Perinatal outcomes of monochorionic multiple pregnancies complicated by twin-to-twin transfusion syndrome
Relevance. Monochorionic multiple pregnancies complicated by twin-to-twin transfusion syndrome carry a high risk of perinatal morbidity and mortality. Aim. To investigate perinatal outcomes of monochorionic multiple pregnancies complicated by TTTS. Material and methods. This prospective study comprised 253 monochorionic pregnancies, including 153 pregnancies complicated by TTTS (study group) and 100 uncomplicated pregnancies (control group). The study group was divided into subgroups categorized as treated with laser coagulation of placenta anastomoses (n = 126), amnioreduction (n = 11), and having no in utero treatment of TTTS (n = 16). The groups and subgroups were compared regarding the course of the antenatal period and the neonatal outcomes. Differences were considered significant at p <0.05. Results. The antenatal death rates in patients with TTTS and control groups were 51.6% and 1%, respectively. The term of delivery in patients with and without TTTS was 31.8 and 36.0 weeks, respectively. The earliest term of delivery was observed among patients undergoing amnioreduction (29.6 weeks) and having no in utero treatment (27.1 weeks). Birthweight of newborns from pregnancies affected by TTTS was significantly lower than that from uncomplicated pregnancies. Neurological morbidity was higher among TTTS infants (26.2%) and was highest in the subgroups of amnioreduction and uncomplicated pregnancy (47.1% and 46.7%). Respiratory disorders were detected only in the study group and had the highest rates in subgroups II and III. Early neonatal mortality was noted only among newborns from pregnancies affected by TTTS (10.8%). Conclusion. Monochorionic twin pregnancies complicated by TTTS are associated with a high risk of antenatal fetal death and neonatal morbidity and mortality. Laser coagulation of placental vascular anastomoses improves perinatal outcomes in TTTS.Kostyukov K.V., Sakalo V.A., Gladkova K.A., Shakaya M.N., Ionov O.V., Tetruashvili N.K.
Keywords
Twin-to-twin transfusion syndrome (TTTS) is one of the most severe conditions that affects 10% to 15% of twin pregnancies with monochorionic diamniotic placentation [1].
TTTS occurs when there is an unbalanced distribution of placental blood vessels between fetuses, which leads to a disproportionate supply of blood delivered [2, 3]. As a result, the blood that would normally go to the donor twin is diverted to the recipient twin, causing a reduction in blood volume in the donor twin and excess of blood in the recipient twin. This leads to significant changes in the cardiovascular systems of both twins [4]. In the absence of treatment, TTTS is associated with more than 95% perinatal morbidity and mortality. Newborns from pregnancies affected by TTTS have a high incidence of cardiovascular (87%), neurological (70%), and respiratory disorders (92%) [5].
Timely diagnosis and optimal management strategy for TTTS are critical for improving perinatal outcomes. Currently, there are several treatment options for TTTS, including selective feticide of the co-twin, fetoscopic laser coagulation of placental anastomoses, and serial amnioreduction.
Selective feticide of the co-twin is used in severe cases where one twin has development anomalies, when there is selective growth restriction of one of the twins (with inter-pair weight discordance of greater than 40% and before 22 weeks’ gestation), and at stage IV TTTS when no other treatment is possible.
Amnioreduction is a palliative treatment for TTTS that involves the removal of the excess fluid from around the recipient twin. This helps reduce the risk of preterm birth and improve to some extent, the placental perfusion. Usually, amnioreduction is used in stage I TTTS, when the diagnosis is made after 26 weeks’ gestation, or after TTTS recurrence due to incomplete coagulation of the anastomoses, or a lack of technical capacity to perform laser coagulation.
Fetoscopic laser coagulation of vascular anastomoses on the placenta is a pathogenetically oriented treatment of TTTS since it is aimed at eliminating the cause of the disease. The implementation of this method into clinical practice has been associated with a reduction in neonatal morbidity and mortality.
Therefore, further investigation of perinatal outcomes in monochorionic twin pregnancies complicated by TTTS at its various stages and different treatment approaches would have been relevant.
The present study aimed to investigate the course and perinatal outcomes of monochorionic multiple pregnancies complicated by TTTS and the effectiveness of different management strategies for this pregnancy complication.
Material and methods
This prospective study was conducted at the V.I. Kulakov NMRC for OG&P of Minzdrav of Russia from 2014 to 2019 and included 253 patients with monochorionic diamniotic pregnancies.
Eligible for inclusion in the study were monochorionic twin pregnancies complicated or not complicated by TTTS.
Exclusion criteria were monochorionic monoamniotic twin pregnancy, dichorionic diamniotic twin pregnancy, higher-ordermultiplepregnancies(triplets, quadruplets), unknown chorionicity, chromosomal abnormalities in one or both twins, and the twin reversed arterial perfusion sequence in monochorionic twins.
The gestational age was calculated based on the first day of the woman's last menstrual period or the crown-rump length (CRL) of the larger fetus measured at 11–136 weeks' gestation. In pregnancies resulting from assisted reproductive technology, gestational age was calculated based on the date of embryo transfer, taking into account the time of cultivation.
The type of chorionicity and amnionicity in multiple pregnancies was determined by ultrasonography before 14 weeks' gestation. Monochorionic diamniotic twin pregnancy was identified by the presence of a single gestational sac containing two live fetuses and two amnions (a T-sign).
Diagnosis of fetal-fetal transfusion syndrome was based on the presence of oligohydramnios (defined as a maximal vertical pocket (MVP) of <2 cm) in the donor twin and of polyhydramnios (MVP >8–10 cm) in the recipient twin. The severity of TTTS was assessed according to the Quintero staging system [6].
The whole study cohort was divided into a study group of women with monochorionic diamniotic twin pregnancies complicated by TTTS (n=153) and a control group with uncomplicated monochorionic diamniotic twin pregnancies (n=100). The study group then was categorized into subgroups as treated with laser coagulation of placental anastomoses (n= 126), amnioreduction (n=11), and having no in utero treatment of TTTS (n=16). The management strategy was based on the time of diagnosis or admission to the Center, the TTTS stage, and the technical feasibility of performing the surgical treatment. Subgroup 1 included 126 patients with stage I–IV TTTS who underwent fetoscopy-guided laser coagulation of placental anastomotic vessels before 27 weeks of pregnancy. Subgroup 2 was made up of 11 patients with stage I–II TTTS who underwent serial amnioreduction because they were admitted after 26 weeks of pregnancy, or there was no technical feasibility of fetoscopy. Subgroup 3 consisted of 16 pregnant women with TTTS who did not undergo in utero treatment due to stage V TTTS or spontaneous miscarriage before fetoscopy.
Fetoscopic laser coagulation of placental anastomotic vessels was performed by transabdominal access under local anesthesia. Prophylactic antibiotics (II–III generation cephalosporins) and tocolytics (the choice was made on a case-by-case basis) were administered. A 2.3–3.3 mm fetoscopic trocar was inserted under continuous ultrasound guidance into the in the recipient amniotic cavity. Then a fetoscope with a laser energy conductor was inserted, and anastomoses were coagulated without contact with the tissue. The operation was completed by amnioreduction until the normal amount of amniotic fluid volume (MVP 4–6 cm).
Serial amnioreduction was performed under local anesthesia and continuous ultrasound guidance. An 18G needle was inserted through the maternal abdominal wall, uterine wall, and into the amniotic sac of the recipient twin. Amniotic fluid was removed until normal volume (MVP<8 cm). The procedure was repeated based on the appearance and growth of polyhydramnios in the recipient twin.
Analysis of the pregnancy course included identification of complications, data on intrauterine death of one or both twins, time and type of delivery (emergency, planned), and indications for delivery (fetal, maternal).
Neonatal outcomes included gestational age and weight-and-height parameters at birth, 1-minute and 5-minute Apgar score, length of stay in the neonatal intensive care unit, respiratory disorder incidence rates, damage to CNS (intraventricular hemorrhage, periventricular leukomalacia) and other systems, and early neonatal mortality. Long-term outcomes in discharged patients were not evaluated in this study.
Statistical analysis
Statistical analysis and graphing were performed using Excel spreadsheets (Microsoft, USA) and the GraphPad Prism 8 software (GraphPad Software, USA). The distribution of continuous variables was tested for normality using the generalized D'Agostino–Pearson test. Quantitative variables showing normal distribution were expressed as means (standard deviation) and compared by t-test. Data with non-normal distribution were reported as a median (interquartile range) and analyzed by the Mann-Whitney test. Qualitative variables were summarized as counts and percentages (n, %) and compared using Fisher's exact test and chisquare (χ2) test. Differences were considered statistically significant at p <0.05. The study was approved by the Research Ethics Committee of the V.I. Kulakov NMRC for OG&P of Minzdrav of Russia.
Results
This study prospectively analyzed 253 patients with monochorionic diamniotic twin pregnancies, including 153 pregnancies complicated by TTTS (study group) and 100 uncomplicated pregnancies (control group).
Stage I, II, III, IV, and V TTTS was detected in 16.3% (25), 49.1% (75), 21.6% (33), 7.8% (12), and 5.2% (8) of pregnant women, respectively.
 The stages of TTTS differed among the study subgroups. Stage II was most common in the subgroup of laser coagulation (49.1%), stage I among patients undergoing amnioreduction, and patients with the natural course of TTTS most commonly had stage IV and V (p <0.01).
The stages of TTTS differed among the study subgroups. Stage II was most common in the subgroup of laser coagulation (49.1%), stage I among patients undergoing amnioreduction, and patients with the natural course of TTTS most commonly had stage IV and V (p <0.01).
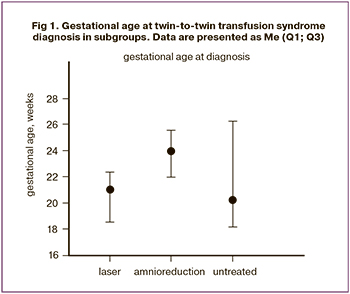
The subgroups also differed significantly regarding the term at TTTS diagnosis. It was the latest in the amnioreduction subgroup (24 weeks), while in the subgroups 1 and 3, the median term at diagnosis was 21 and 20.3 weeks, respectively, p = 0.01 (Fig. 1).
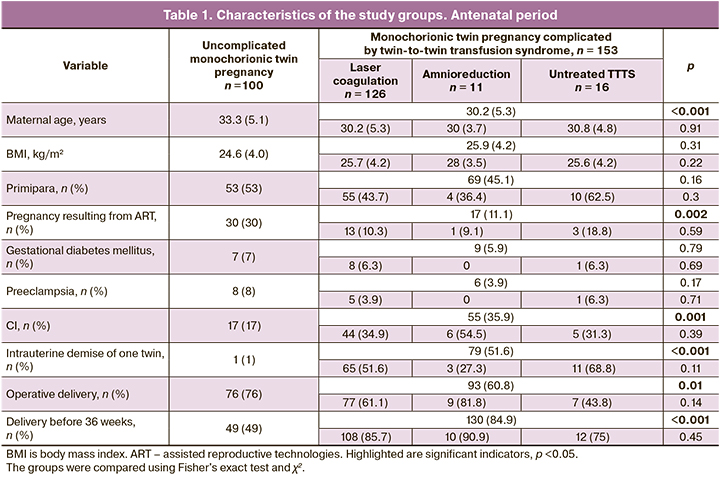
The mean age of pregnant women in the groups differed significantly. Patients with TTTS were younger than patients in the control group [30.2 (5.3) vs. 33.3 (5.1) years], p <0.001. There were no significant differences in age between women in the subgroups.
No differences in body mass index, parity, and somatic comorbidities were identified between women in the subgroups.
In the control group, more pregnancies were resulting from assisted reproductive technologies than in the study group (30% vs. 11.1%, p = 0.002). There were no differences in the subgroups.
The incidence of pregnancy complications such as gestational diabetes mellitus and preeclampsia did not differ in the study and control groups. There were no differences in the subgroups, either.
Patients with TTTS were statistically more likely to have cervical shortening less than 25 mm according to ultrasound data than those with uncomplicated pregnancy (35.9%, vs. 17%, p = 0.001). There was no difference in subgroups. Analysis of the relationship between the severity of polyhydramnios and cervical shortening showed that patients with a short cervix had larger vertical pocket (median MVP 13 cm) than those with normal cervix length (median MVP 11.5 cm) (p = 0.04). At the same time, there was no statistically significant difference in terms of delivery in women of the study group with and without cervical shortening [31.8 (28.3; 34.3vs. 31.7 weeks (26.5; 34.6), respectively], p = 0.64.
The intrauterine death rate of one twin was significantly higher in the study group than in with the control group [51.6% (79) vs. 1% (1), p<0.001, odds ratio 105.7 (95% confidence interval 18.5 - 1076)]. No statistically significant differences were observed between subgroups regarding antenatal death rates.
However, counting all cases of intrauterine death, i.e., the number of non-surviving fetuses to the total number of fetuses in each subgroup, showed that this indicator was higher in the group with untreated TTTS where 17 out of 32 fetuses (53.1%) died in utero. In the subgroups of laser coagulation and amnioreduction, it was 36.5% (92 out of 252) and 22.7% (5 out of 22), respectively, (p = 0.047). Antenatal death of one twin occurred in 28.6% (36 of 126), 9.1% (1 of 11), and 31.3% (5 of 16) of pregnant women in subgroups 1, 2, and 3. Donor and recipient twins died in utero in 61.9% (26 out of 42) and 38.1% (16 out of 42) cases, respectively, p = 0.001. Antenatal death of both twins occurred in 37.5% (6 of 16), 18.2% (2 of 11), and 22.2% (28 of 126) of cases in the subgroup with untreated TTTS, after amnioreduction, and after laser coagulation, respectively.
Overall survival of fetuses with TTTS was 77.8%, 81.8%, and 62.5% in subgroups 1, 2, and 3.
The most common mode of delivery in the study cohort was a cesarean section (66.8%). At the same time, the cesarean delivery rate was significantly higher in the control group (76%) than in the study group (60.8%), p = 0.01. Comparison of the operative delivery rates in subgroups with different approaches to the management of TTTS pregnancy did not reveal a significant difference, p = 0.14.
A total of 179 (70.8%) pregnant women delivered before 36 weeks' gestation. Among women with monochorionic twin pregnancies complicated and not complicated by TTTS, rates of delivery before 36 weeks' gestation were 84.9% (130 of 153) and 49% (49 of 100), respectively, p <0.001. Comparison of rates of delivery before 36 weeks in subgroups showed no significant difference, p = 0.45.
Analysis of the relationship between intrauterine fetal demise and the gestational age at delivery of the surviving co-twin showed that median gestational age at delivery among women with and without this pregnancy complication was 34.7 (31; 38) and 32.3 (29.2; 34.4) weeks, respectively, p = 0.002.
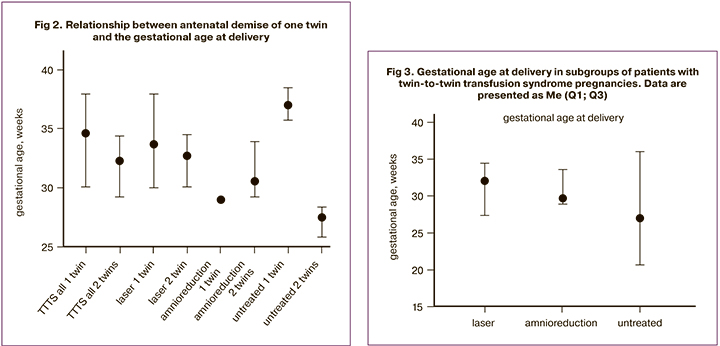
A comparison of the gestational age at delivery in pregnancies with antenatal fetal demise revealed the most significant difference in the subgroup with the natural course of TTTS. The antenatal demise of one co-twin was associated with longer gestation with childbirth occurring on average at 37.1 (1.5) weeks compared with 27.2 (1.4) among women without this complication, p <0.001. Among women who underwent laser coagulation of placental anastomoses, the antenatal demise of one co-twin was also associated with longer gestation [33.7 (4.2) versus 32.3 (2.7) weeks], p = 0.05 (Fig. 2).
The clinical characteristics of pregnant women and the course of the antenatal period in the study groups are presented in Table 1.
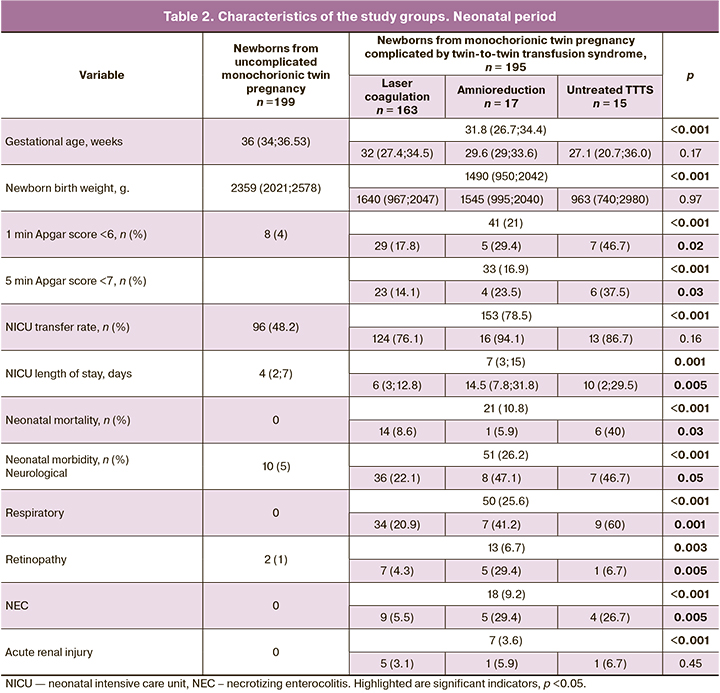
There were significant differences between study groups regarding the gestational age of newborns.
The median gestational age of monochorionic twins complicated and not complicated by TTTS was 31.8 and 36 weeks, respectively (p <0.001). In the subgroup with laser coagulation, amnioreduction, and the natural course of TTTS, this indicator was 32, 29.6, and 27.1 weeks, respectively; no statistically significant differences were found, p = 0.17 (Fig. 3).
The median birth weight of newborns from pregnancies affected by TTTS (study group) was significantly lower (1490 g) than that in controls with uncomplicated pregnancy (2359 g), p <0.001. Comparisons in subgroups reveal no statistically significant differences.
A newborn baby's health was evaluated by the Apgar score at the first and fifth minutes. In each group, the proportions of newborns with Apgar score <6 at the first minute and <7 at the fifth minute were calculated. The percentage of newborns with low Apgar scores was significantly higher among monochorionic twins from TTTS pregnancies than that from uncomplicated pregnancies (first- and fifth-minute Apgar scores 21% and 4% vs. 16.9% and 2%, respectively), p<0.001.
The largest proportion of monochorionic twins from TTTS pregnancies with low Apgar scores was found in the subgroup with the natural course of pregnancy (1-minute and 5-minute Apgar scores 46.7% and 37.5%), compared with subgroups undergoing laser coagulation of placental anastomoses (1-minute and 5-minute Apgar scores 17.8% and 14.1%) and amnioreduction (1-minute and 5-minute Apgar scores 29.4% and 23.5 %), p = 0.03.
Neonatal complication rates were higher in the study group. The neonatal intensive care unit admission rates among newborns from pregnancies affected by TTTS (78.5%) were significantly higher than those from uncomplicated twin pregnancies (48.2%), p<0.001. A comparison of this indicator in subgroups did not reveal statistically significant differences.
The length of stay of newborns in the ICU was longer among newborns from TTTS pregnancies. The median duration of hospital stay for monochorionic twins from pregnancies affected by TTTS was seven days compared with four days for newborns from uncomplicated pregnancies, p = 0.001. The most extended length of stay in the ICU was observed in the subgroups of amnioreduction (median 14.5 days) and the natural course of TTTS pregnancy (10 days). The shortest length of stay in the ICU was among those undergoing laser coagulation of placental anastomoses (6), p = 0.005.
The analysis of neonatal morbidity showed that the rates of neurological complications in newborns from TTTS pregnancies (26.2%) were significantly higher than in the control group (5%), p<0.001. The neurological disorder rates (intraventricular hemorrhage, periventricular leukomalacia) were considerably higher in the subgroups of amnioreduction (47.1% ), and natural course of TTTS pregnancy (46.7%) than in the subgroup with a patient undergoing laser coagulation was performed (22.1%), p = 0.05.
Respiratory disorders in newborns were detected only in the study group (25.6%). In the subgroups of amnioreduction, the natural course of TTTS pregnancy, and laser coagulation, respiratory disorder rates were 41.2%, 60%, and 20.9%, respectively, p = 0.001.
Newborns in the study group were significantly more likely (6.7%) to have retinopathy than in the control group (1%), p = 0.003. In subgroups, the highest retinopathy rate was observed in the amnioreduction group (29.4%), p = 0.005.
Major neonatal morbidities, including necrotizing enterocolitis (NEC) and acute renal injury, were observed only in the study group. Rates of NEC in subgroups of amnioreduction, untreated TTTS, and laser coagulation were 29.4%, 26.7%, and 5.5%, respectively, p = 0.005. There were no statistically significant differences in the rates of acute renal injury between the subgroups.
Neonatal deaths were observed only among newborns from TTTS pregnancies (n=21; 10.8%). Most neonatal deaths occurred in the subgroup with untreated TTTS (40%); in subgroups I and II, it was 8.6% and 5.9%, respectively, p = 0.03.
Analysis of neonatal mortality included rates of neonatal deaths depending on gestational age at delivery, birth weight, stage of TTTS, and the status of the non-surviving co-twin (donor or recipient). Neonatal mortality was significantly associated with gestational age at delivery. Non-surviving twins were born at 26.6 (24.8; 28.7) weeks, while the median gestational age at delivery of pregnancies affected by TTTS was 31.8 (26.7; 34.4) weeks, p = 0.001.
The median birth weight of non-surviving twins was statistically different from the birth weight of newborns from TTTS pregnancies [740 (590; 985) vs. 1490 (950; 2042) grams, respectively], p<0.001. The stages of TTTS also varied: non-surviving twins mostly had stage III, while survivors had stage II. Among the 21 non-surviving twins, 12 were donors, and 9 were recipients, p = 0.54.
Clinical characteristics of newborns and neonatal period of the study groups are presented in Table 2.
Discussion
Twin-to-twin transfusion syndrome is known as a severe twin pregnancy complication. If left untreated, TTTS can be life-threatening for both babies or lead to neurological and respiratory disorders in newborn twins [7, 8]. In our study, intrauterine fetal demise secondary to TTTS was 51.6% and 1% in the control group of normal twin pregnancy. Neurological morbidity in newborns from TTTS pregnancies and the control group was 26.2% and 5%, respectively.
TTTS is one of the significant determinants of perinatal loss in monochorionic multiple pregnancies. The implementation of laser coagulation of placental vascular anastomoses into clinical practice has significantly changed the natural course of this disease [9]. The use of fetoscopy in recent years, according to Diehl W. et al., was associated with an increase in perinatal survival of one or both TTTS twins from 50% to 89.5% [10]. In our study, the overall fetal survival rate of twins undergoing laser coagulation of placental vascular anastomoses was 77.8%. These results provide evidence that laser coagulation of placental vascular anastomoses is effective in the treatment of TTTS.
Of note is the study by Lenclen R. et al. comparing amnioreduction and laser coagulation. The study reported that perinatal mortality was significantly higher in the amnioreduction than in the fetoscopic laser coagulation group (RR, 3.4; 95% CI, 1.4–8.3; p=0.01) and the proportion of extremely preterm babies was also significantly higher in the amnioreduction group (66.6% versus 42.5%; p 0.02) [11].
The antenatal mortality rate of one twin was 36.5% and 22.7% among those undergoing laser coagulation of placenta vascular anastomoses and amnioreduction, respectively. The lower antenatal mortality rate in the amnioreduction subgroup was associated with earlier delivery, high neonatal morbidity, and longer stay of newborns in the ICU.
According to some authors, the implementation of amnioreduction correlates with earlier gestational age at delivery, low Apgar scores, high perinatal and neonatal mortality, and neurological morbidity [7, 11]. Also, many authors reported that babies born to patients undergoing fetoscopic laser coagulation had significantly higher rates of anemia and polycythemia on the 1st day of life. Therefore, amnioreduction is warranted in stage I TTTS and cases of its late-onset. TTTS is known to progress, i.e. transit from stage I to higher stages, only in 60% of cases [12]. Accordingly, sometimes it suffices to perform 1 or 2 amnioreduction procedures to prolong pregnancy and prolong gestational age. In the case of further progression of TTTS, early amnioreduction may affect the effectiveness of laser coagulation due to impaired visualization of placental anastomoses [12].
Amnioreduction is not the treatment of choice for stage II–IV TTTS, as laser coagulation has been associated with higher perinatal survival. In a Cochrane review, D. Roberts et al. (2008) showed that fetus survival rate in pregnancies treated by amnioreduction was 50%, regardless of the TTTS stage and gestational age at the disease onset [7]. The authors suggest that amnioreduction can be retained as a treatment option for those situations in which the expertise for laser coagulation is not available or pending transfer to a unit where such treatment can be obtained in patients with severe polyhydramnios or cervical length shortening to less than 25 mm on ultrasound.
Naturally, the birth weight of the newborns in the study group was significantly lower than that among controls, which is due to the earlier gestational age at delivery. Prematurity and TTTS related morbidity of newborns contributed to low Apgar scores and longer length of stay in the ICU.
R. Lenclen et al. (2007) reported that neonates treated by amnioreduction had a high rate of severe brain damage (37.9% versus 16.2%; p=0.003), such as grade 3 intraventricular hemorrhage and periventricular leukomalacia [13]. Regarding the damage to other organ systems, the authors noted high rates of respiratory distress syndrome (88.6%), renal failure (20.0%), and necrotizing enterocolitis (17.9%).
In the present study, perinatal morbidity was higher in the study group due to high rates of retinopathy, neurological, and respiratory disorders in subgroups II and III. Necrotizing enterocolitis and acute kidney injury were observed only in infants from subgroups II and III. This observation confirms the need for treatment when the diagnosis of TTTS is established, the high morbidity of twins without antenatal treatment, and the insufficient effectiveness of amnioreduction in stages II–IV TTTS.
The study findings confirm that laser coagulation of placental vascular anastomoses is the most effective treatment for stage II–IV TTTS with the best rates of perinatal morbidity and mortality.
The present study demonstrates the role of TTTS in the development of perinatal complications of monochorionic multiple pregnancies, which require more careful attention since this pregnancy is accompanied by a high risk of intrauterine fetal death, neonatal morbidity, and mortality.
The strong point of the study is a sufficient sample of 253 pregnant women and 394 newborns. Maternal care during pregnancy, delivery, and neonatal care was provided at the departments of the V.I. Kulakov NMRC for OG&P of Minzdrav of Russia.
The main limitation of the study is the lack of data on long-term outcomes for pregnancies undergoing TTTS. Further studies in this direction are needed to better inform future parents.
The study findings suggest the need to identify the predictors of monochorionic multiple pregnancy complications to optimize patient management strategy, ensure timely surgical correction and safe pregnancy prolongation, and reduce neonatal morbidity and mortality.
Conclusion
Monochorionic multiple pregnancies complicated by TTTS carry a higher risk of perinatal complications compared with uncomplicated monochorionic twins. Conservative management of TTTS pregnancy and serial amnioreductions are associated with unfavorable outcomes, including the intrauterine demise of one or both twins, early neonatal mortality, and neurological and respiratory morbidity. Laser coagulation of placental vascular anastomoses improves perinatal outcomes in monochorionic multiple pregnancies complicated by TTTS.
References
- Mosquera C., Mille R.S., Simpson L.L. Twin-twin transfusion syndrome. Semin. Perinatol. 2012; 36(3): 182-9. https://dx.doi.org/10.1053/j.semperi.2012.02.006.
- Lewi L., Deprest J., Hecher K. The vascular anastomoses in monochorionic twin pregnancies and their clinical consequences. Am. J. Obstet. Gynecol. 2013; 208(1): 19-30. https://dx.doi.org/10.1016/j.ajog.2012.09.025.
- Бугеренко А.Е., Суханова Д.И., Донченко Я.С., Панина О.Б., Сичинава Л.Г. Ангиоархитектоника плаценты при синдроме фето-фетальной трансфузии у беременных с монохориальной двойней. Перинатальные исходы. Акушерство и гинекология. 2019; 5: 63-9. https://dx.doi.org/10.18565/aig.2019.5.63-69. [Bugerenko A.E., Sukhanova D.I., Donchenko Y.S., Panina O.B., Sichinava L.G. Angioarchitectonics of the monochorionic placenta in twin-to-twin transfusion syndrome. Perinatal outcomes. Obstet. Gynecol. 2019 (5): 63-9. (in Russian)]. https://dx.doi.org/10.18565/aig.2019.5.63-69.
- Sakalo V.A., Kostyukov K.V., Gladkova K.A., Gasanova R.M., Tetruashvili N.K., Bockeria E.L. Fetal cardiovascular hemodynamics in twin-to-twin transfusion syndrome. Child. Heart Vasc. Dis. 2018; 15(3): 137-43. https://dx.doi.org/10.24022/1810-0686-2018-15-3-137-143.
- Simpson L.L.; Society for Maternal-Fetal Medicine. Twin transfusion syndrome. Am. J. Obstet. Gynecol. 2013; 208(1): 3-18. https://dx.doi.org/10.1016/j.ajog.2012.10.880.
- Quintero R.A., Dickinson J.E., Morales W.J., Bornick P.W., Bermúdez C., Cincotta R. et al. Stage-based treatment of twin-twin transfusion syndrome. Am. J. Obstet. Gynecol. 2003; 188(5): 1333-40. https://dx.doi.org/10.1067/mob.2003.292.
- Roberts D., Gates S., Kilby M., Neilson J.P. Interventions for twin-twin transfusion syndrome: a Cochrane review. Ultrasound Obstet. Gynecol. 2008; 31(6): 701-11. https://dx.doi.org/10.1002/uog.5328.
- Gheorghe C.P., Boring N., Mann L., Donepudi R., Lopez S.M., Chauhan S.P. et al. Neonatal Outcomes and maternal characteristics in monochorionic diamniotic Twin pregnancies: uncomplicated versus twin-to-twin transfusion syndrome survivors after fetoscopic laser surgery. Fetal Diagn. Ther. 2020; 47(2): 165-70. https://dx.doi.org/10.1159/000500858.
- De Lia J.E., Cruikshank D.P., Keye W.R. Fetoscopic neodymium: YAG laser occlusion of placental vessels in severe twin‐twin transfusion syndrome. Obstet. Gynecol. 1990; 75(6): 1046-53.
- Diehl W., Diemert A., Grasso D., Sehner S., Wegscheider K., Hecher K. Fetoscopic laser coagulation in 1020 pregnancies with twin-twin transfusion syndrome demonstrates improvement in double-twin survival rate. Ultrasound Obstet. Gynecol. 2017; 50(6): 728-35. https://dx.doi.org/10.1002/uog.17520.
- Lenclen R., Ciarlo G., Paupe A., Bussieres L., Ville Y. Neurodevelopmental outcome at 2 years in children born preterm treated by amnioreduction or fetoscopic laser surgery for twin-to-twin transfusion syndrome: comparison with dichorionic twins. Am. J. Obstet. Gynecol. 2009; 201(3): 291. e1-5. https://dx.doi.org/10.1016/j.ajog.2009.05.036.
- Emery S.P., Hasley S.K., Catov J.M., Miller R.S., Moon-Grady A.J., Baschat A.A. et al. North American Fetal Therapy Network: Intervention vs expectant management for stage I twin-twin transfusion syndrome. Am. J. Obstet. Gynecol. 2016; 215(3): 346. e1-7.
- Lenclen R., Paupe A., Ciarlo G., Couderc S., Castela F., Örtqvist L., Ville Y. Neonatal outcome in preterm monochorionic twins with twin-to-twin transfusion syndrome after intrauterine treatment with amnioreduction or fetoscopic laser surgery: comparison with dichorionic twins. Am. J. Obstet. Gynecol. 2007; 196(5): 450. e1-450. e7. https://dx.doi.org/10.1016/j.ajog.2007.01.036.
Received 18.05.2020
Accepted 11.06.2020
About the Authors
Kirill V. Kostyukov, M.D., Ph.D., Senior Researcher at the Department of Fetal Medicine, Institute of Obstetrics; Physician at the Unit of Functional and Ultrasound Diagnostics, Department of Diagnostic Imaging, V.I. Kulakov NMRC for OG&P of Minzdrav of Russia. Tel.: +7(926)214-97-84. E-mail: kostyukov_k@yahoo.com.4, Ac. Oparina str., Moscow, 117997, Russian Federation.
Victoria A. Sakalo, Physician at the 1st Obstetric Department of Pathology of Pregnancy, V.I. Kulakov NMRC for OG&P of Minzdrav of Russia.
Tel.: +7(929)588-72-08. E-mail: v_sakalo@oparina4.ru.
4, Ac. Oparina str., Moscow, 117997, Russian Federation.
Kristina A. Gladkova, Ph.D., Senior Researcher at the Department of Fetal Medicine, Institute of Obstetrics; Head of the 1st Obstetric Department of Pathology of Pregnancy, V.I. Kulakov NMRC for OG&P of Minzdrav of Russia. Tel.: +7(916)321-10-07. E-mail: k_gladkova@oparina4.ru.
4, Ac. Oparina str., 117997, Moscow, Russian Federation.
Oleg V. Ionov, Ph.D., Head of the A.G. Antonov Neonatal Intensive Care Unit, Institute of Neonatology and Pediatrics, V.I. Kulakov NMRC for OG&P of Minzdrav of Russia; Associate Professor at the Department of Neonatology, Faculty of Pediatrics of I.M. Sechenov First MSMU. E-mail: o_ionov@oparina4.ru.
4, Ac. Oparina str., Moscow, 117997, Russian Federation.
Marika N Shakaya, Ph.D., Teaching Assistant at the Department of Neonatology, N.F. Filatov Clinical Institute of Children’s Health, I.M. Sechenov First MSMU of Minzdrav of Russia (Sechenov University); Emergency Neonatologist at the A.G. Antonov Neonatal Intensive Care Unit, Institute of Neonatology and Pediatrics, V.I. Kulakov NMRC for OG&P of Minzdrav of Russia; Tel.: +7(903)769-61-60. E-mail: m_shakaya@oparina4.ru. 4, Ac. Oparina str., Moscow, 117997, Russian Federation.
Nana K. Tetruashvili, Dr.Med.Sci., Deputy Director, Institute of Obstetrics; Head of the 2nd Obstetrics Department of Pathology of Pregnancy, V.I. Kulakov
NMRC for OG&P of Minzdrav of Russia.. Tel.: +7(495)438-14-77. Е-mail: tetrauly@mail.ru. 4, Ac. Oparina str., Moscow, 117997, Russian Federation.
For citation: Kostyukov K.V., Sakalo V.A., Gladkova K.A., Shakaya M.N., Ionov O.V., Tetruashvili N.K. Perinatal outcomes of monochorionic multiple pregnancies complicated by twin-to-twin transfusion syndrome.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2020; 8: 72-80 (in Russian)
https://dx.doi.org/10.18565/aig.2020.8.72-80