Perinatal outcomes of monochorionic multiple pregnancies with selective intrauterine growth restriction
Monochorionic multiple pregnancy is associated with a high risk for perinatal morbidity and mortality. Perinatal loss may be frequently caused by selective intrauterine growth restriction (sIUGR) of one fetus. Objective. To assess perinatal outcomes of monochorionic multiple pregnancy complicated by selective intrauterine growth restriction of one fetus. Materials and methods. A retrospective study included 196 monochorionic pregnancies and neonatal outcomes of 376 infants. The cases were divided into two groups: the main group consisted of pregnancies with sIUGR and the control group included uncomplicated twin pregnancies. The main group was divided into subgroups according to the classification of sIUGR. Antenatal period and neonatal outcomes were compared in groups and subgroups. The D’Agostino-Pearson test, Mann-Whitney U test, and Kruskal-Wallis test were used for statistical data processing. The differences were considered significant at p<0.05. Results. Type I sIUGR was revealed in 69.8% of pregnant women, type II sIUGR – in 20.8% and type III sIUGR – in 9.4% of women. The highest weight discordance was 51% and was detected in type II subgroup, the lowest discordance was noted in type III which was 26.3% (р<0.001). Antenatal mortality in group with sIUGR was 12.5%, its highest rate was revealed in type III subgroup (44.4%). Gestational age at delivery for sIUGR pregnancies was 33.1 weeks. Earlier delivery occurred in type II and III subgroups, at 31 and 30.7 weeks’ gestation, respectively. The weight of infants with sIUGR was significantly less than one in uncomplicated pregnancies. The incidence of neurological disorders was increased in group with sIUGR (24.3%) and it was the highest in type III subgroup (58.3%). Early neonatal death occurred only in the group with sIUGR (7.9%) and was predominant in type II subgroup (28.6%). Conclusion. Monochorionic twin pregnancy complicated by sIUGR is associated with a high risk for antenatal fetal death, as well as morbidity and mortality of infants. sIUGR type is an important factor which determines pregnancy outcome and neonatal period.Kostyukov K.V., Gladkova K.A.
Keywords
Selective intrauterine growth restriction (sIUGR) is the most common complication of monochorionic multiple pregnancy, the prevalence of the restriction ranges from 10 to 25% [1]. This syndrome is accompanied by a high risk of intrauterine fetal death with growth delay and/or neurological disorders in both twins [2, 3].
The most common cause of sIUGR is an unequal placental sharing between twins [4]. Placental anastomoses play an important role in the development of the syndrome, as their type and size affect the placental perfusion of fetuses. Anastomoses can partially compensate for placental insufficiency due to interfetal hemotransfusion. However, their presence may pose additional risks for a larger fetus [5].
This syndrome is diagnosed on the basis of two consecutive ultrasound examinations performed within the interval of one or two weeks and detection of the following signs: the weight of one of the fetuses is less than the 10th percentile, the difference in the abdominal circumference of fetuses exceeds 10% and the difference in the estimated weight of twins is more than 25% [6].
The study of uterine artery blood flow is considered to be the most informative one for the assessment of the twins condition. Currently, there is a classification of sIUGR developed on the basis of the type of blood flow in the umbilical cord artery of the fetus with growth delay [7]. Type I is characterized by positive diastolic flow, type II is characterized by persistent absent or reversed end-diastolic flow, type III is characterized by intermittent absent or reversed end-diastolic flow in the umbilical artery which results from the presence of arterio-arterial anastomosis of large diameter and the impaired synchrony of fetal heart rate. Recent publications have shown that types of sIUGR are accompanied by adverse outcomes of varying degrees of severity [8, 9].
Despite the use of Doppler measurements of blood flow in the umbilical artery and the classification proposed by Gratacos E. et al. [7], the outcomes of pregnancy complicated by sIUGR can vary widely and they are extremely difficult to predict. Nowadays, there are several approaches to managing pregnancy complicated by sIUGR, such as long-term inpatient monitoring, premature delivery, selective fetocide of the twin with growth delay, fetoscopy and laser coagulation of placental anastomoses. However, there is no reliable data on which option is correct.
Thus, the issue of studying the characteristics of pregnancy and perinatal outcomes in monochorionic twins complicated by sIUGR and its different types remains relevant.
The aim of this investigation was to study the characteristics of the course of monochorionic multiple pregnancy and perinatal outcomes in sIUGR.
Materials and Methods
This was a retrospective study of 196 monochorionic pregnancies and neonatal outcomes of 376 infants that were monitored and given birth between 2014 and 2019 in the National Medical Research Centre for Obstetrics, Gynecology and Perinatology, Moscow.
The inclusion criterion was monochorionic diamniotic twin pregnancy.
The exclusion criteria were monochorionic monoamniotic twins, dichorionic diamniotic twins, high-order multiple gestations (triplets or higher), unknown chorionicity, genetic abnormalities in one or both fetuses, twin-twin transfusion syndrome, anemiapolycythemia sequence, and reverse arterial perfusion syndrome in monochorionic twins.
Gestation period was calculated from the first day of last menstruation or on the basis of crown-rump length of the larger fetus measured at 10–14 weeks’ gestation.
The type of chorionicity and amnionicity in multiple pregnancies was determined before 14 weeks of pregnancy on the basis of echographic assessment. Monochorionic diamniotic pregnancies were confirmed by the presence of a single gestation sac (one chorion) containing two live fetuses and two amnions (the presence of a T-sign).
sIUGR was diagnosed on the basis of the following criteria: the weight of one fetus was less than the 10th percentile, and/or the difference in the abdominal circumference of fetuses exceeded 10%, and/or the difference in the estimated weight of twins was more than 25% according to two consecutive ultrasound examinations performed within the interval of one or two weeks. Birth weight discordance was calculated with the help of the following formula: ((A – B) · 100)/A, where A is the larger twin weight and B is the smaller twin weight.
All patients were divided into two groups: group I (control) included 100 monochorionic diamniotic twin pregnancies with symmetrical fetal growth; group II (main) included 96 monochorionic diamniotic twin pregnancies complicated by sIUGR. According to the classification proposed by E. Gratacos et al., the main group was divided into three subgroups depending on sIUGR type [7]. Changes in blood flow in the umbilical cord artery of the fetus with growth delay are used as the basis for the classification of sIUGR. There are three types of blood flow depending on changes in the diastolic component: type I is characterized by the presence of a diastolic component, type II – zero or reverse blood flow, and type III – intermittent blood flow.
The evaluation of the antenatal course of pregnancy was based on the data on intrauterine fetal death, the mode of delivery (urgent delivery, planned delivery), indications for delivery (fetal, maternal).
The assessment of the neonatal outcomes included gestational age and birth weight, Apgar scores at one and five minutes of life, hospitalization and length of stay in neonatal intensive care unit, disorders of the respiratory system, central nervous system and other systems, early neonatal mortality. Long-term outcomes in patients discharged from hospital were not evaluated in this study.
Statistical analysis
Statistical processing and graphing were performed using Microsoft Excel spreadsheets and GraphPad Prism 8 software package (GraphPad Software, USA). The D’Agostino–Pearson test was used to determine the normality of the distribution. Data with a normal distribution are presented as an average value (standard deviation), and t-test was used for their comparison. Data with a distribution other than normal are presented as a median (interquartile range), the Mann–Whitney criterion was used for their comparison. Qualitative data are presented as an absolute value (n) and %, Fisher’s exact test was used for their comparison. The differences were considered statistically significant at the level of p<0.05. The study was approved by the Local Ethics Committee of the National Medical Research Center for Obstetrics, Gynecology and Perinatology, Moscow, Russia.
Results
This was a retrospective analysis of the course of 196 monochorionic diamniotic pregnancies including 96 pregnancies complicated by sIUGR (main group) and 100 uncomplicated twin pregnancies (control group). Type I sIUGR was revealed in 69.8% of pregnant women (n=67), type II sIUGR – in 20.8% (n=20) and type III sIUGR – in 9.4% of women (n=9). The average period of diagnosing different types of sIUGR did not differ statistically. It was 23.2 weeks for type I, 21.7 weeks for type II, and 22.3 weeks for type III, p=0.34.
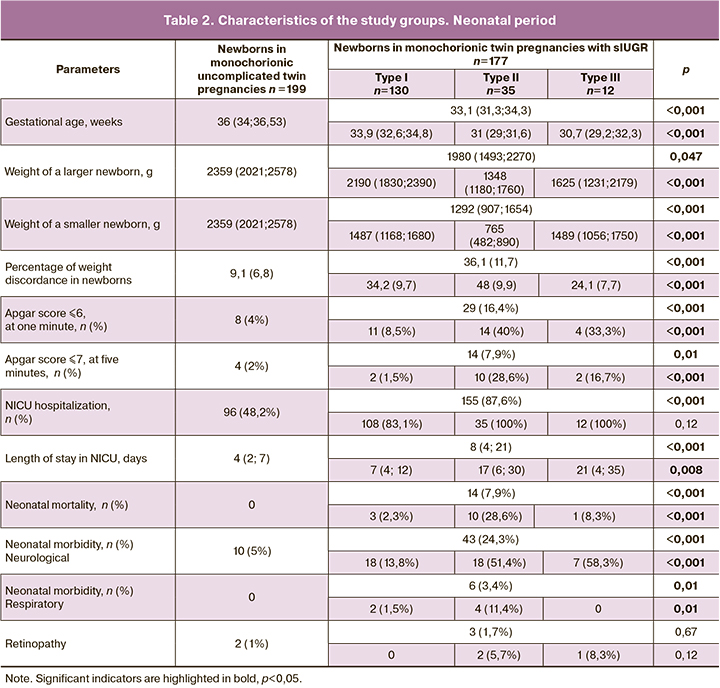
The age of pregnant women in the study groups did not differ statistically. Comparison of the age of pregnant women in subgroups did not reveal any statistically significant differences either.
Significant differences in the study groups as well as subgroups were not found in such parameters as the body mass index of pregnant women, parity, rate of pregnancies following assisted reproductive technologies, and pregnancy complications such as gestational diabetes and preeclampsia.
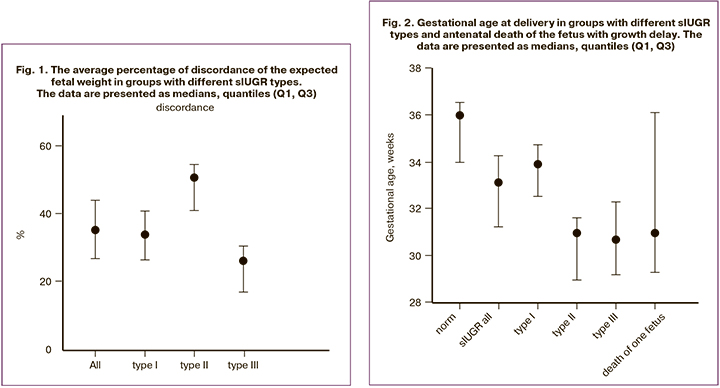
The average percentage of discordance of the expected fetal weight was calculated in the subgroups for each type of sIUGR on the basis of several ultrasound investigations. The highest median percentage of discordance of the expected weight was found in type II sIUGR – 51% (41.3; 54.8), the lowest was revealed in type III – 26.3% (17.1; 30.4). In type I, the median of the average discordance percentage was 34 (26.6; 41), p<0.001 (Fig. 1).
The cases of antenatal death in the study cohort were analyzed thoroughly, antenatal mortality rate was 6.6% (n=13). This indicator prevailed in the group with sIUGR – 12.5% (n=12) compared to the control group – 1% (n=1), p=0.001; the odds ratio (OR) is 14.1, 95% confidence interval (CI) is 2.5–153.1. Comparison of antenatal mortality rate in subgroups showed its predominance in type III sIUGR –44.4% (n=4); this indicator was 20% (n=4) in type II, and 5.9% (n=4) in type I, p = 0.02. Antenatal death of both twins occurred in three cases (3.1%) in the main group, in two patients from type III sIUGR subgroup and in one patient from type II subgroup. The average gestation period when antenatal death was diagnosed was 29.1 weeks. There was no statistically significant difference in the period of antenatal death depending on the sIUGR type: type I – 29.6 weeks, type II – 28.2 weeks, and type III – 29.4 weeks, p=0.39.
There were statistically significant differences in the indications for delivery. The pregnant women with monochorionic twins with sIUGR were significantly more frequently delivered for fetal indications, namely in 50% of cases (n=48). Delivery for fetal indications was performed only in 9% of cases (n=9) in patients from the control group, p<0.001. Assessment of the rate of delivery for fetal indications in subgroups showed its predominance in type II sIUGR (75%) and type III sIUGR (77.8%), compared with type I (38.8%), p=0.004.
The most common mode of delivery in the study groups was cesarean section which was performed in 83.7% of cases. Its rate significantly differed in the main (91.7%) and control (76%) groups, p=0.004. The comparison of operative delivery rate depending on sIUGR type did not reveal any significant differences, p=0.81.
The majority of pregnant women, namely 137 (69.9%) patients, had preterm birth before 36 weeks. The rate of delivery of women pregnant with monochorionic twins with sIUGR before 36 weeks was 91.7% (n=88), in case of uncomplicated pregnancies its rate was 49% (n=49), p<0.001.The comparison of the rate of preterm birth before 36 weeks in the subgroups did not show any significant differences, p=0.15.
The study also assessed the effect of antenatal death of the fetus with growth delay on the delivery time of the surviving twin. The median delivery time for this complication was 31 weeks. The average period of pregnancy prolongation was 3.75 weeks, ranging from 1 day to 12 weeks. The comparison of the delivery time in the subgroups with antenatal death of the fetus with growth delay and subgroups without fetal antenatal death did not reveal a statistically significant difference, p=0.18 (Fig. 2).
Clinical characteristics of pregnant women and the antenatal period in the study groups are presented in Table 1.
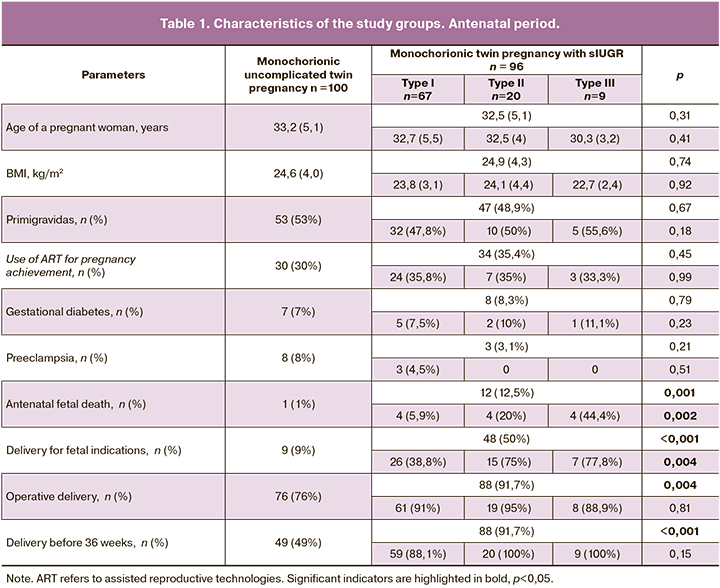
The comparison of the gestational age of newborns showed a significant difference in the study groups. The median gestational age of monochorionic twins complicated by sIUGR was 33.1 weeks, while the median gestational age in uncomplicated pregnancies was 36 weeks, p<0.001. This indicator also differed statistically in subgroups: the lowest gestational age was found in types II and III sIUGR subgroups, 31 and 30.7 weeks, respectively, and it was 33.9 weeks in type I subgroup, p<0.001.
The weight of all newborns in the control group was compared separately with the larger and smaller twins in the main group. Similar division was carried out in subgroups. The analysis showed significantly lower median values for monochorionic twins complicated by sIUGR in comparison with uncomplicated pregnancies, p<0.001. This was typical not only for a newborn with growth delay, but also for a newborn with normal growth. The comparison in subgroups revealed the presence of a statistically significant difference in type II subgroup, the median weight of both the larger and smaller twins was significantly less than weight in types I and III subgroups, p<0.001. Therefore, the average percentage of newborn weight discordance also differed depending on sIUGR type: it was 34.2% in type I subgroup, 48% in type II subgroup, 24.1% in type III subgroup, p<0.001.
Newborn’s condition was assessed according to the Apgar score. In each group, we calculated the number of infants who had a score of 6 points or less at one minute of life and 7 points or less at five minutes. In the group of monochorionic twins complicated by sIUGR, the number of children with low Apgar scores was significantly higher than in the group with uncomplicated pregnancy: at one minute of life it was 16.4% and 4%, at five minutes of life it was 7.9% and 2%, respectively, p<0.001. The largest number of newborns with sIUGR with low Apgar scores was found in types II and III subgroups: 40% and 33.3% at one minute, 28.6% and 16.7% at five minutes, respectively; the number of newborns was significantly lower in type I subgroup, 8.5% at one minute and 1.5% at five minutes, p <0.001.
The comparison of the frequency of neonatal complications showed their predominance in the group with monochorionic twins complicated by sIUGR. Thus, the rate of neonatal intensive care unit (NICU) hospitalization of the newborns with sIUGR was higher than one in uncomplicated pregnancies, 87.6% and 48.2%, respectively, p<0.001. Comparison of this indicator in subgroups did not reveal statistically significant differences.
The stay of newborns in NICU was also longer in the group with sIUGR, the longest stay was noted in types II and III subgroups. The median duration of hospitalization in NICU in group with monochorionic twins complicated by sIUGR was 8 days, while in case of uncomplicated pregnancy it was 4 days, p<0.001. The longest hospitalization in NICU was detected in types II and III subgroups, 17 and 21 days, in type I subgroup this indicator was 7 days, p=0.008.
The analysis of neonatal morbidity revealed an increase in the rate of neurological complications in newborns with sIUGR compared with the control group, 24.3% versus 5%, respectively, p<0.001. The rate of neurological disorders was significantly higher in types II and III sIUGR compared with type I, 51.4, 58.3%, 13.8%, respectively, p<0.001.
Respiratory disorders in newborns were detected only in types I and II sIUGR. Comparison of the rate of neonatal retinopathy in groups and subgroups showed no significant differences.
The cases of early neonatal mortality were observed only in the group of newborns with sIUGR. The frequency of this indicator was 7.9% (n=14). Among 14 dead newborns, 5 infants (35.7%) were large twins, 9 newborns (64.3%) were smaller, p=0.26. Analysis of neonatal mortality in subgroups showed its predominance in type II sIUGR (28.6%). In order to study mortality cases in detail, such indicators as the time and mode of delivery, as well as the weight of newborns were analyzed. The presence of a statistical difference in the delivery period was revealed: dead infants were born at 29 (27.9; 31.5) weeks, while the median delivery in the group with sIUGR was 33.14 (31.3; 34.3) weeks, p<0.001. The mode of delivery did not affect the rate of neonatal mortality, since all the children who died were born by caesarean section. The median values of the weight of dead children were statistically different from the weight of surviving newborns with growth delay, 705 (487; 1053) and 1292 (907; 1654) grams, respectively, p=0.001.
Clinical characteristics of newborns and neonatal period in the study groups are presented in Table 2.
Discussion
Growth restriction of one of the fetuses is one of the specific complications of multiple pregnancy [10]. If the expected fetal weight is less than the 10th percentile [11] and/or the difference between the expected weight of twins is more than 25% [12], the term ‘selective fetal growth restriction’ is applied. Being one of the most frequent complications of monochorionic multiple pregnancy, sIUGR often leads to intrauterine death of one or both fetuses, and/or the development of neurological disorders in twins [2, 3].
The main reason for the development of sIUGR is unequal placental sharing, as well as the presence of vascular anastomoses [4]. It is known that the degree of unequal placental sharing correlates with the severity of fetal weight discordance, and the presence of placental anastomoses can partially compensate for placental insufficiency [5]. Different types of sIUGR are also known to be characterized by different variants of placental angioarchitectonics; the most remarkable unequal placental sharing was noted in type II subgroup, the presence of a large arterio-arterial anastomosis was detected in type III. In this study, the discordance of the expected fetal weight in different types of sIUGR was evaluated. The greatest discordance was found in type II, which can be explained by a remarkable unequal placental sharing, and the lowest discordance was noted in type III as the presence of placental anastomoses compensated for placental insufficiency.
Recent publications have indicated a link between the severity of discordance in the weight of twins and perinatal morbidity and mortality [13].
Antenatal death of one or both fetuses in monochorionic twins is one of the most dangerous complications of pregnancy. It is worth noting that in the monochorionic type of placentation, its frequency is significantly higher than in the dichorionic type, 19.1 versus 6.5 per 1000 newborns, respectively [14]. The rate of antenatal mortality in this study was 6.6%. The analysis of mortality in groups showed its correlation with sIUGR, the risk of antenatal death in complicated monochorionic twins was 14.1 times higher (OR 14.1, 95% CI: 2.5–153.1), compared with uncomplicated pregnancy.
It is known that impaired blood flow is often detected in the umbilical artery of a fetus with growth delay, different forms of its severity formed the basis of classification [7]. The fetal condition correlates with the pulsation index and the type of end-diastolic flow. The most favorable disturbance of blood flow in the umbilical cord arteries is accompanied by an increase in the values of the pulsation index above 95 percentiles while maintaining a positive end-diastolic flow, which is typical for type I sIUGR. Absent and reversed end-diastolic blood flow occurs as a result of combination of the increased resistance to blood flow and decrease in the contractile activity of the myocardium due to decompensation. The types of blood flow typical for type II sIUGR are more unfavorable in comparison with the positive enddiastolic flow. Type III sIUGR is characterized by intermittent blood flow, which occurs in the presence of arterio-arterial anastomosis of a large diameter and the impaired synchrony of fetal heart rate [7].
In accordance with the above-mentioned facts, different types of sIUGR are characterized by different antenatal mortality rate. Most recent publications on the classification of sIUGR types have confirmed that types II and III are most often accompanied by an adverse outcome [9, 15]. These findings are consistent with the results of our study, types II and III sIUGR are characterized by a higher antenatal mortality rate than type I. The highest rate was observed in type III sIUGR – 44.4% (n=4), this indicator was 20% (n=4) in type II, and 5.9% (n=4) in type I, p=0.02. Particular attention should be given to the antenatal death of both twins, which occurred in three cases, two of them were in type III subgroup and one case was in type II subgroup. The high antenatal mortality rate in type III subgroup can be explained by the influence of a large arterio-arterial anastomosis, through which rapid and massive transfusion from one fetus to another can be performed. The analysis of the time of antenatal death in the observed cohort showed that the average gestational age when antenatal death was diagnosed was 29.1 weeks. There was no statistically significant difference in the period of antenatal death depending on the type of sIUGR. Tul et al. performed a prospective study on 387 monochorionic twins and revealed a significant increase in the risk of antenatal death after 33 weeks which was 6.2% [16].
The majority of pregnant women included in the study (83.7%) were performed cesarean section. A similar rate of operative delivery of twins (about 94%) was demonstrated by Carter et al. [17]. In the study groups, there was a difference in the frequency of cesarean section with its predominance in sIUGR groups. At the same time, the difference in the types of sIUGR subgroups did not influence the frequency of operative delivery.
It is known that gestational age at delivery is the main determinant of perinatal outcome, both in single and multiple pregnancies [18]. The rate of preterm birth in multiple pregnancies ranges from 54.4% to 87%, which is significantly higher than one in single pregnancies [19]. Patients with a pregnancy complicated by sIUGR are delivered prematurely due to the risk of death of a fetus with growth delay, which is also consistent with the results of our study. In this study, 49% of pregnant women with uncomplicated monochorionic twin pregnancy were delivered before 36 weeks. The frequency of delivery before 36 weeks in the group with sIUGR was 91.7%. In type II and III subgroups, 100% of pregnant women were delivered before 36 weeks. This is due to the high risk of antenatal fetal death in these types of syndrome. Accordingly, this was also confirmed by the prevalence of delivery for fetal indications in the group with complicated pregnancy.
It is natural that the body weight of newborns in monochorionic twin pregnancy with sIUGR was less than that of children from the control group. This is due to both the smaller weight of the newborn with growth delay, and the earlier delivery of these patients.
The comparison of the neonatal outcomes presented in our study showed the association of fetal sIUGR and morbidity and mortality of newborns. Unsatisfactory condition of newborns, accompanied by low scores on the Apgar scale, was more frequently revealed in the group with complicated monochorionic pregnancy. Newborns with sIUGR were more often hospitalized in the NICU, which was also accompanied by their longer stay in the hospital. It is natural that neonatal morbidity in the group with complicated monochorionic pregnancy was higher. According to a number of authors, the frequency of neonatal complications, such as sepsis, neurological and respiratory disorders, is higher in newborns with sIUGR [9]. D’antonio et al. showed in their study that the risk of neurological disorders increases with the growing delay in height and weight indicators in infants with sIUGR [13]. The analysis of neonatal morbidity depending on the type of sIUGR showed its predominance in type II and III subgroups. This may be caused by earlier delivery of pregnant women in types II and III sIUGR subgroups compared to type I. Type II subgroup is characterized by the highest discordance in the weight of newborns, most complications were also observed in infants with growth delay. Moreover, it is noteworthy that high frequency of neurological disorders was detected in newborns with type III sIUGR. According to E. Gratacos et al., this is due to the presence of a large arterio-arterial anastomosis, through which massive hemotransfusion can occur from one fetus to another causing a dramatic decrease in the volume of circulating blood and leading to hypoxia [15].
The cases of early neonatal mortality were observed only in the group of newborns with sIUGR. It is possible that the high rate of early neonatal mortality of newborns in monochorionic twin pregnancies complicated by sIUGR may result from prematurity. This is confirmed by the fact that the gestational age at delivery of dead infants was lower (29 weeks) than one in other cases of sIUGR (33.14 weeks). However, according to Di Maschio et al., the analysis of the outcomes of newborns in multiple pregnancy delivered after 34 weeks showed a high risk of neonatal morbidity and mortality among newborns with growth delay [20]. This allowed the authors to suggest that sIUGR is an independent factor that negatively affects perinatal outcome at later gestational age. The median weight values of dead infants were statistically different from the weight of surviving infants with growth delay, 705 and 1292 grams, respectively, and confirm the results of the above-mentioned study.
This study provided information about the role of sIUGR in the development of perinatal complications in monochorionic multiple pregnancy. This issue requires closer monitoring, since this pregnancy is accompanied by a high perinatal risk (risk of fetal death, high neonatal mortality, neurological and respiratory morbidity of newborns). The comparison of the rate of complicated course of pregnancy and the critical condition of newborns showed that they were more frequent in type II and III subgroups. The risk of antenatal complications in these types of sIUGR leads to earlier delivery. In this case, a number of complications of the neonatal period can be associated with prematurity.
The strong point of the study is a sufficient sample of 196 pregnant women and 376 newborns; pregnancy management, delivery and nursing of newborns in the departments of one institution.
The main limitation of this study is its retrospective design.
Thus, further research is needed to find predictors of antenatal complications, which would make it possible to prolong a pregnancy complicated by sIUGR.
Conclusion
Monochorionic multiple pregnancy complicated by sIUGR is associated with a high risk of perinatal complications in comparison with uncomplicated monochorionic twin pregnancy. Types II and III sIUGR are most often accompanied by adverse outcomes, namely antenatal death of fetus or fetuses, early neonatal mortality, and neurological disorders.
References
- Lewi L., Jani J., Blickstein .I, Huber A., Gucciardo L., Van Mieghan T. et al. The outcome of monochorionic diamniotic twin gestations in the era of invasive fetal sugery: a prospective cohort. Am J Obstet. Gynecol. 2008; 199: 514.e1–8.
- Gratacós E., Carreras E., Becker J., Lewi L., Enríquez G., Perapoch J. et al. Prevalence of neurological damage in monochorionic twins with selective intrauterine growth restriction and intermittent absent or reversed end-diastolic umbilical artery flow. Ultrasound Obstet. Gynecol. 2004; 24(2): 159-63. https://dx.doi.org/10.1002/uog.1105.
- Sebire N.J., Snijders R.J., Hughes K., Sepulveda W., Nicolaides K.H. The hidden mortality of monochorionic twin pregnancies. Br. J. Obstet. Gynaecol. 1997; 104(10): 1203-7. https://dx.doi.org/10.1111/j.1471-0528.1997.tb10948.x.
- Victoria A., Mora G., Arias F. Perinatal outcome, placental pathology, and severity of discordance in monochorionic and dichorionic twins. Obstet. Gynecol. 2001; 97(2): 310-5. https://dx.doi.org/10.1016/s0029-7844(00)01111-x.
- Lewi L., Gucciardo L., Huber A., Jani J., Van Mieghem T., Doné E. et al. Clinical outcome and placental characteristics of monochorionic diamniotic twin pairs with early- and late-onset discordant growth. Am. J. Obstet. Gynecol. 2008; 199(5): 511. e1-7. https://dx.doi.org/10.1016/j.ajog.2008.04.022.
- Костюков К.В., Гладкова К.А. Диагностика синдрома селективной задержки роста плода, синдрома обратной артериальной перфузии при монохориальной многоплодной беременности. Акушерство и гинекология. 2016; 2: 14-8. [Kostyukov K.V., Gladkova K.A. Diagnosis of selective fetal growth restriction syndrome and reversed arterial perfusion in monochorionic multiple pregnancy. Akusherstvo i ginekologiya/Obstetrics and Gynecology. 2016; (2): 14-8. (in Russian)]. https://dx.doi.org/10.18565/aig.2016.2.14-18.
- Gratacós E., Lewi L., Munoz B., et al. A classification system for selective intrauterine growth restriction in monochorionic pregnancies according to umbilical artery Doppler flow in the smaller twin. Ultrasound Obstet Gynecol 2007; 30: 28-34.
- Miller J., Chauhan S.P., Abuhamad A.Z. Discordant twins: diagnosis, evaluation and management. Am. J. Obstet. Gynecol. 2012; 206(1): 10-20. https://dx.doi.org/10.1016/j.ajog.2011.06.075.
- Valsky D.V., Eixarch E., Martinez J.M., Crispi F., Gratacós E. Selective intrauterine growth restriction in monochorionic twins: pathophysiology, diagnostic approach and management dilemmas. Semin. Fetal Neonatal Med. 2010; 15(6): 342-8. https://dx.doi.org/10.1016/j.siny.2010.07.002.
- Lewi L., Devlieger R., De Catte L., Deprest J. Growth discordance. Best Pract. Res. Clin. Obstet. Gynaecol. 2014; 28(2): 295-303. https://dx.doi.org/10.1016/j.bpobgyn.2013.12.003.
- Ananth C.V., Vintzileos A.M., Shen-Schwarz S., Smulian J.C., Lai Y.L. Standards of birth weight in twin gestations stratified by placental chorionicity. Obstet. Gynecol. 1998; 91(6): 917-24. https://dx.doi.org/10.1016/s0029-7844(98)00052-0.
- O’Brien W.F., Knuppel R.A., Scerbo J.C., Rattan P.K. Birth weight in twins: an analysis of discordancy and growth retardation. Obstet. Gynecol. 1986; 67(4): 483-6.
- D’Antonio F., Khalil A., Dias T., Thilaganathan B.; Southwest Thames Obstetric Research Collaborative (STORK). Weight discordance and perinatal mortality in twins: analysis of the Southwest Thames Obstetric Research Collaborative (STORK) multiple pregnancy cohort. Ultrasound Obstet. Gynecol. 2013; 41(6): 643-8. https://dx.doi.org/10.1002/uog.12412.
- Southwest Thames Obstetric Research Collaborative (STORK). Prospective risk of late stillbirth in monochorionic twins: a regional cohort study. Ultrasound Obstet. Gynecol. 2012; 39(5): 500-4. https://dx.doi.org/10.1002/uog.11110.
- Gratacós E., Antolin E,. Lewi L., Martínez J.M., Hernandez-Andrade E., Acosta-Rojas R. et al. Monochorionic twins with selective intrauterine growth restriction and intermittent absent or reversed end-diastolic flow (Type III): feasibility and perinatal outcome of fetoscopic placental laser coagulation. Ultrasound Obstet. Gynecol. 2008; 31(6): 669-75. https://dx.doi.org/10.1002/uog.5362.
- Tul N., Verdenik I., Novak Z., Srsen T.P., Blickstein I. Prospective risk of stillbirth in monochorionic-diamniotic twin gestations: a population based study. J. Perinat. Med. 2011; 39(1): 51-4. https://dx.doi.org/10.1515/jpm.2010.110.
- Carter E.B., Bishop K.C., Goetzinger K.R., Tuuli M.G., Cahill A.G. The impact of chorionicity on maternal pregnancy outcomes. Am. J. Obstet. Gynecol. 2015; 213(3): 390. e1-7. https://dx.doi.org/ 10.1016/j.ajog.2015.05.027.
- Callaghan W.M., MacDorman M.F., Rasmussen S.A., Qin C., Lackritz E.M. The contribution of preterm birth to infant mortality rates in the United States. Pediatrics. 2006; 118(4): 1566‐73. https://dx.doi.org/10.1542/peds.2006-0860.
- Fumagalli M., Schiavolin P., Bassi L., Groppo M., Uccella S., De C.A. et al. The impact of twin birth on early neonatal outcomes. Am. J. Perinatol. 2016; 33(1): 63-70. https://dx.doi.org/10.1055/s-0035-1556881.
- Di Mascio D., Acharya G., Khalil A., Odibo A., Prefumo F., Liberati M. et al. Birthweight discordance and neonatal morbidity in twin pregnancies: a systematic review and meta‐analysis. Acta Obstet. Gynecol. Scand. 2019; 98(1): 1245‐57. https://dx.doi.org/10.1111/aogs.13613.
Received 05.02.2020
Accepted 25.03.2020
About the Authors
Kirill V. Kostyukov, MD, PhD, Department of the Functional Diagnosis Academician V.I. Kulakov Research Center of Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia. Tel.: +7(926)214-97-84. E-mail: kostyukov_k@yahoo.com.4, Oparina str., Moscow, 117997, Russian Federation.
Kristina A. Gladkova, MD, PhD, research fellow, Obstetrics Pathology Department Academician V.I. Kulakov Research Center of Obstetrics, Gynecology and Perinatology, Ministry of Health of Russia. Tel.: +7(916)321-10-07. E-mail: k_gladkova@oparina4.ru.
4, Oparina str., Moscow, 117997, Russian Federation.
For reference: Kostyukov K.V., Gladkova K.A. Perinatal Outcomes of Monochorionic Multiple Pregnancies with Selective Intrauterine Growth Restriction.
Akusherstvo i Ginekologiya / Obstetrics and gynecology. 2020; 6: 50-58 (in Russian)
https://dx.doi.org/10.18565/aig.2020.6.50-58