Исход беременности, особенно при ее патологическом течении или при наличии неблагоприятного отягощенного преморбидного фона, в разрезе анализа эффективности деятельности родовспомогательной службы напрямую зависит от качества оказываемой медицинской помощи. Итоги оказания медицинской помощи женщинам при беременности, в родах и в послеродовом периоде, а также новорожденным определяют прогнозируемые возможности снижения материнской смертности (МС), являющейся интегральным показателем уровня развития системы здравоохранения в государстве в целом [1–6].
В настоящее время наряду с показателями перинатальных потерь и МС, входящими в структуру индикаторов оценки качества родовспомогательной медицинской службы, особое внимание уделяется индикатору, характеризующему «материнскую заболеваемость, едва не лишившую женщину жизни» (near miss maternal morbidity), – т.н. near miss. По определению ВОЗ, «near miss» – это женщины, которые были при смерти, но выжили после осложнения, случившегося во время беременности, родов или в течение 42 дней после окончания беременности» [3, 7, 8]. Т.е., по сути, случаи near miss отличаются от случаев МС только благоприятным клиническим исходом (несостоявшийся летальный исход).
Критические акушерские состояния (КАС) – это заболевания, синдромы и симптомы, требующие проведения мероприятий по реанимации и интенсивной терапии женщин в период беременности и в течение 42 дней после ее окончания. Таким образом, если случай near miss возникает только после того, как женщина вышла из состояния, угрожающего жизни, то случай КАС – с момента его возникновения. В случаи КАС входят как благоприятные исходы, так и случаи, завершившиеся смертью женщины.
Перманентный мониторинг случаев КАС в родовспомогательных медицинских организациях (МО) позволяет не только объективно оценить качество оказываемой медицинской помощи, но и выявить наиболее значимые факторы, приводящие к случаям near miss и МС. В плоскости поиска решения этой задачи находятся не только чисто медицинские (квалификация медицинского персонала, знание современных клинических протоколов лечения, владение необходимыми профессиональными компетенциями и т.д.), но и организационно-методические (координация работы амбулаторного и стационарного звеньев, четкая маршрутизация, функционирование трехуровневой системы оказания помощи и т.д.), демографические (миграционный прирост населения, неудовлетворительные семейные отношения, высокий паритет и т.д.), а также социально-экономические (низкий социальный статус, низкий уровень валового продукта федерального округа (области, города) и т.д.) причины [2, 5, 9–12].
Мониторинг случаев КАС является одним из наиболее эффективных инструментов выявления жизнеугрожающих состояний, позволяющих обеспечить своевременную медицинскую эвакуацию в МО акушерско-гинекологического профиля III уровня и предупреждение возникновения случаев МС и near miss. Последующий анализ случаев жизнеугрожающих состояний позволяет изучать наибольший массив наблюдений; последствия врачебных ошибок – проводить оценку качества медицинской помощи.
Анализ выявленных дефектов оказания медицинской помощи должен быть использован для повышения профессиональных компетенций при оказании медицинской помощи надлежащего качества [6].
Анализ случаев near miss в субъектах Российской Федерации (РФ), в т.ч. в Санкт-Петербурге, проводится с 2013 г., является важным звеном в профилактике МС, способствует лучшему пониманию механизмов развития связанных с беременностью КАС, детальной оценке качества медицинской помощи и причин ненадлежащего ее оказания с целью определения путей оптимизации исходов беременности [2, 6, 7, 11–13]. С 2021 г. мониторинг КАС осуществляется на основе Регистра КАС вертикально-интегрированной медицинской информационной системы по профилям «Акушерство и гинекология» и «Неонатология» (ВИМИС «АКиНЕО»), что позволило впервые провести аудит случаев near miss из числа зарегистрированных КАС и свидетельствует о выходе на новый качественный уровень разработки мер, направленных на снижение МС.
Цель исследования: проведение анализа мониторинга случаев КАС в родовспомогательных МО Санкт-Петербурга в 2021 г. в соответствии с Регламентом мониторинга КАС в РФ, на основе Порядка оказания медицинской помощи по профилю «акушерство и гинекология», а также аудита случаев near miss в соответствии с письмом Минздрава РФ № 15-4/383 от 11.03.2021 «О методических подходах к оценке и анализу критических состояний (near miss) на основании критериев ВОЗ» из числа случаев КАС, выявленных в ходе мониторинга КАС [2, 14, 15].
Материалы и методы
В Санкт-Петербурге система оказания специализированной медицинской помощи женщинам в период беременности, родов и в послеродовом периоде в 2021 г. представлена 20 МО (табл. 1).

В проведенном анализе случаев КАС, а также при аудите случаев near miss и МС представлены результаты работы службы родовспоможения в Санкт-Петербурге в разрезе профилактики МС в период пандемии новой коронавирусной инфекции (НКИ) COVID-19 в 2021 г. с целью ее объективной оценки в условиях сложной эпидемиологической обстановки, поиска возможных механизмов улучшения реализации главной цели современного перинатального акушерства – рождение здорового потомства и сохранение репродуктивного здоровья женщины.
Систематический сбор информации из всех МО акушерско-гинекологического профиля II и III уровней Санкт-Петербурга и ее дальнейшая передача на федеральный уровень (система информационной вертикальной координации) через Регистр КАС ВИМИС «АКиНЕО» в 2021 г. осуществлялись акушерским дистанционным консультативным центром (АДКЦ) СПбГБУЗ «Городской перинатальный центр № 1» в качестве т.н. «якорной» МО. Это, безусловно, позволило достаточно оперативно обеспечить эффективность регистрации и мониторинга случаев КАС в режиме real-time в Санкт-Петербурге.
В ходе анализа все случаи КАС разделены на 12 основных групп на основе идентификационных критериев [https://nsi.rosminzdrav.ru/#!/refbook/1.2.643.5.1.13.13.99.2.774/version/1.1] (табл. 2).
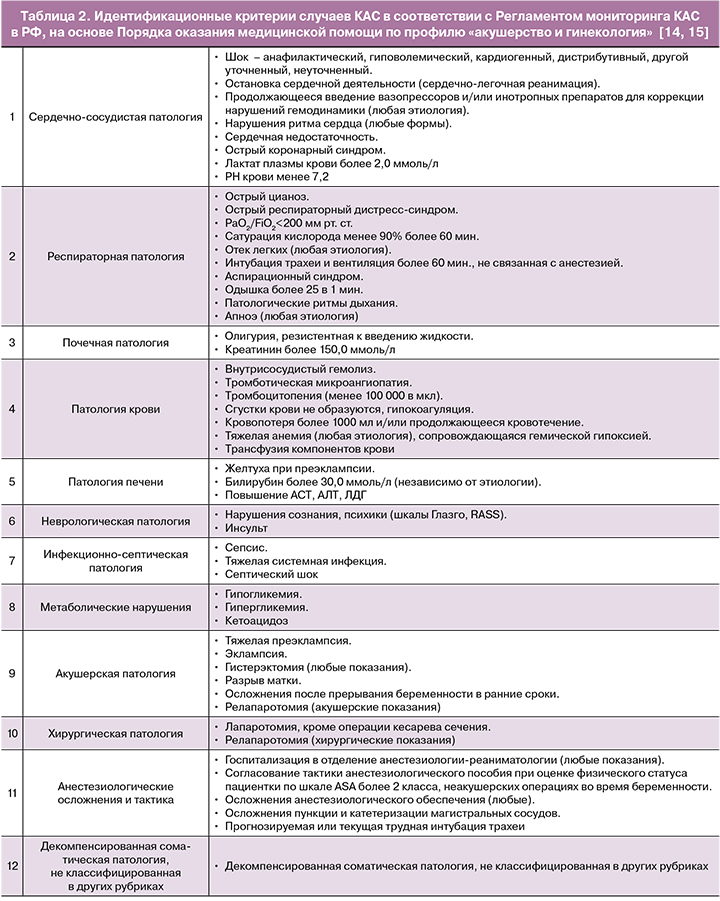
Идентификационные критерии случаев near miss по группам органной дисфунции (7 групп) на основе диагностических критериев ВОЗ представлены в таблице 3.
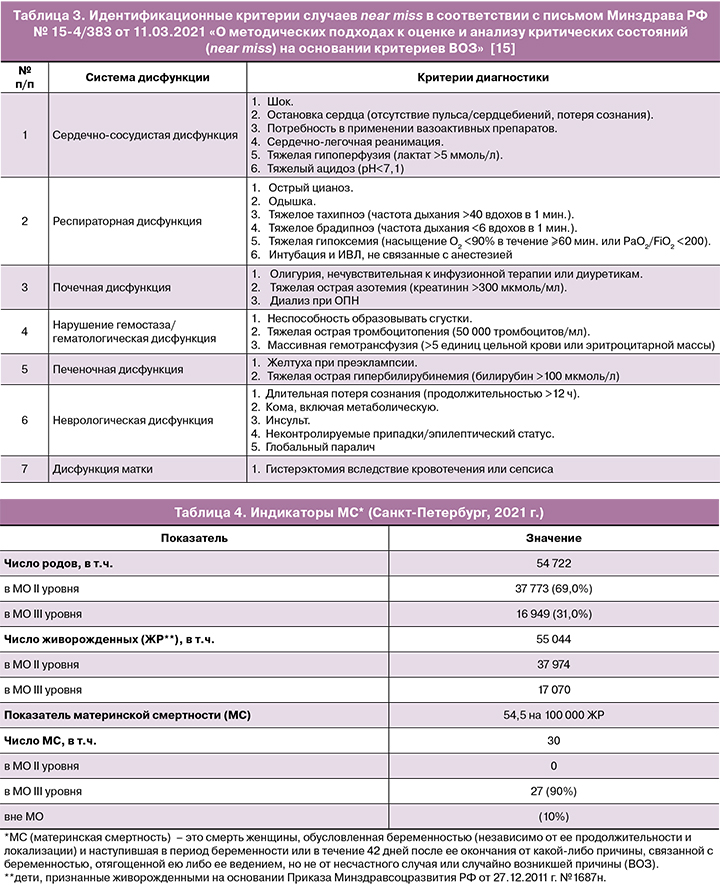
С 2018 г. в Санкт-Петербурге, так же как и во всей РФ, продолжается прогрессивное снижение количества родов. В 2021 г. в Санкт-Петербурге, по оперативным данным родовспомогательных МО, состоялось 54 722 родов, родились 55 044 живорожденных детей, что на 591 (1,1%) родов и на 942 (1,7%) живорожденных новорожденных меньше, чем за 2020 г. (за 12 месяцев 2020 г. состоялось 55 313 родов, родились 55 986 живорожденных детей). При этом в МО II уровня состоялось 37 773 родов и родились 37 974 живорожденных, а в МО III уровня – 16 949 родов и родились 17 070 живорожденных.
В 2021 г. в Санкт-Петербурге по данным Росстата, а также подсистемы «Учет медицинских свидетельств о рождении и смерти» государственной информационной системы Санкт-Петербурга «Региональный фрагмент единой государственной информационной системы в сфере здравоохранения» (СПбГБУЗ «Медицинский информационно-аналитический центр» (МИАЦ)) зарегистрировано 30 случаев МС (12 – в 2020 г.).
По результатам отчета АДКЦ на базе СПбГБУЗ «Городской перинатальный центр № 1» в Санкт-Петербурге в 2021 г. зарегистрировано 449 случев КАС, вошедших в Регистр КАС ВИМИС «АКиНЕО». Из них 229 случаев (51,0%) произошли в МО II группы (родильные дома и акушерско-гинекологические отделения многопрофильных стационаров), 217 случаев (49,0%) – в МО III группы оказания акушерско-гинекологической помощи (перинатальные центры городского и федерального подчинения, акушерско-гинекологические клиники федерального подчинения, гинекологические отделения многопрофильных стационаров, не оказывающих специализированную акушерскую помощь). По акушерскому статусу среди зарегистрированных КАС преобладали родильницы. Благоприятный исход беременности и родов составил в общем 93,3% случая: на 449 случаев КАС зарегистрировано 30 случаев МС, 3 из которых произошли вне МО (табл. 4).
Результаты и обсуждение
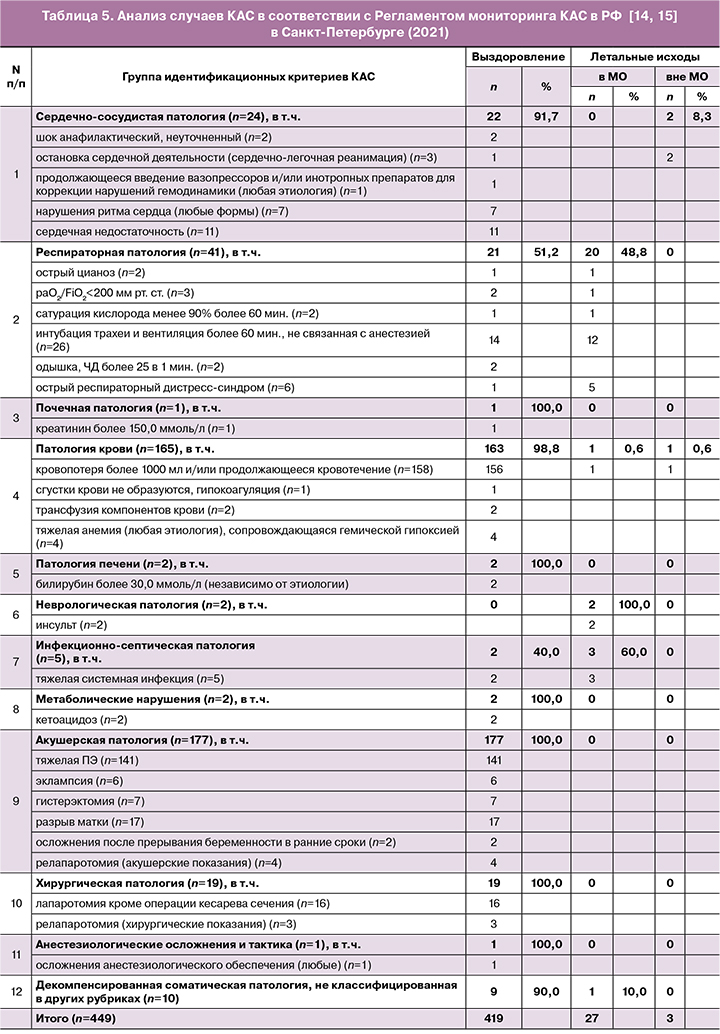
Анализ случаев КАС в соответствии с Регламентом мониторинга КАС в РФ приведен в таблице 5.
По данным Бюллетеня Регистра КАС ВИМИС «АКиНЕО», в РФ за 2021 г. всего было зарегистрировано 8259 случаев КАС, 1055 из них зарегистрированы в Северо-Западном федеральном округе (СЗФО) РФ (12,8% общего числа), из которых 449 (42,6% числа зарегистрированных в СЗФО) – в Санкт-Петербурге (5,4% общего числа в РФ). Структура наиболее часто регистрируемых КАС в РФ в 2021 г. представлена следующими группами:
- акушерская патология (тяжелая преэклампсия/эклампсия – 31,4% случаев, гистерэктомия – 2,6% случаев);
- патология крови (кровопотеря более 1000 мл и/или продолжающееся кровотечение – 24,6% случаев);
- респираторная патология (КАС, ассоциированные с НКИ COVID-19, – 22,8% случаев).
Как следует из приведенных данных, структура наиболее часто регистрируемых КАС в Санкт-Петербурге в 2021 г. представлена следующими группами:
- акушерская патология (39,4% общего числа КАС), в т.ч.:
- тяжелая преэклампсия и эклампсия (83,1% в группе и 32,7% общего числа КАС);
- патология крови (36,7% общего числа КАС), в т.ч.:
- кровопотеря более 1000 мл и/или продолжающееся кровотечение (95,8% в группе и 35,2% общего числа КАС);
- респираторная патология (9,1% общего числа КАС), в т.ч.:
- интубация трахеи и вентиляция более 60 минут, не связанная с анестезией (63,4% в группе и 5,8% общего числа КАС);
- сердечно-сосудистая патология (5,4% общего числа КАС);
- хирургическая патология (4,2% общего числа КАС).
По результатам анализа представленных объективных данных необходимо отметить:
- отсутствие случаев МС в родовспомогательных МО из групп, наиболее часто регистрируемых КАС: акушерская патология, в т.ч. тяжелая преэклампсия, эклампсия, разрыв матки; хирургическая патология;
- практически сопоставимо равная частота регистрации случаев КАС в Санкт-Петербурге по сравнению с общими данными в РФ по идентификационным критериям «тяжелая преэклампсия, эклампсия»: 32,7 и 31,4% соответственно;
- низкая частота выполнения гистерэктомии (критерий КАС из группы «акушерская патология»): 2,6% в целом по РФ и в 1,6% случаев в Санкт-Петербурге;
- низкая частота (1,2%, n=2) случаев МС из группы КАС «патология крови» (идентификационный критерий «кровопотеря более 1000 мл и/или продолжающееся кровотечение»): 1 случай зарегистрирован в МО III уровня, причиной которого явился геморрагический шок вследствие прервавшейся эктопической беременности; 1 случай МС в родах зарегистрирован вне МО, вследствие массивной акушерской кровопотери – неполное предлежание плаценты и разрыв пуповинных сосудов при их краевом прикреплении.
В 2021 г. в Санкт-Петербурге с учетом пандемии НКИ COVID-19 регистрация случаев КАС группы «респираторная патология» составила 9,1% общего числа КАС при наличии 20 летальных исходов в МО III уровня, вследствие тяжелого или крайне тяжелого течения двусторонних вирусных или вирусно-бактериальных пневмоний, острого респираторного дистресс-синдрома или тромбоэмболии легочной артерии вследствие НКИ COVID-19 (O98.5, U07.1).
В группе КАС «сердечно-сосудистая патология» (5,4% общего числа КАС) на 22 случая КАС с благоприятным клиническим исходом (4,9% общего числа КАС и 91,7% в группе) зарегистрировано 2 случая МС («остановка сердечной деятельности (сердечно-легочная реанимация)»), произошедших вне МО, не связанных с прямыми акушерскими причинами и являющихся неуправляемыми (непредотвратимыми) (8,3% в группе):
- аортоартериит с формированием мешковидной аневризмы надклапанной части аорты и ее разрывом (разрыв аневризмы грудного отдела аорты, гемотампонада перикарда) (О99.4, I.71.1, I 31.2) – случай МС при беременности вне МО;
- острая сердечно-сосудистая недостаточность на фоне острого респираторного дистресс-синдрома вследствие НКИ COVID-19, осложненной двусторонней внегоспитальной полисегментарной вирусной пневмонией с диффузным альвеолярным повреждением легких (пролиферативная фаза) (O98.5, U07.1) – случай МС на 24-е сутки послеродового периода до приезда СМП.
Анализ случаев near miss (n=72) в Санкт-Петербурге в 2021 г. по группам органной дисфункции на основе диагностических критериев ВОЗ (2011) [15], а также анализ случаев МС (n=30) проводится с учетом индикаторов аудита near miss и МС. К индикаторам аудита случаев near miss и МС относят [15]:
- коэффициент near miss: число случаев near miss/число живорожденных × 1000;
- коэффициент жизнеугрожающих состояний: число случаев near miss+число случаев МС/число живорожденных × 1000;
- индекс выживаемости: число случаев near miss/число случаев МС;
- индекс смертности: число случаев МС/число случаев near miss+число случаев МС × 100.
Проведенный анализ индикаторов аудита near miss и МС показал: коэффициент near miss составил 1,3, коэффициент жизнеугрожающих состояний – 1,9, индекс выживаемости – 2,4:1, а индекс смертности – 29,4.
Заключение
Перманентный мониторинг КАС в режиме real-time через Регистр КАС ВИМИС «АКиНЕО» (АДКЦ «якорной» МО СПбГБУЗ «Городской перинатальный центр № 1»), внедренный в повседневную работу МО родовспомогательного профиля, постоянный контроль со стороны главного внештатного специалиста по акушерству и гинекологии Комитета по здравоохранению Правительства Санкт-Петербурга, а также эффективное взаимодействие с Федеральным дистанционным консультативным центром НМИЦ акушерства, гинекологии и перинатологии им. акад. В.И. Кулакова являются важными и эффективными звеньями работы родовспомогательной службы по профилактике МС. Кроме того, мониторинг случаев КАС и аудит случаев near miss позволяет провести детальную оценку характера и качества медицинской помощи с целью улучшения исходов беременностей.
В целом полноценная и своевременная регистрация случаев КАС в Регистре КАС ВИМИС «АКиНЕО» позволяет:
- создать единое оперативное информационное пространство, реализованное в режиме реального времени, для специалистов, непосредственно оказывающих медицинскую помощь пациенткам с жизнеугрожающими состояниями (КАС/near miss) в акушерской практике, специалистов АДКЦ и профильного НМИЦ, а также для организаторов здравоохранения на уровне субъекта, федерального округа и всей страны;
- проводить эффективный мониторинг случаев КАС и аудит случаев near miss с целью повышения эффективности оказания медицинской помощи по родовспоможению путем реализации проведения комплексного междисциплинарного медицинского консилиума в кратчайшие сроки, с использованием системы телекоммуникационных технологий с привлечением специалистов МО, непосредственно оказывающей медицинскую помощь, акушерских региональных дистанционных центров и федеральных МО по профилю заболевания;
- оперативно получать данные о состоянии и нагрузке акушерско-гинекологической службы региона в разрезе оказания медицинской помощи пациенткам с жизнеугрожающими состояниями (КАС/near miss);
- проводить анализ эффективности организации оказания медицинской помощи пациенткам с КАС/near miss.
Частота случаев КАС, зарегистрированных в МО II уровня оказания акушерско-гинекологической помощи, составила 51,0%, а в МО III уровня – 49,0%, в то время как аудит случаев near miss показал, что 12,5% из них произошли в МО II уровня, а 83,3% – в МО III уровня.
Структура и частота наиболее часто регистрируемых групп КАС в Санкт-Петербурге в 2021 г., представленная группами «акушерская патология», «патология крови» и «респираторная патология», сопоставима с данными регистрации КАС в РФ.
Лидирующее место в структуре регистрации КАС занимает группа «акушерская патология» (39,4% общего числа КАС) при отсутствии случаев МС. Второе место в структуре регистрации КАС занимает группа «патология крови» (36,8% общего числа КАС) с регистрацией двух случаев МС, которые идентифицированы по критерию «кровопотеря более 1000 мл и/или продолжающееся кровотечение» (95,8% в группе).
В 2021 г. в условиях пандемии НКИ COVID-19 в Санкт-Петербурге был зарегистрирован 41 случай КАС «респираторная патология» (9,1% общего числа КАС), из которых 39 были идентифицированы как случаи near miss («респираторная дисфункция»), что составило 54,2% общего числа случаев near miss при наличии 20 случаев летальных исходов в МО III уровня вследствие тяжелого или крайне тяжелого течения двусторонних вирусных или вирусно-бактериальных пневмоний, осложнившихся острым респираторным дистресс-синдромом или тромбоэмболией легочной артерии вследствие НКИ COVID-19 (O98.5, U07.1).
Недостаточный уровень достижения целевых показателей индикаторов аудита near miss и МС демонстрирует необходимость более углубленного сравнительного анализа и аудита таких случаев с выявлением факторов, способствующих предупреждению МС, с дальнейшим их использованием при разработке комплекса мер, направленных на предотвращение случаев МС.