The effect of surgeon experience on outcomes of fetoscopic laser coagulation of placental anastomoses in twin-to-twin transfusion syndrome
Relevance. Fetoscopic laser coagulation (FLC) of placental anastomoses is the only pathogenetically oriented treatment of twin-to-twin transfusion syndrome (TTTS). Aim. To investigate the effect of the learning curve for TTTS on treatment outcomes and the incidence of postoperative complications. Material and methods. This retrospective study included 126 patients with monochorionic diamniotic twins who underwent fetoscopic laser coagulation of placental anastomoses for TTTS at the V.I. Kulakov NMRC for OG&P in 2014–2019. The patients were divided into three equal groups of 42 women each. Groups 1, 2, and 3 included pregnant women who underwent FLC in 2014–2016, 2017–2018, and 2018–2019, respectively. The study investigated the effect of the learning curve on fetal survival and complication rates. Statistical analysis was performed using the D’Agostino-Pearson test, the Mann-Whitney U-test, and the Kruskal-Wallis test. Differences were considered statistically significant at p <0.05. Results. Increasing surgeon caseload for FLC was associated with higher overall (from 61.9% to 88.1%) and both twins’ survival rates (from 38.1% to 59.5%). Postoperative complication rates reduced from 64.3% to 52.4%. The incidence of neonatal morbidity and mortality decreased along with an increasing number of FLCs performed. We achieved satisfactory FLC results for overall survival (at least 73%) after performing 34 procedures, and 80 procedures for the survival of both twins (at least 55%). Conclusion. The accumulation of experience and concentration of fetal surgery at a high-volume provider contributes to better overall and both twins’ survival with a concomitant reduction in the incidence of postoperative complications. FLC and other in utero surgical procedures should be concentrated at highly specialized high-volume centers with high patients’ flow.Gladkova K.A., Kostyukov K.V.
Keywords
Twin-to-twin transfusion syndrome complicates 9–15% of monochorionic multiple pregnancies [1]. The most effective in utero treatment of TTTS is fetoscopy-guided laser coagulation of placental anastomotic vessels. Fetoscopic laser coagulation (FLC) is the only pathogenetically oriented treatment with the best fetal survival rates and neurologic outcomes in newborns, as proven by a randomized controlled trial [2]. At the same time, many researchers reported that outcomes of FLC depend on a surgeon's skills and experience in performing these interventions [3, 4]. There is no doubt that the implementation of FLC requires training of the surgical team. The acquisition of new surgical skills can be reflected using a learning curve, which is a graphical representation showing the change in a learner's performance in a particular knowledge or skill. This study aimed to determine the learning curve for fetoscopic laser coagulation of placental anastomoses in twin-to-twin transfusion syndrome during its implementation in V.I. Kulakov NMRC for OG&P.
Material and methods
This retrospective study included 126 patients with monochorionic diamniotic twins who underwent fetoscopic laser coagulation of placental anastomoses for TTTS at the V.I. Kulakov NMRC for OG&P in 2014–2019.
The inclusion criterion was a monochorionic diamniotic twin pregnancy complicated by TTTS, which was managed by FLC, followed by postoperative observation and delivery at the V.I. Kulakov NMRC for OG&P.
Exclusion criteria were monochorionic monoamniotic twin pregnancy, dichorionic diamniotic twin pregnancy, higher-ordermultiplepregnancies(triplets, quadruplets), unknown chorionicity, genetic abnormalities in one or both fetuses.
The gestational age was calculated based on the first day of the woman's last menstrual period or the CPD of the larger fetus measured at 10–14 weeks of gestation.
The type of chorionicity and amnionicity in multiple pregnancies was determined by ultrasonography up to 14 weeks of gestation. Monochorionic diamniotic twin pregnancy was identified by the presence of a single gestational sac containing two live fetuses and two amnions (a T-sign).
Diagnosis of fetal-fetal transfusion syndrome was based on the presence of oligohydramnios (defined as a maximal vertical pocket of <2 cm) in one sac, and of polyhydramnios (a maximal vertical pocket of >8 cm) in the other sac. The severity of TTTS was assessed according to the Quintero staging system [5].
All FLCs were performed by one team of surgeons using a standard protocol. Fetoscopic laser coagulation of placental anastomotic vessels was performed by transabdominal access under local anesthesia. Prophylactic antibiotics (II–III generation cephalosporins) and tocolytics (the choice was made on a case-by-case basis) were administered. A 2.3–3.3 mm fetoscopic trocar was inserted under continuous ultrasound guidance into the in the recipient amniotic cavity. Then a fetoscope with a laser energy conductor was inserted, and anastomoses were coagulated without contact with the tissue. The operation was completed by amnioreduction until the normal amount of amniotic fluid (MVP 4–6 cm).
All 126 patients were divided into three equal groups of 42 women each. Groups 1, 2, and 3 included pregnant women who underwent FLC in 2014–2016, 2017–2018, and 2018–2019, respectively. The groups were compared by indicators of the antenatal period, such as overall survival, the survival of both twins, the rates of preterm birth, and postoperative complications. Neonatal indicators included the gestational age of newborns, their birth weight, morbidity, and mortality. The learning curve was assessed according to three criteria: overall and both twins' survival rates, and the incidence of postoperative complications.
Statistical analysis
Statistical analysis and graphing were performed using Excel spreadsheets (Microsoft, USA) and the GraphPad Prism 8 software (GraphPad Software, USA). The distribution of continuous variables was tested for normality using the generalized D'Agostino-Pearson test. Quantitative variables showing normal distribution were expressed as means (standard deviation) and compared by t-test. Data with non-normal distribution were reported as a median (interquartile range) and analyzed by the Mann-Whitney test. Qualitative variables were summarized as counts and percentages (n, %) and compared using Fisher's exact test. To determine the number of operations required to achieve the target, the function was approximated using a trend line with values varying between 0 and 1. Differences were considered statistically significant at p <0.05. The study was approved by the Research Ethics Committee of the V.I. Kulakov NMRC for OG&P of Minzdrav of Russia.
 Results
Results
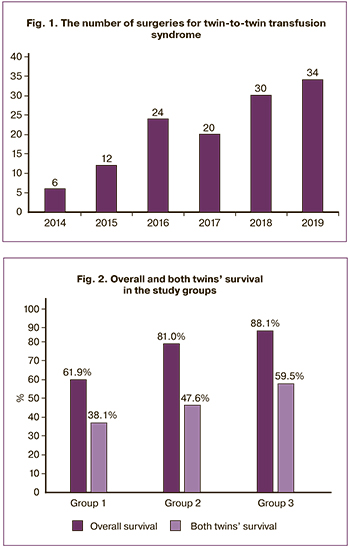
In 2014–2019, 188 fetoscopic laser coagulations of placental anastomoses for TTTS were performed at the V.I. Kulakov NMRC for OG&P of Minzdrav of Russia. The study included 126 women who were observed postoperatively and delivered their babies at the Center. The number of surgical interventions for TTTS increased from year to year (Fig. 1).
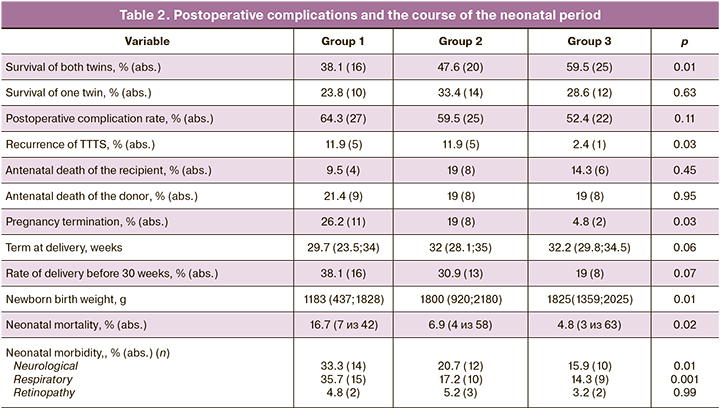
No significant differences between study groups were observed concerning operating time for FLC (p = 0.58) and TTTS stages (p = 0.78). The most common was TTTS with stages II and III. There were no significant differences between study groups regarding the posterior and anterior location of the placenta (p = 0.27). The characteristics of the studн groups are presented in Table 1.
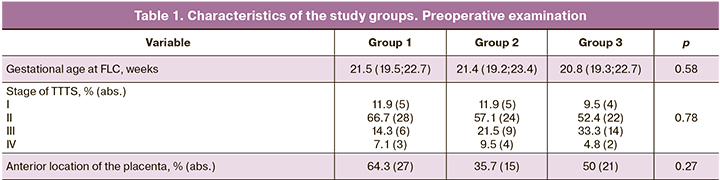
The rates of overall and both twins' survival were assessed in the study groups (Fig. 2).
Increasing surgeon caseload was associated with higher overall and both twin survival rates. Overall survival in groups 1, 2, and 3 was 61.9%, 81%, and 88.1%, respectively (p <0.001). The both twins’ survival rates in groups 1, 2, and 3 was 38.1%, 47.6%, and 59.5%, respectively (p = 0.01).
Postoperative complication rates in groups 1 and 3 reduced by 64.3% and 52.4%, respectively, but the differences were not statistically significant (p = 0.11). A more detailed analysis was conducted of complications that may be associated w the experience in performing FLC, such as TTTS recurrence, termination of pregnancy, antenatal death of the donor and recipient. There was a statistically significant decrease in the incidence of TTTS recurrence both in group 2 (by 11.9%) and 3 (by 2.4%), p = 0.03. Pregnancy termination rates in the postoperative period also were higher in group 1 (26.2%), and was lowest in group 3 (4.8%), p = 0.03.
The terms at delivery did not differ significantly between the groups 1, 2, and 3 (29.7, 32, and 32.2 weeks, respectively), p = 0.06. Also, there were no statistically significant differences in the rates of childbirth before 30 weeks, even though it was found to decrease from 38.1% in group 1 to 19% in group 3 (p = 0.07). Antenatal death rates of the donor and recipient did not differ significantly between the groups.
There was a statistically significant difference in the newborns' birth weight, which was the lowest in group 1 (1183g) compared with groups 2 and 3 (1800 and 1825g, respectively), p = 0.01.
Neonatal mortality rate decreased, being 16.7%, 6.9%, and 4.8% in group 1, 2, and 3, respectively (p = 0.020).
Neonatal morbidity, primarily neurological and respiratory, also decreased from the first to the third group. Neurological and respiratory disorder rates were highest in group 1 (33.3% and 35.7%, respectively) and lowest in group 3 (15.9% and 14.3%, respectively), (p = 0.01 and 0.001).
The characteristics of the course of the postoperative and neonatal periods in the study groups are presented in Table 2.
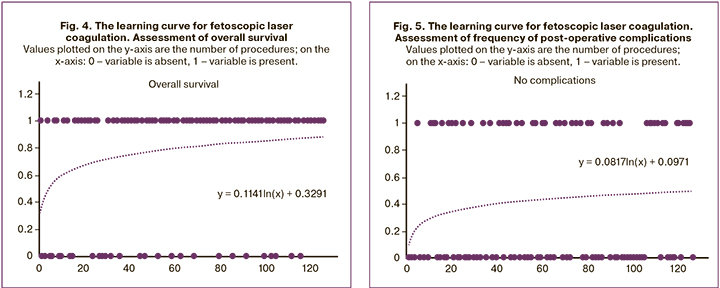
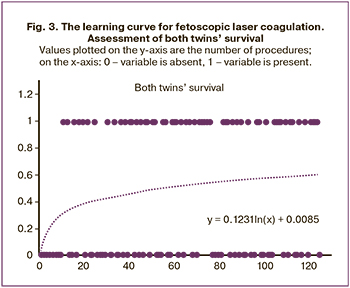 The FLC training charts were constructed based on the determination of the overall and both twins’ survival and postoperative complication rates. There was an association between the shapes of the curves and the increasing number of operations. Initially, the parabolic shape is transformed into an almost horizontal line, along with gaining experience and skills (Fig. 3–5).
The FLC training charts were constructed based on the determination of the overall and both twins’ survival and postoperative complication rates. There was an association between the shapes of the curves and the increasing number of operations. Initially, the parabolic shape is transformed into an almost horizontal line, along with gaining experience and skills (Fig. 3–5).
The study findings demonstrated that accumulation of experience was associated with an increase in overall and both twins’ survival.
The study findings indicated that accumulation of experience was associated with a decrease in the number of postoperative complications.
Discussion
Twin-to-twintransfusionsyndromeisoneoftheleading causes of adverse perinatal outcomes of monochorionic multiple pregnancies. The implementation of in utero treatment of TTTS into clinical practice has significantly changed the natural course of this disease. Fetoscopic laser coagulation of vascular anastomoses on the placenta, eliminating the immediate cause of TTTS, is the optimal treatment of this pregnancy complication. The operation is minimally invasive and is performed from 16 to 26 weeks of pregnancy [6, 7]. In the present study, FLC was conducted from 16 to 27.6 weeks, with an average of 21.4±2.5 weeks.
Recently, there has been growing interest in the modification of coagulation referred to as the «Solomon technique», which involves coagulation of the vascular equator of the chorionic surface after selective FLC. This technique is aimed at increasing fetal survival, reducing the rates of TTTS recurrence and APS, which occurs in 13% of cases after selective coagulation [8]. Extensive studies have reported overall fetal survival after fetoscopic laser coagulation of placental vascular anastomoses in patients with TTTS, ranging from 73 to 90.5%, and both twins’ survival from 55 to 82.5% [9].
According to Chmait et al., who analyzed the outcomes of 682 FLCs, both twins’ survival and overall survival rates were 67% and 91%, respectively [10]. There are published data demonstrating a wide variety of FLC outcomes in TTTS. It is believed that gaining experience of a surgical team has a positive effect on overall and both twins’ survival rates. In this connection, the study of the effect of the learning curve for performing fetoscopic laser coagulation of placental anastomoses in TTTS is exceptionally relevant. A meta-analysis by Ahmed et al. of studies published between 1995 and 2009 did not find a significant effect of surgeon experience and the improvement of surgical technique on single twin survival [11]. However, they did not analyze the survival rate of both twins, which is the main goal of in utero TTTS correction. In contrast, Morris et al. reported a significant improvement in perinatal one twin survival with increased experience of the surgeon [3]. However, they also did not assess the effect of the experience on the survival of both twins. According to Diehl W. et al., who analyzed 600 cases of laser coagulation of placental anastomoses from 1995 to 2007, the survival rate of both twins increased from 50% in the first 200 patients to 69.5% in the last 200. The overall survival rate increased from 65% to 79.5% (p <0.001) [4]. In our study, the overall survival after FLC was 77.8%; the survival rate of both twins was 49.2%. There was also an increase in the overall survival rate with an increase in the number of surgical interventions from 61.9% in group 1 (2014–2016) to 88.1% in group 3 (2018–19), p <0.001. Similar data were obtained for both twins’ survival rates. The acquisition of experience in FLC resulted in an increase in the survival rate from 38.1% in group 1 to 59.5% in group 3, p = 0.01. According to a systematic review of 25-year FLC data by Akkermans et al., both twins’ survival rates significantly increased from 31% to 62%, reflecting the learning curve effect [12].
The outcome of TTTS may depend on other factors, such as the stage of the syndrome. According to Chmait et al., who analyzed the relationship between survival and stages of TTTS, there were no significant differences in both twins’ survival of two fetuses in stage I and II TTTS. Still, they found a significant decrease in the donor survival rate in stage III TTTS [10].
In our study, there was no significant difference in TTTS stages between groups. However, there was a slight increase in the rate of stage III TTTS in group 3. This may be due to later admission since a large number of patients were referred from remote regions of Russia. Training in new surgical interventions can be carried out using the observation by an experienced surgeon or through hands-on training with the assistance of a surgeon who has perfectly mastered the technique. According to Papanna et al., an observer trained operator must perform at least 60 FLCs on his own to reach an acceptable performance rate. A hands-on trained operator assisted by an experienced surgeon needs to complete about 20 procedures to achieve an adequate level of competence [13].
Another study showed similar results suggesting that 25-35 procedures need to be performed to acquire the skills necessary for FLC [14]. The advantages of hands-on training with an experienced surgeon include a consistent increase in the level of operation complexity (start with technically more straightforward procedures when the placenta is located on the posterior wall), the possibility of immediate intervention by an experienced surgeon in case of technical difficulties and for a final check whether all anastomoses were coagulated. In our Center, the training of the surgical team performing FLC was based on observation of an entire procedure done by experienced colleagues during internships in clinics in the USA and Great Britain. We achieved satisfactory FLC results for overall survival (at least 73%) after performing 34 procedures, and 80 procedures for the survival of both twins (at least 55%), which was consistent with the above data [3, 9].
Our study supports the notion that fetoscopic laser coagulation of placental anastomoses in TTTS and other in utero surgical interventions should be centralized at high-volume providers and large national specialized centers. This is because mastering FLC skills and accumulating surgical experience requires an annual caseload of at least 20–30 FLCs. Only under this condition the acquired skills will be improved and maintained at the proper level. This approach is supported by a study by van Klink et al., reporting a reduction in the incidence of neurodevelopmental impairment from 18% to 6% and an increase in twin survival, which was attributed to the improvement of pregnancy management, the effect of the learning curve and the development of new treatments [15].
One of the limitations of this study is that we were not able to investigate the effect of FLC modalities, such as sequential selective laser coagulation and Solomon's technique. We started using Solomon's technique in 2016; therefore, it was used only in patients of groups 2 and 3. The results of a multicenter randomized clinical trial comparing Solomon's technique with selective coagulation of anastomoses showed a decrease in the APS rate and TTTS recurrence rate in Solomon's technique group compared with the standard FLC group (4% versus 21%). Still, there were no differences in antenatal mortality and severe neonatal morbidity, as well as survival without neurodevelopmental impairment in children under two years of age (67% versus 68%) [16].
The experience of creating learning curves for new interventions in pediatric and adult surgery is common. Until now, no attempts have been made in the Russian Federation to generate learning curves in fetal medicine. Our work summarizes the experience gained during the implementation of fetoscopic laser coagulation of placental anastomoses into the management of TTTS in the National Center. Our 6-year experience in surgical correction of TTTS demonstrates an increase in overall and both twins’ survival with a concomitant reduction in the incidence of postoperative complications. Several factors may have contributed to this, such as the accumulation of experience (learning curve effect), improvements in surgical techniques, and ultrasound monitoring. Our data provide strong arguments in favor of concentrating fetal surgery at high-volume providers in the hands of an experienced team of surgeons trained in international fetal medicine clinics.
Conclusion
Improving the outcomes of surgical treatment of TTTS is undoubtedly the result of the training of the surgical team and optimization of surgical techniques, which is possible only at highly specialized high-volume and high-tech centers with high patients’ flow.
References
- Костюков К.В., Гладкова К.А. Диагностика фето-фетального трансфузионного синдрома, синдрома анемии-полицитемии при монохориальной многоплодной беременности. Акушерство и гинекология. 2016; 1: 10-5. [Kostyukov K.V., Gladkova K.A. Diagnosis of twin-twin transfusion syndrome, anemia-polycythemia sequence in monochorionic diamniotic twins. Obstetrics and gynecology. 2016; 1: 10-5. (in Russian)]. https://dx.doi.org/10.18565/aig.2016.1.10-15.
- Roberts D., Neilson J.P., Weindling A.M. Interventions for twin–twin transfusion syndrome: a Cochrane review. Ultrasound Obstet. Gynecol. 2008; 31(6): 701-11. https://dx.doi.org/10.1002/uog.5328.
- Morris R.K., Selman T.J., Harbidge A., Martin W.L., Kilby M.D. Fetoscopic laser coagulation for severe twin-to-twin transfusion syndrome: factors influencing perinatal outcome, learning curve of the procedure and lessons for new centres. BJOG. 2010; 117(11): 1350-7. https://dx.doi.org/10.1111/j.1471-0528.2010.02680.x.
- Diehl W., Diemert A., Glosemeyer P., Wegscheider K. OP06.02: Development of survival rates after intrauterine therapy for severe mid-trimester twin-twin transfusion syndrome: experience with 600 cases. Ultrasound Obstet. Gynecol. 2012; 36(Suppl. 1): 67.
- Quintero R.A., Morales W.J., Allen M.H., Bornick P.W., Johnson P.K., Kruger M. Staging of twin-twin transfusion syndrome. J Perinatol. 1999; 19(8, Pt1): 550-5. https://dx.doi.org/10.1038/sj.jp.7200292.
- Rossi A.C., D’Addario V. Laser therapy and serial amnioreduction as treatment for twin-twin transfusion syndrome: a metaanalysis and review of literature. Am. J. Obstet. Gynecol. 2008; 198(2): 147-52. https://dx.doi.org/10.1016/j.ajog.2007.09.043.
- Бугеренко А.Е., Курцер М.А., Сичинава Л.Г., Суханова Д.И. Синдром фето-фетальной трансфузии. Фетоскопическая лазерная коагуляция анастомозов. Акушерство и гинекология. 2013; 10: 40-5. [Bugerenko A.E., Kurtser M.A., Sichinava L.G., Sukhanova D.I. Twin-twin transfusion syndrome. Fetoscopic laser coagulation of anastomoses. Obstetrics and gynecology. 2013; 10: 40-5. (in Russian)].
- Ruano R., Rodo C., Peiro J.L., Shamshirsaz A.A., Haeri S., Nomura M.L. et al. Fetoscopic laser ablation of the placental anastomoses in twin-twin transfusion syndrome using the ‘Solomon technique’. Ultrasound Obstet. Gynecol. 2013; 42(4): 434-9. https://dx.doi.org/10.1002/uog.12492.
- Yamamoto M., El Murr L., Robyr R., Leleu F., Takahashi Y., Ville Y. Incidence and impact of perioperative complications in 175 fetoscopy-guided laser coagulation of chorionic plate anastomoses in Feto-Fetal Transfusion Syndrome before 26 weeks of gestation. Am. J. Obstet. Gynecol. 2005; 193(3, Pt 2): 1110-6. https://dx.doi.org/10.1016/j.ajog.2005.07.003.
- Chmait R.H., Kontopoulos E.V., Korst L.M., Llanes A., Petisco I., Quintero R.A. Stage-based outcomes of 682 consecutive cases of twin–twin transfusion syndrome treated with laser surgery: the USFetus experience. Am. J. Obstet. Gynecol. 2011; 204(5): 393. e1-6. https://dx.doi.org/10.1016/j.ajog.2011.02.001.
- Ahmed S., Luks F.I., O’Brien B.M., Muratore C.S., Carr S.R. Influence of experience, case load, and stage distribution on outcome of endoscopic laser surgery for TTTS – a review. Prenat. Diagn. 2010; 30(4): 314-9. https://dx.doi.org/10.1002/pd.2454.
- Akkermans J., Peeters S.H.P., Klumper F.J., Lopriore E., Middeldorp J.M., Oepkes D. Twenty-five years of fetoscopic laser coagulation in twin-twin transfusion syndrome: a systematic review. Fetal Diagn. Ther. 2015; 38(4): 241-53. https://dx.doi.org/10.1159/000437053.
- Papanna R., Biau D.J., Mann L.K., Johnson A., Moise K.J.Jr. Use of the Learning Curve – Cumulative Summation test for quantitative and individualized assessment of competency of a surgical procedure in obstetrics and gynecology: fetoscopic laser ablation as a model. Am. J. Obstet. Gynecol. 2011; 204(3): 218. e1-9. https://dx.doi.org/10.1016/j.ajog.2010.10.910.
- Peeters S.H.P., Van Zwet E.W., Oepkes D., Lopriore E., Klumper F.J., Middeldorp J.M. Learning curve for fetoscopic laser surgery using cumulative sum analysis. Acta Obstet. Gynecol. Scand 2014; 93(7): 705-11. https://dx.doi.org/10.1111/aogs.12402.
- van Klink J.M., Koopman H.M., van Zwet E.W., Middeldorp J.M., Walther F.J., Oepkes D., Lopriore E. Improvement in neurodevelopmental outcome in survivors of twin – twin transfusion syndrome treated with laser surgery. Am. J. Obstet. Gynecol. 2014; 210(6): 540. e1-7. https://dx.doi.org/10.1016/j.ajog.2014.01.002.
- Slaghekke F., Lopriore E., Lewi L., Middeldorp J.M., van Zwet E.W., Weingertner A.S. et al. Fetoscopic laser coagulation of the vascular equator versus selective coagulation for twin-to-twin transfusion syndrome: an open-label randomised controlled trial. Lancet. 2014; 383(9935): 2144-51. https://dx.doi.org/10.1016/S0140-6736(13)62419-8.
Received 26.05.2020
Accepted 17.06.2020
About the Authors
Kristina A. Gladkova, M.D., Ph.D., Senior Researcher at the Department of Fetal Medicine, Institute of Obstetrics;Head of the 1st Obstetric Department of Pathology of Pregnancy, V.I. Kulakov NMRC for OG&P of Minzdrav of Russia.
Tel.: +7(916)321-10-07. E-mail: k_gladkova@oparina4.ru. 4, Ac. Oparina str., 117997, Moscow, Russian Federation.
Kirill V. Kostyukov, M.D., Ph.D., Senior Researcher at the Department of Fetal Medicine, Institute of Obstetrics; Physician at the Unit of Functional and Ultrasound Diagnostics, Department of Diagnostic Imaging, V.I. Kulakov NMRC for OG&P of Minzdrav of Russia. Tel.: +7(926)214-97-84. E-mail: kostyukov_k@yahoo.com.
4, Ac. Oparina str., Moscow, 117997, Russian Federation.
For citation: Gladkova K.A., Kostyukov K.V. The effect of surgeon experience on outcomes of fetoscopic laser coagulation of placental anastomoses in twin-to-twin transfusion syndrome.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2020; 8: 57-63 (in Russian)
https://dx.doi.org/10.18565/aig.2020.8.57-63