Pregnancy loss after intrauterine surgical treatment of twin-to-twin transfusion syndrome
Gladkova K.A., Sakalo V.А.
Background: The most common indication for intrauterine surgery is the fetoscopic laser coagulation (FLC) of placental anastomoses in twin-twin transfusion syndrome (TTTS). TTTS is a complication of monochorionic multiple pregnancy characterized by high perinatal and neonatal morbidity and mortality caused in most cases by preterm birth. FLC has been shown to be more beneficial than amnioreduction and is therefore the current standard of care for the treatment of TTTS. Fetoscopic coagulation is characterized by a postoperative survival rate of both fetuses of almost 90% and is associated with a high incidence of premature rupture of membranes and subsequent termination of pregnancy.
Objective: To analyze the association of preoperative cervical length shortening and its correction with termination of pregnancy in women with monochorionic twins after intrauterine TTTS surgical treatment.
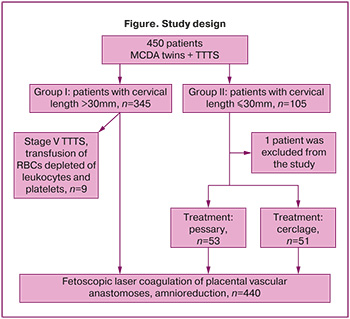
Materials and methods: This was a retrospective cohort study with the analysis of postoperative termination of pregnancy and preterm labor in patients with monochorionic twins complicated by TTTS. The study included 450 pregnant women with monochorionic diamniotic twins. All of them underwent FLC for TTTS at the National Medical Research Centre for Obstetrics, Gynecology and Perinatology in Moscow from January 2013 to January 2024. Group I (n=345) consisted of patients with preoperative cervical length ≥3 cm, group II (n=104) included patients with cervical length <3 cm, one patient was excluded from the study. Depending on the methods of cervical shortening correction, group II was divided into subgroups: subgroup 1 (n=53) had pessary, subgroup 2 (n=51) had cervical cerclage. FLC was performed in 440 cases, namely, in patients with I-IV stages of TTTS. Nine pregnant women received intrauterine treatment of TTTS stage V as transabdominal cordocentesis, intrauterine transfusion of erythrocyte mass to the surviving fetus with severe anemia.
Results: No statistically significant increase in the frequency of pregnancy loss was found in patients with correction of cervical shortening. Spontaneous pregnancy loss within seven days after surgery occurred in 17 (4.9%) patients of group I and in 6 (5.8%) patients of group II. The median term of delivery was 31.8 and 32 weeks in the study groups (p=0.281 and p=0.330, respectively). In the group of patients with cervical shortening, premature rupture of membranes was statistically significantly more frequent (p<0.05), regardless of the correction method.
Conclusion: No correlation between cervical length shortening, methods of correction and adverse pregnancy outcomes was found in our study.
Authors’ contributions: Gladkova K.A. – developing the concept and design of the study, review of publications, structural organization, writing the text; Sakalo V.A. – collection of material, analysis and statistical processing of the data, writing the text.
Conflicts of interest: The authors declare that there are no conflicts of interest.
Funding: The study was carried out without sponsorship.
Ethical Approval: The study was approved by the Ethical Review Board of the Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia.
Patient Consent for Publication: The patients signed informed consent for the publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available on request from the corresponding author after approval from the principal investigator.
For citation: Gladkova K.A., Sakalo V.А. Pregnancy loss after
intrauterine surgical treatment of twin-to-twin transfusion syndrome.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2024; (12): 26-32 (in Russian)
https://dx.doi.org/10.18565/aig.2024.245
Keywords
The development and introduction of minimally invasive fetal surgery into clinical practice is an area of active research at the present time. The most common indication for fetoscopic surgery is laser photocoagulation of placental vascular anastomoses in twin-twin transfusion syndrome (TTTS). TTTS occurs in 10–15% of monochorionic twin pregnancies and it is a major cause of perinatal morbidity and mortality [1, 2]. Fetoscopic laser coagulation (FLC) of placental vascular anastomoses is the only effective treatment for stage II-IV TTTS [3, 4], which has significantly reduced perinatal mortality and shifted the vector from child morbidity to the consequences of premature rupture of membranes (PROM) and preterm labor (PTL), including such serious long-term complications as cerebral palsy, delayed motor and cognitive development [5–7]. The mean gestational age at delivery in patients with TTTS is 29–33 weeks, and the incidence of PROM is as high as 39% [8–10]. Reducing the rate of PTL is a key to improving the management of pregnant women and perinatal outcomes in patients with TTTS.
Preoperative assessment of risk factors for perinatal failure plays an important role in developing a management strategy for complicated monochorionic pregnancy. Preoperative cervical shortening occurs in approximately 10% of patients with TTTS and it is considered to be a significant risk factor for PTL [9]. Specifically, cervical length of less than 30 mm is associated with a higher incidence of spontaneous PTL, as well as an increased neonatal mortality [11]. Buskmiller C. et al. (2022) showed that cervical shortening and absence of treatment led to the following results: more than one in four (26%) pregnant women gave birth within 4 weeks after FLC, about one third of women (30%) had PROM, and almost two thirds (62%) gave birth before 32 weeks [12].
Cervical shortening is an evident risk factor for early termination of pregnancy, yet the optimal intervention to reduce PTL in this cohort of patients remains unclear [12–14]. In most studies, expectant management, progesterone, cerclage, and pessary placement have not been shown to be effective in preventing PTL in multiple pregnancies [15]. A retrospective study conducted by Bartin R. et al. (2024) showed that the use of Arabin pessary in pregnant women with cervical length of 5–18 mm with TTTS contributed to later delivery and improved perinatal survival [16]. However, the routine use of a pessary was not shown to be effective and a large randomized trial was terminated prematurely [17]. In small studies of patients with TTTS and short cervical length (1–1.5cm), preoperative cervical cerclage was found to be associated with longer duration of pregnancy [18], while large prospective cohort studies did not prove the efficacy of cerclage [12, 19].
A better understanding of the causes of pregnancy termination and preterm labor in this patient population may be the first step in optimizing the management strategy after intrauterine treatment of TTTS.
The aim of the study is to analyze the association of preoperative cervical shortening and its treatment with termination of pregnancy in women with monochorionic twins after intrauterine surgical treatment of TTTS.
Materials and methods
This was a retrospective cohort study conducted at the Academician V.I. Kulakov National Medical Research Centre for Obstetrics, Gynecology and Perinatology (Centre) in Moscow from January 2013 to January 2024. The study included 450 women with monochorionic diamniotic twin pregnancies complicated by TTTS, most of them underwent FLC of placental vascular anastomoses. Group I (n=345) consisted of patients with preoperative cervical length ≥3 cm and group II (n=105) included patients with cervical length <3 cm. Depending on the methods of treatment of cervical shortening, group II was divided into subgroups: subgroup 1 (n=53) had a pessary placement, subgroup 2 (n=51) underwent cervical cerclage (Figure). One patient with cervical shortening was excluded after refusing to undergo treatment. Patients with stages I–IV TTTS underwent laser coagulation of placental vascular anastomoses. Surgical treatment of stage I TTTS was performed only in the presence of echographic evidence of cardiomyopathy in the recipient fetus (cardiomegaly, myocardial hypertrophy). Nine patients with stage V TTTs underwent transabdominal cordocentesis and intrauterine transfusion of erythrocyte mass washed of leukocytes and platelets to the fetus that survived and had severe anemia.
The inclusion criteria for this study are as follows: monochorionic diamniotic twins complicated by stage I–V TTTS according to the classification system developed by R. Quintero with the subsequent intrauterine treatment and postoperative treatment at the Centre.
There were the following non-inclusion criteria: monochorionic monoamniotic twins, higher order multifetal pregnancies (triplets, quadruplets), refusal of treatment.
Gestational age was determined by measuring the crown rump length of the larger fetus at 11–14 weeks’ ultrasound scanning in case of spontaneous pregnancy or by the date of embryo transfer, taking into account the days of culturing, in case of pregnancy resulting from in vitro fertilization. Chorionicity was confirmed by ultrasound scanning at 14–15 weeks’ gestation. TTTS was diagnosed based on the following echographic criteria: donor twin anemia (maximum vertical pocket (MVP) less than 2 cm) and recipient twin anemia (MVP more than 8–10 cm). TTTS severity was assessed according to the classification proposed by Quintero R. et al. (1999) [20].
A complete clinical and laboratory examination, expert ultrasound assessment and Doppler ultrasonography of fetal and feto-placental blood flow, and transvaginal cervicometry were performed before surgery. In case of cervical shortening <3 cm, two methods of correction were performed before FLC: Arabin pessary (Dr. Arabin GmbH & Co. KG, Witten, Germany); surgical cerclage with two circular or U-shaped 2-Ethibond excel sutures (Ethicon Inc.) or one circular suture using Mersilene tape (Ethicon Inc., Somerville, NJ, USA). The patients who were prescribed vaginal progesterone received micronized progesterone vaginally 200-400 mg daily until labor. Due to the fact that most of the patients received progesterone irrespective of cervical length and long before coming to the Centre, the efficacy of progesterone was not evaluated in our study.
FLC technique included local anesthesia, transabdominal access under ultrasound guidance into the amniotic cavity of the recipient twin. In order to ensure an optimal view of the anastomoses, a trocar with a diameter of 3.3 mm was inserted opposite the presumed vascular equator of the placenta. A curved fetoscope was used to provide optimal visibility of the anterior placenta.
In a number of clinical cases, there was a partial replacement of amniotic fluid due to unsatisfactory visualization caused by staining of amniotic fluid. Partial replacement of amniotic fluid was performed using amnioreduction and amnioinfusion of physiological solution heated to 37–38.0°C until optimal visualization was achieved.
Non-contact laser photocoagulation was performed with the help of yttrium-neodymium laser (Dornier MedTech, Germany), laser energy power did not exceed 40W. The operation was completed by amnioreduction until there was a normal amount of amniotic fluid in the recipient twin.
At the beginning of the operation and in the early postoperative period all patients received tocolytic therapy: nifedipine or indomethacin, antibiotic therapy, namely second- and third-generation cephalosporins for 3–5 days. After the operation, the condition of the pregnant woman and fetus were monitored; the results of the laboratory tests and ultrasound were examined for 5–7 days during the in-patient treatment. After discharge from hospital, the patients underwent ultrasound assessment weekly or every two weeks and were managed either at the Centre or at their local clinics under the supervision of the specialists of the Centre during telemedicine consultations. The course of pregnancy was further assessed on the basis of fetal monitoring that included the data on intrauterine death of one or both fetuses, postoperative complications, and the time of delivery.
The primary outcome was the assessment of termination of pregnancy in the early postoperative period (within 7 days). The secondary outcomes included the delivery before 34 weeks of gestation, PROM before 34 weeks of gestation.
Statistical analysis
The statistical processing of the results of the study was carried out using the SPSS 26.0 software package. Descriptive statistics for qualitative characteristics are presented as absolute values (n, %) and as median and interquartile range (Me [Q1; Q3]). The significance of differences in quantitative characteristics between groups was compared using the Mann–Whitney test, and the significance of differences in qualitative characteristics was compared using the chi-square test (χ2). Differences were considered statistically significant at the level of p<0.05.
The study was approved by the Ethical Review Board of the Academician V.I. Kulakov National Medical Research Center for Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia.
Results
Cervical shortening was diagnosed in 105/450 (23.3%) patients with monochorionic diamniotic twin pregnancies complicated by TTTS. One patient was excluded from the study, thus there were 104 patients left for further analysis: 53 of them were treated with a pessary and 51 pregnant women were treated with a cerclage (Figure). A total of 440 patients underwent fetoscopic laser coagulation of placental vascular anastomoses. Cordocentesis was performed in 9 cases: these pregnant women had stage V TTTS and their fetuses that survived experienced severe anemia, therefore fetuses had the transfusion of red blood cells depleted of leukocytes and platelets.
According to the ultrasound cervicometry findings obtained on admission, cervical length in patients of group II was significantly different from those in group I (median: 24 mm vs. 37 mm; p<0.001). No differences were found between groups in age, BMI, achieving pregnancy, parity, and TTTS stage. The details of the preoperative characteristics are presented in Table 1.
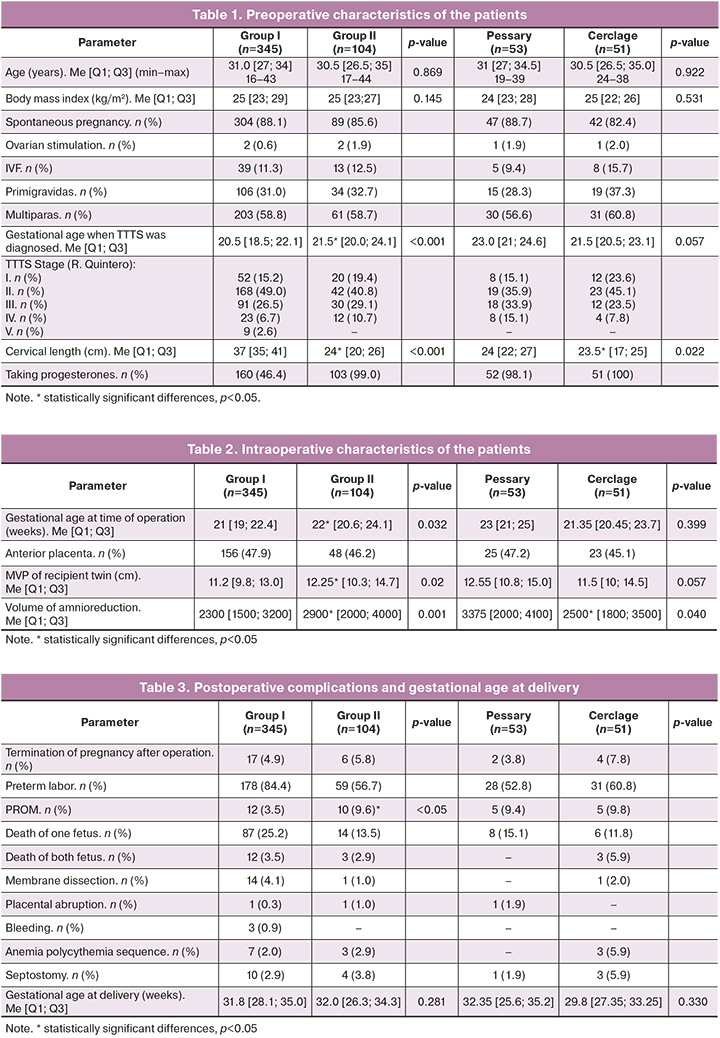
The mean gestational age at the time of intrauterine treatment was 21 weeks in group I and 22 weeks in group II (p=0.032). When assessing the intraoperative characteristics of the patients in both groups (Table 2), one should pay attention to the difference in the amount of amniotic fluid, severity of polyhydramnios in the recipient twin and therefore the volume of amnioreduction (p=0.02 and p=0.001). Perhaps cervical shortening in patients of group II was caused by severe polyhydramnios.
The data presented in Table 3 show that there are no associations between preoperative cervical length with subsequent correction by different methods and postoperative termination of pregnancy as well as the time of delivery. Spontaneous termination of pregnancy within 7 days after operation occurred in 17/345 (4.9%) patients in group I and 6/104 (5.8%) in group II. The median of gestational age at delivery was 31.8 and 32 weeks in the study groups, respectively (p=0.281 and p=0.330). In the group of patients with cervical shortening, PROM was statistically significantly more frequent (p<0.05) regardless of the correction method. The details of postoperative complications are shown in Table 3.
Discussion
Termination of pregnancy and PTL remain a major challenge in the management of patients with monochorionic twin pregnancy complicated by TTTS. Spontaneous PTL before 32 weeks gestation remains a main problem in TTTS in more than 40% of patients [9]. Many factors are believed to contribute to the pathogenesis of termination of pregnancy, including the invasiveness of intrauterine surgery, overstretched uterine wall and cervical incompetence. Another multifactorial cause is the large-scale introduction of the Solomon technique, which significantly improved fetal survival, but it also increased the incidence of PROM and PTL, which can be a serious disadvantage, especially when the operation is performed at early gestation [21].
Given the contradictory results in the literature on the effectiveness of pessary placement and cervical suturing in preventing PTL in multifetal pregnancies, the use of these findings for patients with TTTS whose pregnancies were complicated by severe polyhydramnios and intrauterine surgery is controversial. In TTTS, the association between the severity of polyhydramnios, intra-amniotic pressure, cervical shortening and perinatal outcome remains unclear [22]. Investigating this issue, Finneran M. et al. (2016) did not obtain any data on the change in cervical length after amnioreduction, which, in turn, contradicts the idea of a purely mechanical effect of polyhydramnios [23]. Further, a large 2018 cohort study showed no correlation between cervical shortening before FLC and PROM [24]. It should be noted that amniotic fluid leakage after FLC is not correctly assessed as a standard obstetric complication, as in some cases it starts from the site of instrument insertion into the uterus and stops after some time.
Although cervical shortening before surgery appears to be the only visible preoperative ‘part of the iceberg’ of risk factors for spontaneous PTL and termination of pregnancy in TTTS, our study did not identify an association between cervical length and correction methods and adverse pregnancy outcomes either. In our study, postoperative pregnancy loss occurred in the group of patients with normal length cervix with the same frequency as in the group with cervix shortening followed by correction.
Our findings are consistent with a recent retrospective study conducted by Buskmiller C. et al. (2022), who similarly compared interventions for cervical shortening to prevent PTL with expectant management in patients with monochorionic diamniotic twin pregnancy with TTTS [12]. The authors found no evidence for the efficacy of any management method, particularly a pessary, unlike Bartin R. et al. (2023) who showed that pessaries were effective at cervical length of 5–18 mm [16].
Conclusion
Current understanding of the pathogenesis of termination of pregnancy and PTL after FLC is variable; suggested risk factors and current management tactics are controversial and not supported by conclusive evidence. The analysis of postoperative management strategies for patients with complicated monochorionic multiple pregnancies should be evaluated in randomized trials, which can improve overall perinatal outcomes, reduce neonatal mortality and morbidity and be the next step in making fetoscopic laser surgery for TTTS more effective.
References
- Lewi L. Monochorionic diamniotic twin pregnancies. Am. J. Obstet. Gynecol. MFM. 2022; 4(2): 100501. https://dx.doi.org/10.1016/j.ajogmf.2021.100501.
- Djaafri F., Stirnemann J., Mediouni I., Colmant C., Ville Y. Twin–twin transfusion syndrome – What we have learned from clinical trials. Semin. Fetal. Neonatal. Med. 2017; 22(6): 367-75. https://dx.doi.org/10.1016/j.siny.2017.08.005.
- Slaghekke F., Lopriore E., Lewi L., Middeldorp J.M., van Zwet E.W., Weingertner A.S. et al. Fetoscopic laser coagulation of the vascular equator versus selective coagulation for twin-to-twin transfusion syndrome: an open-label randomised controlled trial. Lancet. 2014; 383(9935): 2144-51. https://dx.doi.org/10.1016/S0140-6736(13)62419-8.
- Костюков К.В., Сакало В.А., Гладкова К.А., Шакая М.Н., Ионов О.В., Тетруашвили Н.К. Перинатальные исходы монохориальной многоплодной беременности, осложненной фето-фетальным трансфузионным синдромом. Акушерство и гинекология. 2020; 8: 72-80. [Kostyukov K.V., Sakalo V.A., Gladkova K.A., Shakaya M.N., Ionov O.V., Tetruashvili N.K. Perinatal outcomes of monochorionic multiple pregnancies complicated by twin-to-twin transfusion syndrome. Obstetrics and Gynecology. 2020; (8): 72-80 (in Russian)]. https://dx.doi.org/10.18565/aig.2020.8.72-80.
- Snowise S., Mann L.K., Moise K.J., Johnson A., Bebbington M.W., Papanna R. Preterm prelabor rupture of membranes after fetoscopic laser surgery for twin–twin transfusion syndrome. Ultrasound Obstet. Gynecol. 2017; 49(5): 607-11. https://dx.doi.org/10.1002/uog.15958.
- Rossi A.C., Vanderbilt D., Chmait R.H. Neurodevelopmental outcomes after laser therapy for twin–twin transfusion syndrome. Obstet. Gynecol. 2011; 118(5): 1145-50. https://dx.doi.org/10.1097/AOG.0b013e318231827f.
- Stirnemann J., Djaafri F., Kim A., Mediouni I., Bussieres L., Spaggiari E. et al. Preterm premature rupture of membranes is a collateral effect of improvement in perinatal outcomes following fetoscopic coagulation of chorionic vessels for twin–twin transfusion syndrome: a retrospective observational study of 1092 cases. BJOG. 2018; 125(9): 1154-62. https://dx.doi.org/10.1111/1471-0528.15147.
- Robyr R., Boulvain M., Lewi L., Huber A., Hecher K., Deprest J. et al. Cervical length as a prognostic factor for preterm delivery in twin‐to‐twin transfusion syndrome treated by fetoscopic laser coagulation of chorionic plate anastomoses. Ultrasound Obstet. Gynecol. 2005; 25(1): 37-41. https://dx.doi.org/10.1002/uog.1798.
- Papanna R., Mann L.K., Baschat A.A., Bebbington M.W., Khalek N., Johnson A. et al. Cervical length in prediction of preterm birth after laser surgery for twin-twin transfusion syndrome. Ultrasound Obstet. Gynecol. 2015; 45(2): 175-82. https://dx.doi.org/10.1002/uog.14696.
- Malshe A., Snowise S., Mann L.K., Boring N., Johnson A., Bebbington M.W.et al. Preterm delivery after fetoscopic laser surgery for twin–twin transfusion syndrome: etiology and risk factors. Ultrasound Obstet. Gynecol. 2017;49(5): 612-6. https://dx.doi.org/10.1002/uog.15972.
- Buskmiller C., Bergh E.P., Brock C., Miller J., Baschat A., Galan H. et al. Interventions to prevent preterm delivery in women with short cervix before fetoscopic laser surgery for twin-twin transfusion syndrome. Ultrasound Obstet. Gynecol. 2022; 59(2): 169-76. https://dx.doi.org/10.1002/uog.23708.
- Доброхотова Ю.Э., Кузнецов П.А., Джохадзе Л.С., Константинова К.И. Коррекция истмико-цервикальной недостаточности при многоплодной беременности. Дискуссионные вопросы. Акушерство и гинекология. 2017; 11: 10-5. [Dobrokhotova Yu.E., Kuznetsov P.A., Dzhokhadze L.S., Konstantinova K.I. Correction of isthmic-cervical insufficiency in multiple pregnancies: Debating points. Obstetrics and Gynecology. 2017; (11): 10-5.(in Russian)]. https://dx.doi.org/10.18565/aig.2017.11.10-15.
- Roman A., Ramirez A., Fox N.S. Prevention of preterm birth in twin pregnancies. Am. J. Obstet. Gynecol. MFM. 2022; 4(2): 100551. https://dx.doi.org/10.1016/j.ajogmf.2021.100551.
- Bartin R., Andrioli Peralta C.F., Peneluppi Horak A.C., Rodrigues daCosta K.J., Colmant C., Stirnemann J. et al. Management of short cervix in twin-to-twin transfusion syndrome: a role for pessary placement following fetoscopic laser surgery? Am. J. Obstet. Gynecol. 2024; 230(1): 91.e1-91.e12. https://dx.doi.org/10.1016/j.ajog.2023.07.014.
- Rodo C., Maiz N., Arevalo S., Lewi L., Couck I., Hollwitz B. et al. The Arabin cervical pessary for the prevention of preterm birth in twin-to-twin transfusion syndrome treated by fetoscopic laser coagulation: a multicenter randomized controlled trial. Am. J. Obstet. Gynecol. 2024; 231(2): 252.e1-252.e11. https://dx.doi.org/10.1016/j.ajog.2023.11.1245.
- Salomon L.J., Nasr B., Nizard J., Bernard J.P., Essaoui M., Bussieres L. et al. Emergency cerclage in cases of twin-to-twin transfusion syndrome with a short cervix at the time of surgery and relationship to perinatal outcome. Prenat. Diagn. 2008; 28(13): 1256-61. https://dx.doi.org/10.1002/pd.2156.
- Chmait R.H., Korst L.M., Llanes A., Mullin P., Lee R.H., Ouzounian J.G. Perioperative characteristics associated with preterm birth in twin-twin transfusion syndrome treated by laser surgery. Am. J. Obstet. Gynecol. 2013; 209(3): 264.e1-8. https://dx.doi.org/10.1016/j.ajog.2013.05.025.
- Quintero R.A., Morales W.J., Allen M.H., Bornick P.W., Johnson P.K., Kruger M. Staging of twin-twin transfusion syndrome. J. Perinatol. 1999; 19(8): 550-5. https://dx.doi.org/10.1038/sj.jp.7200292.
- D’Antonio F., Herrera M, Oronzii L, Khalil A. Solomon technique vs selective fetoscopic laser photocoagulation for twin–twin transfusion syndrome: systematic review and meta‐analysis of maternal and perinatal outcomes. Ultrasound Obstet Gynecol. 2022; 60(6): 731-8. https://dx.doi.org/10.1002/uog.26095.
- Bergh E.P., Mann L.K., Jain R.R., Donepudi R., Moise K.J., Johnson A. et al. Effect of intra‐amniotic fluid pressure from polyhydramnios on cervical length in patients with twin–twin transfusion syndrome undergoing fetoscopic laser surgery. Ultrasound Obstet. Gynecol. 2019; 54(6): 774-9. https://dx.doi.org/10.1002/uog.20228.
- Finneran M., Temming L., Templin M., Stephenson C. Effect of cervical length recovery after laser surgery for twin-twin transfusion syndrome. AJP Rep. 2016; 6(1): e137-41. https://dx.doi.org/10.1055/s-0036-1579654.
Received 07.10.2024
Accepted 25.11.2024
About the Authors
Kristina A. Gladkova, PhD, Senior Researcher at the Fetal Medicine Unit, Institute of Obstetrics, Head of the 1st Obstetric Department of Pregnancy Pathology, V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia, 117997, Russia Moscow, Ac. Oparin str., 4, +7(916)321-10-07, k_gladkova@oparina4.ru,https://orcid.org/0000-0001-8131-4682
Viktoriya A. Sakalo, PhD, Researcher of the Fetal Medicine Unit, Institute of Obstetrics, obstetrician-gynecologist at the 1st Obstetric Department of Pregnancy Pathology, V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia, 117997, Russia Moscow, Ac. Oparin str., 4, +7(929)588-72-08, v_sakalo@oparina4.ru,
https://orcid.org/0000-0002-5870-4655