POP was found in all women with third- or fourth-degree perineal tear. In women without obstetric traumas, the incidence of POP ranged from 1.5% (group with BMI 25-29.9 kg/m2) to 48.6% (a group of women with surgical intervention in medical history) depending on medical and demographic characteristics. Obviously, the groups with body mass index 25–29.9 kg/m², who had no obstetric traumas in history, had a minimal risk of POP. The risk of developing POP was similar in the groups of women with different educational level (p> 0.05).
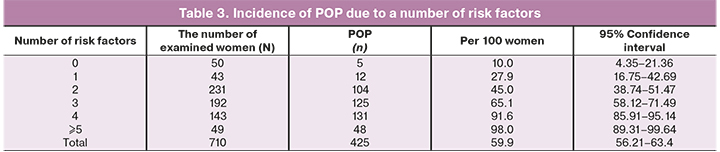
Distribution of women according to risk factors showed that only a small proportion of them had no risk factors for POP in history (50/710; 7%). The largest number of women had 2 and 3 risk factors in history (32.5 and 27.0%, respectively). Table 3 shows the incidence of POP due to a number of risk factors. It is evident from these data that the incidence of POP increases proportionally with an increase in the number of risk factors.
Discussion
According to published studies, prevalence of POP varies widely and changes depending on many factors (congenital connective tissue dysplasia, age-related changes in female body, aggravated obstetric history, giving birth multiple times, obesity, heavy physical job and other [1–5]. Obstetric traumas of different types (forceps delivery or vacuum extractor delivery, first-, second-, third-, fourth-degree perineal tears, as well as perineal excision) in women without the presence of these factors are associated with the increased risk and prevalence of POP. A combination of these factors and obstetric traumas in history even more increases the risk of developing POP. In the absence of studied risk factors in the medical histories, POP was detected in 10.0% of women. The presence of one or more risk factors in medical history was associated with the proportional increase in prevalence of POP from 27.8% to 98.0%. The phenomenon of combination of risk factors for POP is noteworthy: only a small proportion of women had no risk factors in history (50/710; 7%). Most women had 2 or 3 risk factors in history (32.5% and 27,0%, respectively). Grouping of women according to the combination of risk factors of POP can be used for differential observation of women with purpose of early identification of risk factors.
Conclusion
1. The prevalence of pelvic organ prolapse in population was 59.9%; at the same time, the development of this condition varies depending on the absence (26.5%) or presence (67.2%–100%) of obstetric traumas in medical history and correlates with the severity degree.
2. A combination of risk factors plays an important role in development of POP compared to any of these factors separately. An increase in the absolute number of risk factors proportionally increases the risk of developing this condition.
References
- Barber M.D., Maher C. Epidemiology and outcome assessment of pelvic organ prolapse. Int. Urogynecol. J. 2013; 24(11): 1783-90. https://dx.doi.org/10.1007/s00192-013-2169-9.
- Jokho A.H., Rizvi R.M., MacArthur C. Prevalence of pelvic organ prolapse in women, associated factors and impact on quality of life in rural Pakistan: Population Based Study. BMC Women’s Health. 2020; 20(1): 82. https://dx.doi.org/10.1186/s12905-020-00934-6.
- Yuk J.S., Lee J.H., Hur J.Y., Shin J.H. The prevalence and treatment pattern of clinically diagnosed pelvic organ prolapse: a Korean National Health Insurance Database-based cross-sectional study 2009-2015. Sc. Rep. 2018; 8(1):1334. https://dx.doi.org/10.1038/s41598-018-19692-5.
- Аскерова М.Ш., Рзакулиева Л.М. Распространенность и факторы риска выпадения женских половых органов у жительниц г. Баку. Казанский медицинский журнал. 2018; 99(2): 187-94. [Askerova M.Sh., Rzakulieva L.M. Prevalence and risk factors of prolapse of female genital organs in residents of Baku. Kazan Medical Journal. 2018; 99(2): 187-94. (in Russian)].
- Гвоздев М.Ю., Тупикина Н.В., Касян Г.Р., Пушкарь Д.Ю. Пролапс тазовых органов в клинической практике врача уролога. Методические рекомендации №3. М.; 2016. [Gvozdev M.Yu., Tupikina N.V., Kasyan G.R., Pushkar D.Yu. Pelvic organ prolapse in the clinical practice of a urologist. Methodical recommendations No. 3. Moscow; 2016. (in Russian)].
- Барсуков А.Н., Пересади О.А., Куликов А.А. Пролапс тазовых органов у женщин: современное состояние проблемы. Медицинская панорама. 2011; 6: 21-8. [Barsukov A.N., Peresadi O.A., Kulikov A.A. Pelvic organ prolapse in women: current state of the problem. Medical panorama. 2011; 6: 21-8. (in Russian)].
- Vergeldt T.F.M., Weemhoff M., Inthou T.J, Kluivers K. Risk factors for pelvic organ prolapse and its recurrence a systematic review. Int. Urogynecol. J. 2015; 26(11): 1359-73. https://dx.doi.org/10.1007/s00192-015-2695-8.
- Rogowski A., Bienkowski P., Tarwacki D., Dziech E., Samochowiec J., Jerzak M., Baranowski W. Association between metabolic syndrome and pelvic organ prolapsed severity. Int Urogynecol J. 2015; 26(4): 563-8. https://dx.doi.org/10.1007/s00192-014-2468-9.
- Hagen S., Stark D., Dougall I. A survey of prolapse practice in UK women’s health physiotherapists: what has changed in the last decade? Int Urogynecol J. 2016; 27(4): 579-85. http://dx.doi.org/10.1007/s00192-015-2864-9.
- Lyatoshinskaya P., Gumina D., Popov A., Koch M., Haymann M. Knowledge of pervic organ prolapse in patients and their information-seeking preferences: comparing Vienna and Moscow. Int. Urogynecol. J. 2016; 27(11): 1673-80. https://dx.doi.org/10.1007/s00192-016-3018-4.
- Смольнова Т.Ю., Адамян Л.В. Клинико-патогенетические аспекты опуще-ния и выпадения внутренних половых органов при недифференциро-ванных формах дисплазии соединительной ткани. Кубанский научный медицинский вестник. 2009; 6: 69-73. [Smolnova T.Yu., Adamyan L.V. Clinical and pathogenetic aspects of prolapse and prolapse of internal genital organs in undifferentiated forms of connective tissue dysplasia. Kuban Scientific Medical Bulletin. 2009; 6: 69-73. (in Russian)].
- Гланц С. Медико-биологическая статистика. Пер. с англ. М.: Практика; 1998. 459 с. [Glantz S. Biomedical statistics. Transl. from English. M.: Practice. 1998. 459 p. (in Russian)].
Received 18.01.2021
Accepted 18.05.2021
About the Authors
Minara Shain Askerova, the author of dissertation, Department of Obstetrics and Gynecology, A. Aliev Azerbaijan State Institute for the Improvement of Doctors; obstetrician-gynecologist, Maternity Hospital No. 2, Baku. E-mail: mirmmms@mail.ru. AZ 1012, Azerbaijan, Baku, Muzaffar Hasanov str., 35.For citation: Askerova M.Sh. The risk of pelvic organ prolapse in women after obstetric traumas.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2021; 6: 80-84 (in Russian)
https://dx.doi.org/10.18565/aig.2021.6.80-84



