Prediction of pregnancy outcomes in patients with cervical insufficiency undergoing cervical cerclage
Pesegova S.V., Timokhina E.V., Strizhakov A.N., Ignatko I.V., Belousova V.S., Anokhina V.M.
Objective: To assess the clinical significance of interleukin (IL-6 and IL-8, and matrix metalloproteinase-8 (MMP-8) in predicting pregnancy outcomes in patients with cervical insufficiency (CI) undergoing cervical cerclage. Materials and methods: This prospective cohort study included 67 pregnant women with CI. Women were divided into two groups based on the timing of their subsequent deliveries. Group 1 comprised 30 (44.8%) pregnant women who gave birth before 32 weeks, whereas Group 2 included 37 (55.2%) women who gave birth after 32 weeks. During the vaginal speculum examination, cervical mucus was collected from the cervical canal before the cerclage procedure to determine the concentrations of IL-6, IL-8, and MMP-8. Results: In Group 1, the concentrations of IL-6, IL-8, and MMP-8 were 12.3 pg/ml, 261.0 pg/ml, and 28.5 ng/ml, respectively. In Group 2, the concentrations were 6.4 pg/ml, 102.3 pg/ml, and 12.3 ng/ml for IL-6, IL-8, and MMP-8, respectively. The threshold values for each marker were determined by ROC analysis. The threshold concentrations at the cut-off point were 11.3 pg/ml, 202.6 pg/ml, and 22.3 ng/ml for IL-6, IL-8, and MMP-8, respectively. Conclusion: Our study revealed that in patients with CI who delivered after 32 weeks, the levels of immunological markers were significantly higher than those in patients who delivered later. Unfavorable pregnancy outcomes with delivery before 32 weeks of gestation were predicted at levels of IL-6, IL-8, and MMP-8 ≥ 11.3 pg/ml, ≥ 202.6 pg/ml, and ≥ 22.3 ng/ml, respectively. Cervical cerclage is considered ineffective in these patients.
Authors' contributions: Timokhina E.V., Ignatko I.V., Strizhakov A.N., Pesegova S.V. – conception of the study; Timokhina E.V., Pesegova S.V., Belousova V.S. – data collection, drafting of the manuscript; Timokhina E.V., Ignatko I.V. – reviewing and editing of the manuscript; Pesegova S.V., Anokhina V.M. – statistical analysis and visualization.
Conflicts of interest: The authors have no conflicts of interest to declare.
Funding: This study did not receive any funding.
Ethical Approval: The study was reviewed and approved by the Research Ethics Committee of the I.M. Sechenov First Moscow State Medical University of Ministry of Health of Russia (Sechenov University) (Ref. No. 31-20).
Patient Consent for Publication: All patients provided informed consent for the publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available upon request from the corresponding author after approval from the principal investigator.
For citation: Pesegova S.V., Timokhina E.V., Strizhakov A.N., Ignatko I.V., Belousova V.S., Anokhina V.M. Prediction of pregnancy outcomes in patients with cervical insufficiency undergoing cervical cerclage. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2023; (10): 119-125 (in Russian) https://dx.doi.org/10.18565/aig.2023.159
Keywords
Cervical insufficiency (CI) complicates approximately 0.5–1% of all pregnancies and accounts for 15–40% of cases of spontaneous abortion and very early preterm birth (PB) [1–5]. Cervical cerclage is considered the "gold standard" for the treatment of CI [6, 7]. With the use of cervical cerclage, pregnancy can be prolonged in approximately 72% of cases, thereby reducing neonatal morbidity and mortality [8, 9].
It has been established that one of the causes of CI and the development of spontaneous PB is intra-amniotic inflammation [10]. This inflammation can be aseptic (caused by immune molecules known as alarmins) or associated with a microbial agent and its invasion into the amniotic cavity [6, 11]. Intra-amniotic infection is detected in more than half of the cases where amniocentesis is performed in patients with CI [6, 12–14].
In patients with progressive intra-amniotic inflammation, cervical cerclage may yield unsatisfactory results owing to the development of chorioamnionitis, premature rupture of membranes, and premature termination of pregnancy [6].
Despite the widespread use of cervical cerclage in patients with CI, predictors of successful surgical treatment remain poorly understood. The most accurate method for predicting success during cervical cerclage is the determination of infectious and inflammatory markers in amniotic fluid obtained through amniocentesis. For instance, the levels of interleukins IL-6 and IL-8, matrix metalloproteinase-8 (MMP-8), and tissue inhibitor of metalloproteinases in amniotic fluid reflect the development of intra-amniotic inflammation [15, 16].
However, amniocentesis is an invasive procedure, with premature rupture of membranes and termination of pregnancy as the main complications. Therefore, the use of this diagnostic modality is limited in everyday clinical practice [16].
The search for non-invasive markers to identify the presence of intra-amniotic inflammation may hold clinical significance in developing an appropriate patient management strategy and guiding the choice of the CI correction method (cervical cerclage, obstetric pessary, or conservative management).
The objective of this study was to evaluate the clinical significance of IL-6, IL-8, and MMP-8 levels in cervical secretions in predicting pregnancy outcomes after cervical cerclage.
Materials and methods
This prospective study included 67 women with singleton pregnancies who were diagnosed with CI between 18 and 26 weeks of gestation and underwent cervical cerclage.
All pregnant women were observed in the Department of Pregnancy Pathology at the Perinatal Center of the S.S. Yudin City Clinical Hospital from 2020 to 2022.
CI was diagnosed based on medical history, bimanual examination, and ultrasound data (shortened cervical length < 25 mm and/or cervical dilation >10 mm). An analysis of the course and outcomes of pregnancy was carried out from the moment the diagnosis of CI was made upon admission of the pregnant woman to the maternity hospital and until delivery.
The study included an analysis of the characteristics of the obstetric and gynecological history, course of pregnancy, childbirth, and postpartum period, as well as the condition of newborns.
The study included women over 18 years of age with a singleton pregnancy with a cervical length according to ultrasound of ≤ 25 mm and/or dilation of the internal os >10 mm, 18–26 weeks gestational age at the time of CI correction, correction of CI using cervical cerclage, and written informed consent to participate in the study.
The exclusion criteria were multiple pregnancies, history of surgical interventions on the cervix, prolapse of the membranes into the cervical canal, acute phase or exacerbation of chronic infectious diseases, clinical signs of chorioamnionitis at the time of CI correction, and patient refusal to participate in the study.
Cervical mucus was collected from all patients using a sterile soft universal probe before cervical cerclage during speculum cervical examination. The probe was inserted into the cervical canal and rotated 2 times clockwise and then 2 times counterclockwise. The probe tip was then placed in an Eppendorf tube containing 1 mL buffer solution. After collection, the tubes were centrifuged and frozen at -40°C until testing.
The concentrations of IL-6, IL-8, and MMP-8 in the cervical mucus were determined using an enzyme-linked immunosorbent assay (ELISA) (Thermo Fisher Scientific, USA).
The study was reviewed and approved by the Research Ethics Committee of the I.M. Sechenov First Moscow State Medical University, Ministry of Health of Russia (Sechenov University) (Ref. No: №31-20).
Statistical analysis
Statistical analysis was performed using the StatTech v. 2.8.5 software (Stattech LLC, Russia). The distribution of continuous variables was tested for normality using the Shapiro–Wilk test (for the number of subjects < 50) or the Kolmogorov–Smirnov test (for the number of subjects > 50). Quantitative variables showing a normal distribution were expressed as mean (M), standard deviation (SD), and 95% confidence interval (95% CI). If numerical variables were not normally distributed, they were reported as the median (Me) and lower and upper quartiles (Q1 and Q3). Categorical data were presented as counts and percentages. Normally distributed continuous variables with equal variances were compared between the two groups using Student's t-test; in the case of unequal variances, Welch's test was used. A nonparametric Mann–Whitney test was used to compare numerical data with a non-normal distribution. Comparisons of percentages were performed using Fisher's exact test for two-by-two contingency tables when the expected frequency of one or more cells was < 10). Comparisons of percentages in multi-way contingency tables were performed using Pearson’s chi-squared test. ROC curve analysis was performed to assess the diagnostic significance of quantitative characteristics in predicting a specific outcome. The optimal cut-off value was calculated using the Youden index. Differences were considered statistically significant at p<0.05.
Results
In accordance with these criteria, we conducted a prospective analysis of the course and outcomes of pregnancy in 67 patients hospitalized in the pregnancy pathology department with signs of CI and its correction by cervical cerclage.
The median patient age was 31.0 years.
The period for correction of CI with cervical cerclage, as well as the period for collecting material from the cervical canal for research, averaged 21.9 (1.3) weeks of gestation (min–max 19.0–25.0). At the same time, the median length of the cervix according to transvaginal ultrasound was 21.0 mm (Q1–Q3 18.2–22.0; min–max 13.0–25.0).
Among the patients, 12/67 (17.9%) were primigravida and 55/67 (82.1%) were multigravida. At the same time, 40/67 (59.7%) women had their first birth, 27/67 (40.3%) pregnant women had a second birth, and 43/67 (64.2%) patients had a complicated obstetric and gynecologic history (COGH).
Upon hospital admission, all women were examined according to the clinical protocol. If the bacteriological examination revealed an inflammatory smear and/or opportunistic microflora of 104 or more, vaginal cleansing and antibacterial treatment were performed according to antibiotic susceptibility, and then CI was corrected by cervical cerclage.
During follow-up, all patients were divided into 2 groups according to gestational age at delivery. Group 1 consisted of 30 pregnant women (44.8%) with birth occurring before 32 weeks of gestation, and group 2 included 37 women (55.2%) with delivery after 32 weeks of gestation. The criterion for separation was 32 weeks' gestational age at delivery because clinical observations have shown more favorable obstetric and perinatal outcomes at delivery after 32 weeks of gestation. The clinical and anamnestic characteristics of patients are shown in Table 1. The patients in both groups were comparable in terms of their main clinical and anamnestic characteristics.

It should be noted that patients born before 32 weeks of gestation were significantly more likely to have a complicated reproductive history (p=0.031) in the context of high parity.
The index pregnancy ended preterm in 58.2% of patients. The median gestational age at delivery was 33.0 weeks (Q1–Q3: 26.0–38.0).
The distribution by gestational age at delivery was as follows: very early PB occurred in 21/67 (31.3%) pregnant women, early PB in 9/67 (13.4%), and PB in 9/67 (13.4%) women. Pregnancy ended in term delivery in 28/67 (41.8%) patients. All the patients underwent vaginal delivery.
Cervical mucus samples collected prior to CI correction with cervical cerclage were analyzed by ELISA for the measurement of IL-6, IL-8, and MMP-8 in all women.
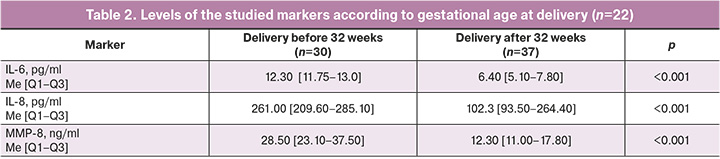
The levels of the studied markers at the time of cervical cerclage were significantly higher in patients who delivered before 32 weeks than in those who delivered after 32 weeks of gestation (Table 2).
Using ROC analysis, we determined the threshold concentrations of the studied markers for predicting childbirth before 32 weeks of pregnancy (Figure).
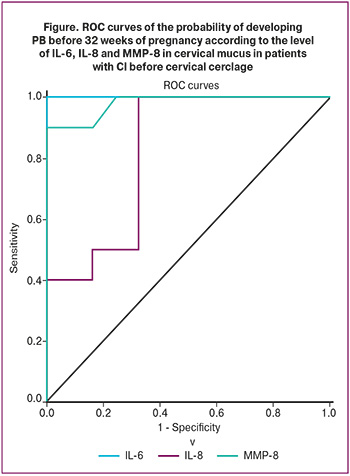
Cervical IL-6 levels ≥11.3 pg/mL predicted delivery before 32 weeks' gestation with 100% sensitivity and specificity (area under the ROC curve, 1.000±0.000 with 95% CI:1.000–1.000; p<0.001).
IL-8 levels of ≥202.6 pg/mL in the cervical canal predicted delivery before 32 weeks' gestation with a sensitivity of 67.6% and a specificity of 100% (area under the ROC curve, 0.822±0.053 with 95% CI:0.717–0.926; p=0.012).
MMP-8 levels ≥22.3 ng/ml in the cervical mucus predicted delivery before 32 weeks. Sensitivity and specificity were 100% and 90%, respectively, and the area under the ROC curve was 0.980±0.019 (95% CI:0.943–1.000, p<0.001).
Discussion
Our study showed that the determination of markers IL-6, IL-8, and MMP-8 in the cervical mucus before cervical cerclage in patients with CI can be useful in clinical practice for predicting unfavorable pregnancy outcomes.
In pregnant women with CI, the presence of intra-amniotic infection/inflammation is prognostically unfavorable, especially when performing cervical cerclage [17]. Intra-amniotic inflammation is associated with increased levels of IL-6 and IL-8. In 2015, Kacerovsky et al. conducted a study that demonstrated a relationship between IL-6 and -8 in cervical mucus with intra-amniotic inflammation and PB [18]. Sakai et al. found that increased levels of IL-8 in cervical mucus, as well as the concentration of neutrophils and lymphocytes in peripheral blood, are predictors of PB in patients undergoing cervical cerclage [19].
We found that in patients with subsequent very early and early PB, the levels of IL-6, -8, and MMP-8 at the time of CI correction were significantly higher than in those with later gestational age at delivery.
Considering the high risk of developing intra-amniotic inflammation in patients with CI, we conducted a pathomorphological study of the placenta after delivery and compared the results with the timing of delivery and the concentrations of markers in the cervical mucus. Pathomorphological examination of the placenta revealed signs of histological chorioamnionitis were found in of 39/67 (58.2%) patients. At the same time, clinical manifestations of chorioamnionitis in the form of fever, inflammatory changes in blood tests, and tachycardia in the fetus were detected in only 9/67 (13.4%) pregnant women. When comparing the results of histological examination with the concentrations of markers in the cervical canal, all patients had comparably high levels of IL-6, -8, and MMP-8 above the threshold values.
Our data indicate that, at the time of CI development, even before its correction by cervical cerclage, there were immunological signs indicating the development of intra-amniotic inflammation. Therefore, threshold values for the concentrations of IL-6 ≥11.3 pg/ml, IL-8 ≥202.6 pg/ml, and MMP-8 ≥22.3 ng/ml in cervical mucus can be recommended as prognostic indicators in patients with CI when deciding to perform cervical cerclage. When the obtained threshold values are exceeded, these markers predict the development of intra-amniotic inflammation/infection and PB. Correction by cervical cerclage was ineffective in these cases.
Conclusion
Levels of IL-6 ≥ 11.3 pg/mL, IL-8 ≥ 202.6 pg/mL, and MMP-8 ≥ 22.3 ng/mL are predictive of an adverse pregnancy outcome with delivery before 32 weeks' gestation and the development of intraamniotic inflammation, regardless of the presence of an infectious agent. Cervical cerclage in these cases is ineffective and is not recommended because of the progression of already existing intra-amniotic inflammation and, as a consequence, the development of very early and early PB, premature rupture of the membranes, and chorioamnionitis.
These patients are recommended to receive micronized progesterone and antibiotic therapy based on the results of bacteriological cultures, taking into account sensitivity. After antibiotic therapy, it is possible to re-examine cervical mucus with the determination of IL-6, IL-8, and MMP-8, and a possible revision of the management strategy with surgical correction of CI while continuing to take micronized progesterone when determining concentrations below those presented.
References
- Thakur M., Mahajan K. Cervical Incompetence. 2021 Jun 9. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan.
- Brown R., Gagnon R., Delisle M.F.; MATERNAL FETAL MEDICINE COMMITTEE. Cervical insufficiency and cervical cerclage. J. Obstet. Gynaecol. Can. 2013; 35(12): 1115-27. https://dx.doi.org/10.1016/S1701-2163(15)30764-7.
- Борщева А.А., Перцева Г.М., Алексеева Н.А. Истмико-цервикальная недостаточность в структуре причин невынашивания беременности. Медицинский вестник Юга России. 2020; 1(1): 34-40. [Borscheva A.A., Pertseva G.M., Alekseeva N.A. Isthmic-cervical insufficiency in the structure of the causes of miscarriage. Medical Herald of the South of Russia. 2020; 1(1): 34-40. (in Russian)]. https://dx.doi.org/10.21886/2219-8075-2020-11-1-24-40.
- Леваков С.А., Боровкова Е.И., Шешукова Н.А., Боровков И.М. Ведение пациенток с истмико-цервикальной недостаточностью. Акушерство, гинекология и репродукция. 2016; 10(2): 64-9. [Levakov S.A., Borovkova E.I., Sheshukova N.A., Borovkov I.M. Management of patients with cervical insufficiency. Obstetrics, Gynecology and Reproduction. 2016; 10(2): 64-9. (in Russian)]. https://dx.doi.org/10.17749/2313-7347.2016.10.2.064-069.
- Беспалова А.Ю., Саргсян Г.С. Выбор метода коррекции истмико-цервикальной недостаточности. Журнал акушерства и женских болезней. 2017; 66(3): 157-68. [Bespalova O.N., Sargsyan G.S. Selection of the method for correction of cervical incompetence. Journal of Obstetrics and Women’s Diseases. 2017; 66(3): 157-68. (in Russian)]. https://dx.doi.org/10.17816/J0WD663157-168.
- Oh K.J., Romero R., Park J.Y., Lee J., Conde-Agudelo A., Hong J.S., Yoon B.H. Evidence that antibiotic administration is effective in the treatment of a subset of patients with intra-amniotic infection/inflammation presenting with cervical insufficiency. Am. J. Obstet. Gynecol. 2019; 221(2): 140.e1-140.e18. https://dx.doi.org/10.1016/j.ajog.2019.03.017.
- Тетруашвили Н.К., Агаджанова А.А., Милушева А.К. Коррекция истмико-цервикальной недостаточности при пролабировании плодного пузыря: возможности терапии. Акушерство и гинекология. 2015; 9: 106-9. [Tetruashvili N.K., Agadzhanova A.A., Milusheva A.K. Correction of isthmicocervical insufficiency in amniotic sac prolapse. Obstetrics and Gynecology. 2015; (9): 106-9. (in Russian)].
- Ehsanipoor R.M., Seligman N.S., Saccone G., Szymanski L.M., Wissinger C., Werner E.F., Berghella V. Physical examination-indicated cerclage: a systematic review and meta-analysis. Obstet. Gynecol. 2015; 126(1): 125-35. https://dx.doi.org/10.1097/AOG.0000000000000850.
- Цхай В.Б. Возможности хирургической коррекции истмико-цервикальной недостаточности при пролабировании плодного пузыря. Акушерство и гинекология. 2016; 9: 5-11. [Tskhai V.B. Possibilities for surgical correction of isthmicocervical insufficiency in fetal bladder prolapse. Obstetrics and Gynecology. 2016; (9): 5-11. (in Russian)]. https://dx.doi.org/10.18565/aig.2016.9.5-11.
- Тетруашвили Н.К., Агаджанова А.А., Милушева А.К. Экстренный серкляж: показания, противопоказания, возможности медикаментозного лечения. Доктор.Ру. 2019; 11: 11-3. [Tetruashvili N.K., Agadzhanova A.A., Milusheva A.K. Urgent cerclage: indications, contraindications, drug therapy. Doctor.Ru. 2019; (11): 11-3. (in Russian)]. https://dx.doi.org/10.31550/1727-2378-2019-166-11-11-13.
- Jung E.Y., Park K.H., Lee S.Y., Ryu A., Joo J.K., Park J.W. Predicting outcomes of emergency cerclage in women with cervical insufficiency using inflammatory markers in maternal blood and amniotic fluid. Int. J. Gynaecol. Obstet. 2016; 132(2): 165-9. https://dx.doi.org/10.1016/j.ijgo.2015.07.011.
- Lee S.E., Romero R., Park C.W., Jun J.K., Yoon B.H. The frequency and significance of intraamniotic inflammation in patients with cervical insufficiency. Am. J. Obstet. Gynecol. 2008; 198(6): 633.e1-8. https://dx.doi.org/10.1016/j.ajog.2007.11.047.
- Lee K.N., Park K.H., Kim Y.M., Cho I., Kim T.E. Prediction of emergency cerclage outcomes in women with cervical insufficiency: еhe role of inflammatory, angiogenic, and extracellular matrix-related proteins in amniotic fluid. PLoS One. 2022; 17(5): e0268291. https://dx.doi.org/10.1371/journal.pone.0268291.
- Долгушина В.Ф., Курносенко И.В., Алиханова Е.С., Семёнов Ю.А. Цервико-вагинальные инфекции при истмико-цервикальной недостаточности. Доктор.Ру. 2021; 20(1): 61-7. [Dolgushina V.F., Kurnosenko I.V., Alikhanova E.S., Semenov Yu.A. Cervical and vaginal infections in insuficiencia istmicocervical. Doctor.Ru. 2021; 20(1): 61-7. (in Russian)]. https://dx.doi.org/10.31550/1727-2378-2021-20-1-61-67.
- Агруц К.Р., Пасман Н.М., Степанова А.А., Каткова Н.С., Дударева А.В., Кустов С.М., Проничева С.В., Воронова Н.В. Оценка эффективности современных методов коррекции истмико-цервикальной недостаточности. Научное обозрение. Медицинские науки. 2020; 2: 16-20. [Agruts K.R., Pasman N.M., Stepanova A.A., Katkova N.S., Dudareva A.V., Kustov S.M., Pronicheva S.V., Voronova N.V. Evaluation of the effectiveness of modern correction methods cervical insufficiency. Scientific review. Medical Sciences. 2020; (2): 16-20. (in Russian)]. https://dx.doi.org/10.17513/srms.1091.
- Dan K., Lee J.E., Han D., Kim S.M., Hong S., Kim H.J., Park K.H. Proteomic identification of biomarkers in maternal plasma that predict the outcome of rescue cerclage for cervical insufficiency. PLoS One. 2021; 16(4): e0250031. https://dx.doi.org/10.1371/journal.pone.0250031.
- Hong S., Park K.H., Lee Y.E., Shin S., Kim H.J., Kim Y.M. Antibody microarray analysis of the amniotic fluid proteome for predicting the outcome of rescue cerclage in patients with cervical insufficiency. Biosci. Rep. 2021; 41(7): BSR20210174. https://dx.doi.org/10.1042/BSR20210174.
- Kacerovsky M., Musilova I., Jacobsson B., Drahosova M., Hornychova H., Janku P. et al. Cervical fluid IL-6 and IL-8 levels in pregnancies complicated by preterm prelabor rupture of membranes. J. Matern. Fetal Neonatal Med. 2015; 28(2): 134-40. https://dx.doi.org/10.3109/14767058.2014.908179.
- Sakai M., Sasaki Y., Yoneda S., Kasahara T., Arai T., Okada M. et al. Elevated interleukin-8 in cervical mucus as an indicator for treatment to prevent premature birth and preterm, pre-labor rupture of membranes: a prospective study. Am. J. Reprod. Immunol. 2004; 51(3): 220-5. https://dx.doi.org/10.1111/j.1600-0897.2004.00145.x.
Received 22.06.2023
Accepted 14.09.2023
About the Authors
Svetlana V. Pesegova, Teaching Assistant, Department of Obstetrics, Gynecology and Perinatology of the Institute of Clinical Medicine, I.M. Sechenov First MoscowState Medical University, Ministry of Health of Russia (Sechenov University), +7(499)782-30-45, pesegova_s_v@staff.sechenov.ru, https://orcid.org/0000-0002-1339-5422,
119991, Russia, Moscow, B. Pirogovskaya str., 2-4.
Elena V. Timokhina, Dr. Med. Sci., Professor, Department of Obstetrics, Gynecology and Perinatology of the Institute of Clinical Medicine, I.M. Sechenov First Moscow State Medical University, Ministry of Health of Russia (Sechenov University), +7(499)782-30-45, +7(916)607-45-34, elena.timokhina@mail.ru, https://orcid.org/0000-0001-6628-0023, 119991, Russia, Moscow, B. Pirogovskaya str., 2-4.
Alexander N. Strizhakov, Academician of the RAS, Professor, Honored Head of the Department of Obstetrics, Gynecology and Perinatology of the Institute of Clinical Medicine, I.M. Sechenov First Moscow State Medical University, Ministry of Health of Russia (Sechenov University), +7(499)782-30-45, kafedra-agp@mail.ru,
119991, Russia, Moscow, B. Pirogovskaya str., 2-4.
Irina V. Ignatko, Dr. Med. Sci., Corresponding Member of the RAS, Professor of the RAS, Professor, Head of the Department of Obstetrics, Gynecology and Perinatology of the Institute of Clinical Medicine, I.M. Sechenov First Moscow State Medical University, Ministry of Health of Russia (Sechenov University), +7(499)782-30-45,
ignatko_i_v@staff.sechenov.ru, 119991, Russia, Moscow, B. Pirogovskaya str., 2-4.
Vera S. Belousova, Dr. Med. Sci., Professor, Department of Obstetrics, Gynecology and Perinatology of the Institute of Clinical Medicine, I.M. Sechenov First Moscow State Medical University, Ministry of Health of Russia (Sechenov University), +7(499)782-30-45, belousova_v_s@staff.sechenov.ru, https://orcid.org/0000-0001-8332-7073,
119991, Russia, Moscow, B. Pirogovskaya str., 2-4.
Valeria M. Anokhina, student, I.M. Sechenov First Moscow State Medical University, Ministry of Health of Russia (Sechenov University), +7(499)782-30-45,
119991, Russia, Moscow, B. Pirogovskaya str., 2-4.
Corresponding author: Elena V. Timokhina, elena.timokhina@mail.ru