Тяжелая преэклампсия (ПЭ) – осложнение беременности с высоким риском угрозы жизни, состояния near miss, сохраняет лидирующие позиции по причинам материнской смертности (МС) во всем мире, включая развитые станы [1, 2]. В Российской Федерации показатель МС в 2018 г. составил 9,1 на 100 000 родившихся живыми (абсолютное число случаев – 146), по причине ПЭ – 0,81 (8,9% от всех причин МС) [3]. ПЭ относится к гипертензивным расстройствам во время беременности, в родах и послеродовом периоде, но в ее дефинициях [4–7], в международной классификации болезней 11 пересмотра в том числе (код JA24) [8], помимо артериальной гипертензии (АГ) при наличии протеинурии, указываются другие, не менее значимые маркеры – вновь возникшая материнская органная дисфункция (только тромбоцитопения, или повышенный в сыворотке крови уровень креатинина или печеночных трансаминаз, или неврологическое состояние, или задержка роста плода (ЗРП). Не исключается атипическое течение ПЭ – без АГ, с дебютом ранее 20 недель, с отсутствием протеинурии и др. [7]. Рост частоты раннего дебюта ПЭ (до 34 недель беременности) обосновал дифференцировку ПЭ «раннюю» (Early-onset) и преждевременную (Preterm) (FIGO, The International Federation of Gynecology and Obstetrics, англ. – Международная федерация акушеров-гинекологов, 2019), регламентирующую скрининг и профилактику ПЭ, начиная с I триместра беременности [6]. Ранняя манифестация и атипичная клиническая картина ПЭ признаны одной из ключевых причин ее несвоевременной диагностики и риска прогрессирования в тяжелые формы, непредотвратимой МС [9–12]. Возможность высокоточного прогноза ПЭ, обосновывающего ее эффективную профилактику, является поводом для острой полемики во всем мире [13–16].
Целью настоящего исследования явилось изучение клинико-лабораторных критериев «точки отсчета» транзита тяжелой ПЭ в угрожающее жизни состояние с различным исходом (near miss или МС).
Материалы и методы
Проведено ретроспективное многоцентровое исследование, основанное на экспертизе 18 130 историй родов, осложненных тяжелой ПЭ. Период исследования – 1 января 2013–31 декабря 2018 гг. Количество центров – 27 учреждений здравоохранения г. Москвы. Из общего числа отобраны 122 истории родов женщин с ПЭ и угрожающим жизни состояниями, приведшими к развитию у 100 пациенток состояния near miss (группа Near miss), у 22 – МС (группа МС). Отбор пациенток с near miss основывался на применении таблицы случайных чисел, сгенерированной при помощи пакета анализа данных программы Excel 2007. В группу МС включали всех пациенток с данным исходом в указанный период. Критерии near miss соответствовали рекомендациям ВОЗ [2].
Статистический анализ данных выполняли при помощи программ Statistica 12.0, Microsoft Excel 2007. Оценивались: n – число женщин; М – среднее значение, Me – медиана; SD – стандартное отклонение; верхний и нижний квартили (Q25 и Q75); минимальное (Min) и максимальное (Max) значения. Значимость различий (p) оценивали при нормальности распределения вариаций и однородности дисперсий по t-критерию Стьюдента, при ненормальности распределения – U-критерию Манна–Уитни; нормальность распределения - по критерию Колмогорова–Смирнова, при р>0,05 распределение расценивалось нормальным. Для сравнения двух зависимых (парных) выборок при нормальности распределения использовали парный t-критерий Стьюдента, при ненормальности – одновыборочный критерий Уилкоксона. Для оценки значимости различий исходов в зависимости от воздействия фактора рассчитывался критерий хи-квадрат (χ2), при n<10 – χ2 с поправкой Йейтса. Количественную интерпретацию тесноты связи фактора риска с исходом основывали на расчете отношения шанса (ОШ) с 95% доверительным интервалом (ДИ). Для прогнозирования бинарного исхода (переменные отклика – near miss (0) и МС (1) с учетом изучаемого параметра (предиктора) применяли метод бинарной логистической регрессии (logit–модель), рассчитывая значения логистической функции (от 0 до 1); коэффициент регрессии В, стандартную ошибку, статистику Вальда, проверяющую значимость отличия коэффициентов от нуля, 95% ДИ. Значимость модели оценивали по значению уровня построенной модели (р) менее 0,05. Экспоненты коэффициентов логистической регрессии с 95% ДИ рассматриваются как ОШ для оценки вероятности наступления бинарного исхода согласно определенному предиктору. Разбиение множества исследуемых признаков на группы однородности проводили на основании метода кластерного анализа с предварительной стандартизацией данных. Для объективной оценки различий групп использовали дискриминантный анализ; значимость дискриминации (различий) определяло значение лямбды Уилкса (чем ближе к 0, тем дискриминация лучше), значимость которого подтверждалась F-критерием и p<0,05; квадрат расстояния Махаланобиса и его статистическую значимость (p). Рассчитывали значения переменных для уравнения дискриминантной функции (коэффициенты переменных и константу), позволяющие подсчитать баллы классификации дискриминантной функции, наибольший из которых определял вероятный исход (near miss или МС), точность прогноза в обучающей выборке.
Результаты и обсуждение
Возраст пациенток был крайне вариабелен (от 17 до 45 лет), не соотносился с известными рисками тяжелой ПЭ [4, 7], в группах Near miss (32,01 (6,29) года) и МС (29,82 (6,33) года) был сопоставим (р=0,14). Соответствуя глобальному росту частоты ПЭ с ранним дебютом, срок беременности составил 32,64 (4,23) (24-40) недель в группе МС и 34,33 (3,91) (22-41) недель в группе Near miss (p=0,07). Несмотря на то, что ранняя ПЭ определяет риск тяжелого ее течения [2, 4, 5, 7], МС не была сопряжена с ранним дебютом ПЭ: доля пациенток группы Near miss и МС была сопоставима (41 и 50% соответственно, χ2=0,6, р=0,44; ОШ=1,22, 95% ДИ 0,57–3,63).
Трудность своевременной диагностики ПЭ, включая тяжелую [1, 12, 13, 16–18], объяснялась отсутствием «классических» симптомов ПЭ или ее атипичным течением. Бригадой скорой медицинской помощи (СМП) были доставлены 81,82% женщин группы МС и 94% Near miss (p=0,15), но в плановом порядке поступили 9,09 и 4% (p=0,65), и 2 женщин каждой группы обратились в приемный покой ПЦ самостоятельно (p=0,3). В унисон с исследователями, доказывающим вероятность начального бессимптомного течения тяжелой ПЭ [9, 12], отмечено, что у 16,39% от общего числа женщин (22,73% в группе МС и 15% Near miss, p=0,57) при поступлении в ПЦ отсутствовали жалобы, характерные для ПЭ, и отражали только «акушерские» аспекты: начало регулярной родовой деятельности, отхождение околоплодных вод и прочее, и в направляющей медицинской документации СМП, и в истории родов при поступлении в ПЦ отсутствовали сведения о ПЭ. Степень тяжести общего состояния при поступлении в ПЦ была расценка как удовлетворительная.
Симптомы, патогномоничные для тяжелой ПЭ, отмечались в группе МС и Near miss с сопоставимой частотой: ухудшение самочувствия, общая слабость (соответственно 68,18 и 72%, р=0,72), головная боль, выраженная тяжесть в затылке (40,918 и 21% соответственно, р=0,09), боли в эпигастрии (18,18% и 8% соответственно, р=0,29); рвота – только в группе МС (13,64%, р=0,003). Дифференцирующим отличием женщин группы МС от Near miss явилось наличие судорог (27,27 и 1% соответственно, р<0,001). Тяжелое общее состояние явилось значимым фактором риска МС, диагностировано значительно чаще, чем в группе Near miss (36,36 и 15% соответственно, p=0,04; ОШ=3,24; 95% ДИ 1,16–9,05).
Критерии Near miss по ВОЗ [2] при поступлении в ПЦ отмечались менее чем у 10% пациенток исследуемой когорты: в группе МС - кома у 9,09%, выраженный ацидоз крови (pH<7,1) – у 9,09%, уровень билирубина более 100 мкмоль/л – у 4,55%, креатинина 300 мкмоль/л и более – у 4,55%, лактата – более 5 ммоль/л у 4,55%, количество тромбоцитов менее 50 тыс./мл у 4,55%, сатурация кислорода менее 90% – у 4,55%; в группе Near miss - кома у 1% женщин, сатурация кислорода менее 90% – у 4%, количество тромбоцитов менее 50 тыс./мл – у 1%. Полученные данные вызывают особую настороженность в связи с тем, что медиана временного интервала от поступления женщины в ПЦ до диагностики угрожающего жизни состояния в обеих группах составила 0 суток (до 24 ч), интерквартильный диапазон в группе МС составил 0–5 суток, в группе Near miss – 0 суток (до 24 ч). Следовательно, у основной доли женщин, первые 24 ч от поступления в ПЦ являлись точкой отсчета риска развития угрожающего жизни состояния, обусловленного ПЭ.
Трудности эффективной профилактики и своевременной диагностики ПЭ объясняют поступление женщин в ПЦ с той стадии, когда предупредить тяжелые функциональные и полиорганные нарушения невозможно, и родоразрешение уже не являлось мерой предотвращения критических, потенциально необратимых осложнений ПЭ. Согласуясь с известными рисками дебюта 44% эклампсий в послеродовом периоде [4], обнаружено, что угрожающее жизни состояние развилось после родоразрешения у 9,09% женщин в группе МС и у 6% – в группе Near miss (р=0,96), в родах – только у 1 женщины группы МС. Осложнения, обусловленные или сопряженные с ПЭ, прогресс которой в угрожающее жизни произошел до (а) или после родоразрешения (б), отражены на рис. 1.
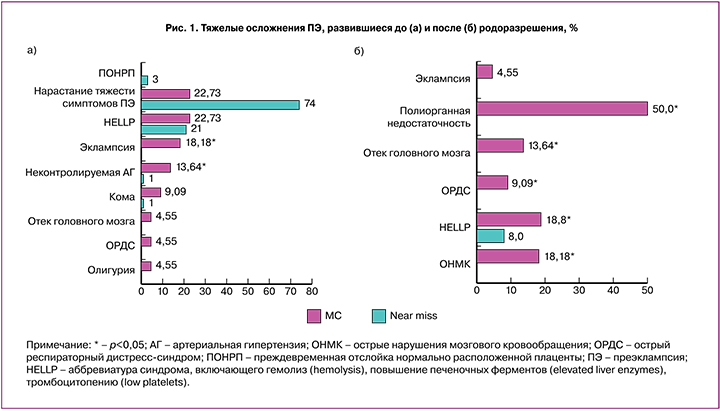
Согласно данным FIGO (2019), у женщин с ПЭ внутримозговое кровоизлияние является первостепенной причиной МС среди других (преждевременная отслойка нормально расположенной плаценты (ПОНРП), HELLP-синдром, острый отек легких, острый респираторный дистресс-синдром (ОРДС) и острая почечная недостаточность) [5]. Согласно полученным данным, угрожающие жизни состояния, развившиеся при беременности, были сопряжены с эклампсией (в группе МС частота составила 18,1,8%, в Near miss – 1%, р<0,001) и неконтролируемой значительной АГ (200/100 мм рт.ст. и выше) (13,64 и 1% соответственно, р<0,02); после родоразрешения - с эклампсией (4,55%, р=0,4), острые нарушения мозгового кровообращения (ОНМК) (18,18%, р<0,001), ОРДС (9,09%, р=0,04), отеком головного мозга (13,64%, р=0,003), и у 50% - полиорганной недостаточностью (ПОН) (р<0,001), которые диагностированы только в группе МС, и HELLP-синдромом у сопоставимого с группой Near miss количества женщин (18,18% и 8% соответственно, р=0,29). Таким образом, показано, что у женщин с ПЭ риск МС, в отличие от near miss, был значительно выше при тяжелом состоянии при поступлении в ПЦ (ОШ=3,24, 95% ДИ 1,16–9,05), неконтролируемой значительной АГ (ОШ=15,63, ДИ 1,54–158,4), судорогах (ОШ=37,13, ДИ 4,19–329,05), эклампсии (ОШ=46,2, ДИ 5,3–402,44).
Несмотря на то, что тяжелая ПЭ не является абсолютным показанием к родоразрешению путем операции кесарева сечения (КС) [4], тяжесть состояния матери или плода, отсутствие условий для преиндукции родов, ПОНРП потребовали родоразрешения основной доли женщин в группе МС и Near miss путем операции КС (86,36% и 88% соответственно, р=0,88). Вопреки тяжелому течению ПЭ, высоким рискам коагулопатии [6], кровопотеря при родоразрешении путем КС составила в среднем 616,07 (284,92) мл, была сопоставима при МС и Near miss (719,05 (473,15) мл и 592,31 (217,55) мл соответственно, р=0,07). ПОНРП произошла только у 3% женщин в группе Near miss, общая кровопотеря составила 1000 (200) (800–1200) мл. Кровотечение не явилось дифференцирующим предиктором МС и Near miss, его частота была незначительной и сопоставимой между пациентками групп МС и Near miss: интраоперационно – у 2% пациенток группы Near miss, в раннем послеродовом периоде – у 5,55% группы МС и 7% Near miss, в позднем послеродовом периоде (на 6-е и 12-е сутки) – у 9,09% пациенток группы МС.
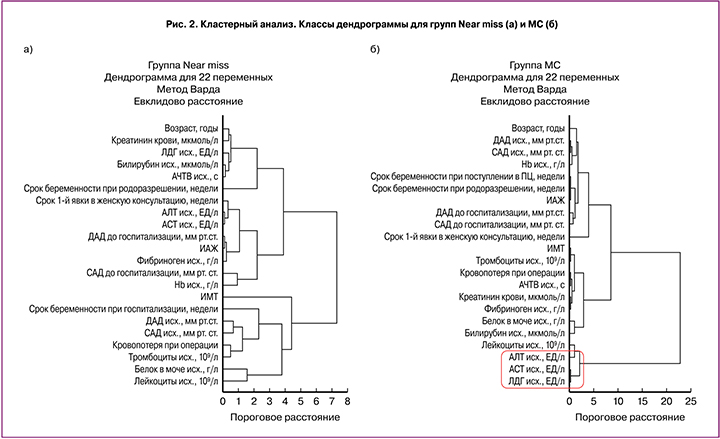
Несмотря на то, что мировое сообщество признает отсутствие точного предиктора (-ов) ПЭ, был проведен поиск вероятной точки «невозврата», когда при развитии тяжелой ПЭ риск МС превышал вероятность Near miss. При анализе различных анамнестических, клинических, лабораторных и функциональных параметров установлено, что у женщин с ПЭ дифференцировку исхода угрожающего жизни состояния определяла различная группа признаков, распределенная с помощью кластерного анализа (после предварительной стандартизации их значений) на основные классы в каждой группе, но с различным пороговым расстоянием (для группы Near miss=4,42 и для группы МС=8,48). Отмечено, что МС конкурентно с гемодинамической, ренальной, коагуляционной и др. определяла печеночная дисфункция (рис. 2).
Проблема предотвращения МС отчасти кроется в том, что в современных протоколах четко обозначены критерии тяжелой ПЭ и критерии near miss. Значительные трудности представляет определение «точки отсчета» прогресса ПЭ в угрожающее жизни состояние. Оценена динамика клинико-лабораторных маркеров ПЭ от поступления в ПЦ до развития угрожающего жизни состояния с учетом показанного интервала времени (медиана – 0 суток) менее 24 ч). Полученные данные дополнили общемировую дискуссию по вопросам интерпретации АГ как облигатного маркера ПЭ [11–13, 17, 18]. Действительно, в группе женщин с МС АД обнаружены значения 180/100 мм рт.ст., в группе Near miss – 220/110 мм рт.ст. Однако, в группе МС в сравнение с Near miss, начиная с догоспитального этапа, значения систолического АД (121,07 (26,47) мм рт.ст. и 152,03 (15,53) мм рт.ст. соответственно) и диастолического АД (77,15 (14,37) мм.рт.ст. и 93,28 (6,44) мм рт.ст. соответственно) были значимо ниже (р<0,0001). До развития угрожающего жизни состояния АД в группе МС не превышали 160/100 мм рт.ст., в группе Near miss достигали 200/120 мм рт.ст., среднее значения систолического АД составляли 115,68 (33,96) и 146,21 (17,08) мм рт.ст. соответственно (р<0,0001), диастолического – 71,96 (21,83) и 91,16 (9,24) мм рт.ст. соответственно (р<0,0001). Только в группе Near miss выявлено статистически значимое увеличение уровня систолического АД в сравнение с догоспитальными значениями (р=0,03), в группе МС аналогичная динамика отсутствовала.
Сравнительный анализ значений АД показал, что систолическое АД 140 мм рт.ст. и более выявлено только у 76% пациенток в группе Near miss и 27,27% пациенток в группе МС (χ2=17,28, р<0,001), диастолическое АД 90 мм рт.ст. и выше – у 72% пациенток в группе Near miss и 22,72% пациенток в группе МС (χ2=16,75, р<0,001). Тяжелая АГ выявлена у значительно меньшего числа женщин: систолическое АД 160 мм рт.ст. и более - у 26% пациенток в группе Near miss и 9,09% пациенток в группе МС (χ2=2,04, р=0,15), диастолическое АД 110 мм рт.ст. и выше - только у 4% пациенток в группе Near miss (χ2=0,09, р=0,77). Протеинурия 3 г/л и более была у 46% пациенток в группе Near miss и 31,82% пациенток в группе МС (χ2=0,96, р=0,33), 5 г/сутки и более – у 18% пациенток в группе Near miss и 9,09% пациенток в группе МС (χ2=0,5, р=0,48). Таким образом, тяжелая ПЭ, прогрессирующая в Near miss или МС в диапазоне времени (медиана 0 суток) от 0 до 5 суток, не исключала отсутствие АГ и/или протеинурии.
Предиктором критических полиорганных и полифункциональных нарушений, обусловленных ПЭ, явилась динамика ее лабораторных маркеров, отражающих тяжесть коагуляционной/гематологической (тромбоциты, фибриноген, АЧТВ), почечной (креатинин), печеночной (билирубин, АЛТ, АСТ, ЛДГ), кардиоваскулярной (лактат, ph), респираторной (сатурация кислорода) дисфункции, обусловленной ПЭ (табл. 1).
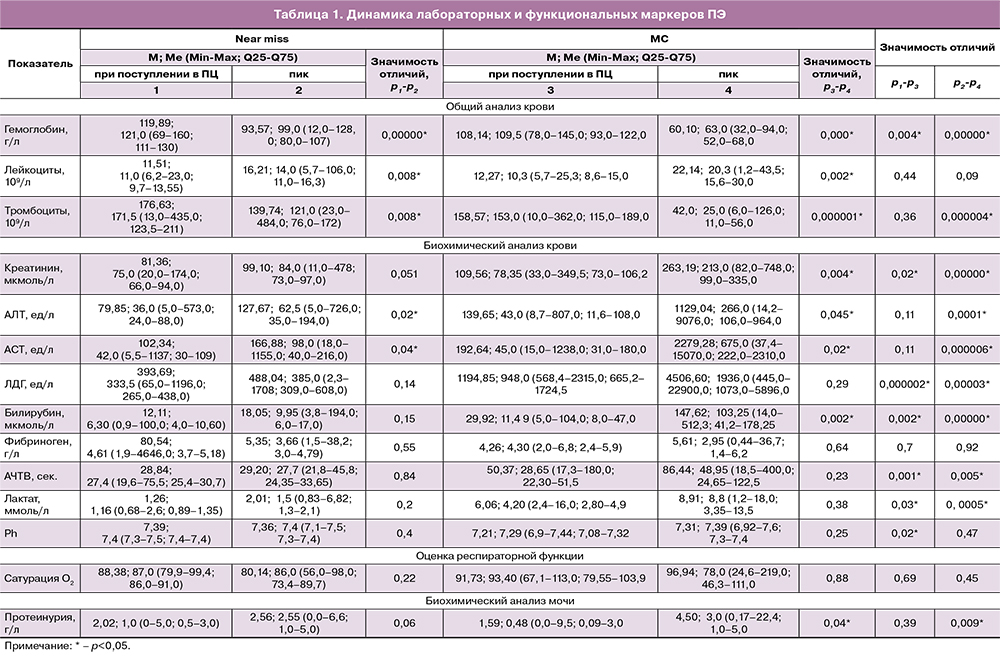
Основными маркерами, динамика которых (р<0,001) уже в течение первых суток диктовала исход угрожающего жизни состояния, явились показатели дисфункции печени (рис. 3).
Согласно имеющимся знаниям, беременность признана «тестом» для проявления имеющихся в организме женщине функциональных нарушений, способствующих развитию кардиоваскулярных и метаболических изменений, реализующихся при беременности в ПЭ, в дальнейшей жизни – в кардиоваскулярную патологию, атеросклероз [6], деменцию [19], острый инфаркта миокарда [20]. Тогда как объяснить развитие ПЭ при отсутствии АГ у женщин, например, с HELLP-синдромом [11–13, 17]? Настоящее исследование поддерживает исследования, обосновывающие необходимость пересмотра дефиниций ПЭ и ее классификации [12, 15, 21, 22], акцентирования внимания на рисках тяжелой дисфункции печени [1, 4, 11–13, 17, 18] без значительной АГ и бессимптомном течении.
Проведен поиск высокоинформативных моделей математического прогнозирования исхода угрожающего жизни состояния, основанных на диагностических маркерах ПЭ, определенных при поступлении в ПЦ (до развития угрожающего жизни состояния). Выполнен дискриминантный анализ значимости АД и протеинурии (классических маркеров ПЭ). Несмотря на то, что АГ считается основным критерием не только ПЭ, но и ее тяжести, самостоятельной дискриминирующей значимостью исходов МС или Near miss ни систолическое АД (Лямбда Уилкса=0,99, p<0,66), ни диастолическое АД (Лямбда Уилкса=0,99, p<0,89), ни протеинурия (Лямбда Уилкса=1,0, p<0,99) не обладали. Комбинация же трех параметров характеризовалась значимой дискриминацией исходов (Лямбда Уилкса: 0,73; p<0,001), но основной акцент в дискриминации привносило диастолическое АД (уровень значимости F – критерия p=0,01).
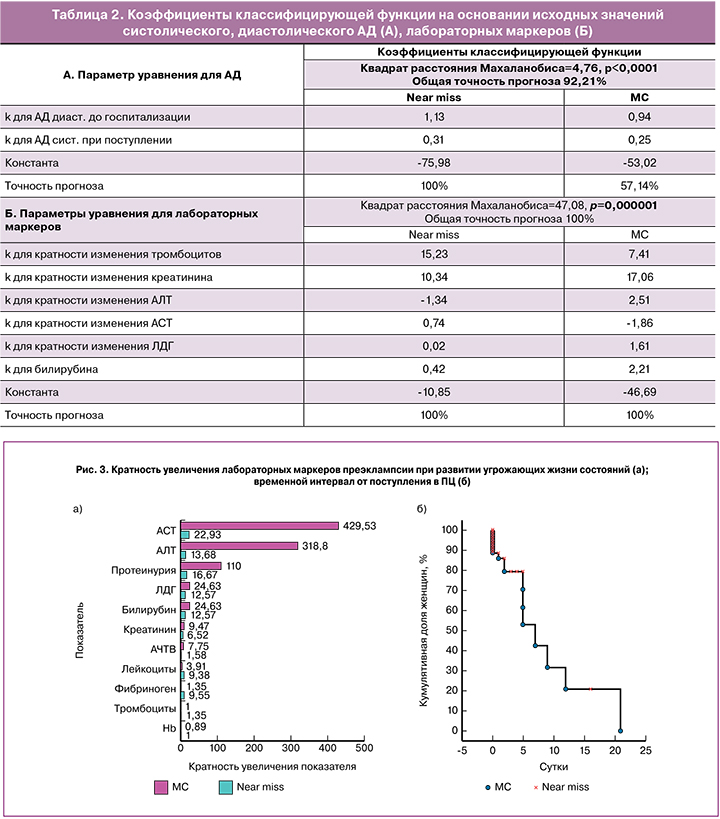
Наибольшей дискриминацией характеризовались такие параметры, как диастолическое АД, определенное на догоспитальном этапе (дома или бригадой СМП) и систолическое АД, определенное при госпитализации в ПЦ до развития угрожающего жизни состояния (Лямбда Уилкса: 0,58; p<0,0001). Полученное уравнение дискриминантной функции предоставило высокоинформативную модель прогноза с точностью 100% для Near miss, но очень низкую (57,14%) – для МС (табл. 2, А).
Модель прогноза, основанная на динамике лабораторных маркеров ПЭ (тромбоцитов, креатинина, АЛТ, АСТ, ЛДГ, билирубина) оказалась высокоинформативной (значимость дискриминации групп – лямбда Уилкса=0,26; F=12,46, p=0,000001). Точность прогноза и для Near miss, и для МС составила 100% (табл. 2, Б).
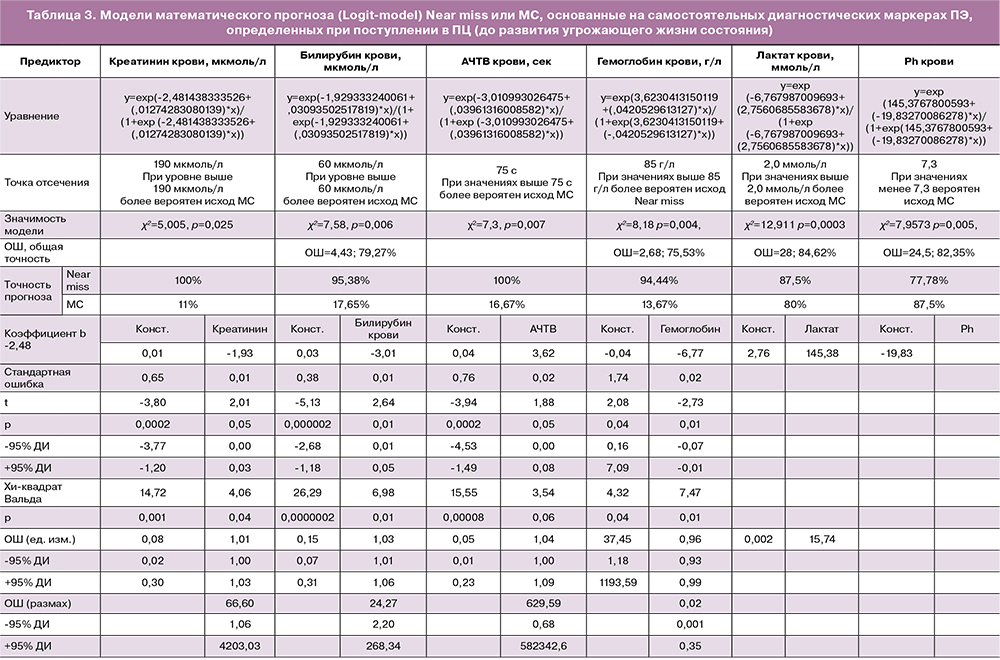
На основании отдельных параметров (предикторов) при помощи логистической регрессии (Logit-model) установлены «точки отсчета» бинарного исхода угрожающего жизни состояния (Near miss или МС) (табл. 3). Модель на основании протеинурии оказалась незначимой (χ2=0,81, p=0,37).
Полученные модели подтверждают значимость отрицательной динамики маркеров ПЭ в исходе угрожающего состояния, но не имеют решающего прикладного значения в клинической практике, так как управлять подобными изменениями практически невозможно. Риск молниеносного (менее чем за 24 ч) прогресса ПЭ до критической стадии требует не его прогнозирования, а ранней диагностики ПЭ, точной оценки ее тяжести с учетом атипичных форм, и главное – своевременного родоразрешения, не допускающего прогресс ПЭ в принципе. Срок беременности для принятия данного решения начинает отсчет с 20 недель.
Из полученных данных следует, что тяжелая ПЭ менее чем за 24 ч (медиана – 0 суток), при возрасте женщины от 18–45 лет после естественного зачатия в сроке беременности, начиная с 24 недель (в 50% – до 34 недель), при АД менее 160/100 мм рт.ст., исходном уровне креатинина от 33,0 до 349,5 мкмоль/л и его увеличении в 9,47 раз, исходном уровне тромбоцитов от 10,0 до 362,0 10⁹/л и их увеличении как в 0,04, так и 1,0 раз, исходном уровне билирубина от 5,0 до 104,0 мкмоль/л и его увеличении в 1,56–24,63 раз, исходном уровне АЛТ от 8,7 до 807,0 ед/л и ее увеличении в 1,0–318,8 раз, исходном уровне АсТ от 15,0 до 1238,0 ед/л и ее увеличении в 1,68–429,53 раз, исходном уровне ЛДГ 568,4-2315,0 ед/л и ее увеличении в 2,79–9,89 раз, отсутствии патогномоничных жалоб и при удовлетворительном общем состоянии в 22,73% случаев сопряжена с риском угрожающего жизни состояния, исходом в МС.
Показано, что ни один из рутинных предикторов ПЭ не составлял прогноз МС, значимость которого конкурировала бы показателям лактата и pH крови, которые, к сожалению, являются констатацией имеющейся, но не ожидаемой, значительной гипоперфузии тканей и ацидоза. Следовательно, данные клинико-лабораторные параметры не позволяют высокоточно прогнозировать МС до того, как развилось критическое утяжеление ПЭ, что исключает составление сценария катастрофы. Вероятно, возможность прогнозирования Near miss отражает остаточный ресурс, способность организма контролировать крайне тяжелые нарушения функции жизненно важных органов, повернуть «их вспять», что поддается математической интерпретации в виде функции (уравнения логистической регрессии). Неконтролируемые, критические нарушения (хаос), которые происходят при манифестации ПЭ вплоть до МС, перешагнувшие границы «естественных возможностей», не укладываются в математические модели, поэтому точность прогноза МС не превышает 50%, и составляет, например, 11% на основании значений креатинина или 17,65% –билирубина крови.
Заключение
Прогнозирование МС, обусловленной ПЭ, до развития тяжелой полиорганной дисфункции крайне сложно. ПЭ способна манифестировать в угрожающее жизни состояние в течение нескольких часов (до 24 ч), при возможном отсутствии АГ. Критическое нарушение функции печени конкурирует по значимости в рисках МС со значительной АГ, требует диагностики на начальной стадии с учетом бессимптомного течения. Точка отсчета от диагностики ПЭ до развития угрожающего жизни состояния может соответствовать значениям клинико-лабораторных маркеров, не относящимся не только к критериям near miss, но и тяжелой ПЭ.
Невозможность точного прогнозирования тяжелой ПЭ, раннего дебюта (с 22 недель беременности согласно полученным данным), риск молниеносного и уже неуправляемого ее прогресса определяют основополагающей тактику своевременного родоразрешения, не допускающей прогресса ПЭ, развития тяжелых, угрожающих жизни осложнений, являющейся мерой предотвращения МС.