1) Maternity Hospital No. 17, Saint Petersburg, Russia;
2) Department of Obstetrics, Gynecology, and Reproductology, Academician I.P. Pavlov First Saint Petersburg State Medical University, Ministry of Health of Russia, Saint Petersburg, Russia;
3) S.N. Davydov Department of Obstetrics and Gynecology, I.I. Mechnikov North-Western State Medical University, Ministry of Health of Russia, Saint Petersburg, Russia;
4) Department of Obstetrics, Gynecology, and Reproductology, Saint Petersburg State University, Saint Petersburg, Russia;
5) D.O. Ott Research Institute of Obstetrics, Gynecology, and Reproductology, Saint Petersburg, Russia
The paper provides an overview of modern concepts of different forms of twin-to-twin transfusion in monochorionic multiple pregnancy. It deals with diagnostic criteria for acute twin-to-twin transfusion during monochorionic twin delivery. The pathogenetic mechanisms of risk factors for acute twin-to-twin transfusion are considered. The differential diagnosis in chronic (twin-to-twin transfusion syndrome, twin anemia polycythemia sequence) and acute (single fetal death in twin pregnancy, placentofetal and acute twin-to-twin transfusions) forms of twin-to-twin transfusion is discussed in detail.
The possibility of predicting and preventing the development of acute twin-to-twin transfusion during childbirth has not been now defined; however, it is assumed that in some cases the changes in the cardiotocographic heart rate patterns may suspect specific disorders and make a timely delivery decision to minimize both antenatal losses and neonatal morbidity and mortality rates. The review gives possible approaches to postnatal correction for neonatal hematological disorders due to acute bypass surgery during monochorionic twin delivery.
Conclusion: Further investigations are needed to clarify diagnostic criteria and risk factors for acute twin-to-twin transfusion and optimal delivery tactics and to study long-term consequences for the health of children with this complication of monochorionic multiple pregnancy.
Authors’ contributions: Mikhailov A.V. – analyzing and generalizing the data available in the literature, editing and processing the manuscript; Romanovsky A.N., Osipova A.V., Kyanksep A.N., Volchenkova V.E. – collecting, analyzing, and generalizing the data available in the literature, writing the text of the article, executing the manuscript; Kuznetsov A.A., Tcyganova M.K., Saveleva A.A. – collecting, analyzing, and generalizing the data available in the literature, editing the manuscript.
Conflicts of interest: The authors declare that there are no conflicts of interest.
Funding: The article has been prepared for publication without sponsorship.
For citation: Mikhailov A.V., Romanovsky A.N., Volchenkova V.E.,
Kuznetsov A.A., Kyanksep A.N., Saveleva A.A., Osipova A.V., Tcyganova M.K.
Acute twin-to-twin transfusion in monochorionic multiple pregnancy.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2023; (2): 5-11 (in Russian)
https://dx.doi.org/10.18565/aig.2022.259
monochorionic twin
acute twin-to-twin transfusion
twin-to-twin transfusion syndrome
twin anemia polycythemia sequence
Распространенность беременностей двойней составляет приблизительно 1 случай на 90 беременностей, из которых около 30% приходится на монозиготные (идентичные) двойни [1]. Большинство – 70–75% – монозиготных двоен являются монохориальными с распространенностью в популяции 1 на 250–400 беременностей [1–3]. Монохориальное многоплодие относится к беременности высокого риска в значительной мере за счет специфических осложнений, связанных с наличием васкулярных анастомозов в единой для двух плодов сосудистой системе плаценты [1, 4–6].
В монохориальной плаценте выделяют поверхностные двунаправленные артерио-артериальные и вено-венозные и глубокие однонаправленные артерио-венозные анастомозы, функционирование которых может приводить к развитию неравномерного шунтирования крови между системами гемоциркуляции близнецов, в результате которого один из плодов становится донором, а другой – реципиентом [1, 5, 7].
Особенности ангиоархитектуры монохориальной плаценты определяют более высокие показатели перинатальной смертности и заболеваемости при этом типе, по сравнению с дихориальным многоплодием [1, 3]. Перинатальные потери при монохориальных двойнях почти в 2 раза выше по сравнению с дихориальными и в 4 раза выше по сравнению с таковыми при одноплодной беременности – 28, 16 и 7‰ соответственно [1, 3]. Однако эти показатели уровня перинатальной смертности не отражают общие плодовые потери при монохориальном многоплодии, так как наибольшие потери происходят до достижения срока жизнеспособности плодов, составляя в период с 10-й по 24-ю неделю беременности 120‰ [1]. Кроме того, частота развития неврологических осложнений при монохориальном типе плацентации многоплодной беременности в 4–5 раз выше, чем при дихориальном, что в 25–30 раз выше частоты подобных осложнений при одноплодной беременности [3]. Частота развития церебрального паралича у детей, рожденных от беременных двойней, достигает 1,2% [1]. При монохориальных двойнях частота детского церебрального паралича увеличивается как в связи с увеличением доли ранних преждевременных родов до 32 недель, так и в силу высокой частоты антенатальной гибели одного плода из двойни, которая может обуславливать поражение головного мозга выжившего плода вследствие гиповолемического шока, являющегося следствием острой трансфузии в систему циркуляции погибшего плода [1, 8, 9]. Таким образом, по мнению большинства экспертов, осложненное течение беременности и неонатального периода характерно для трети всех монохориальных двоен [3, 8].
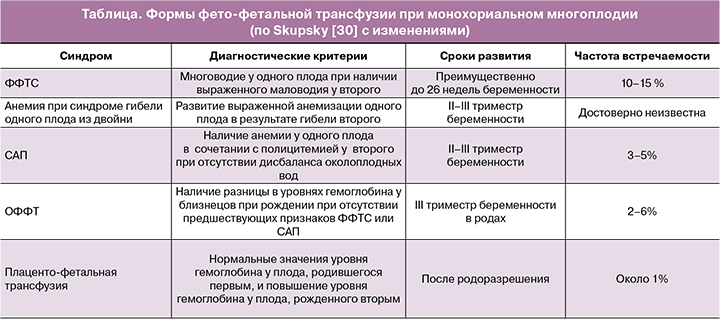
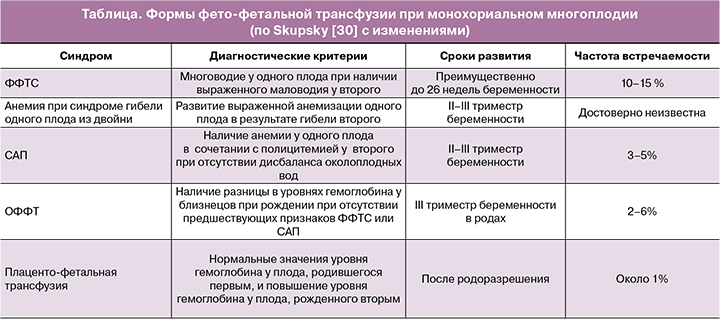
Среди специфических осложнений, связанных с несбалансированным шунтированием крови между плодами, выделяют хронические и острые формы. Фето-фетальный трансфузионный синдром (ФФТС), синдром анемии-полицитемии (САП) и синдром обратной артериальной перфузии относят к осложнениям, для которых характерно хроническое течение. Синдром гибели одного плода из двойни и острую интранатальную трансфузию считают острыми вариантами данного патологического процесса.
ФФТС является одним из наиболее тяжелых осложнений монохориального многоплодия, частота которого составляет среди всех монохориальных двоен 10–15% [5, 10–12]. В основе патогенеза ФФТС лежит несбалансированное шунтирование крови по глубоким артерио-венозным анастомозам от одного близнеца к другому при отсутствии компенсирующего возврата крови к последнему через поверхностные артерио-артериальные анастомозы, что приводит к каскаду активации вазоактивных факторов, обусловливающих развитие выраженного многоводия у плода-реципиента и критического маловодия вплоть до ангидрамниона у плода-донора [10–15]. Наиболее частым периодом развития клинической манифестации ФФТС является срок беременности с 15 до 26 недель беременности [11]; однако описано и более позднее его развитие в течение ее III триместра [12]. При отсутствии своевременного патогенетически обоснованного лечения методами фетальной хирургии с применением фетоскопической лазерной коагуляции (ФЛК) глубоких артерио-венозных анастомозов перинатальная смертность при ФФТС достигает 80–100% [3, 5, 10, 11, 16].
САП является другой формой хронической фето-фетальной трансфузии по артерио-венозным сосудистым анастомозам малого калибра. В отличие от ФФТС, при САП основным клиническим признаком является дискордантность уровней гемоглобина у плодов при отсутствии в их амниотических полостях дисбаланса околоплодных вод. Частота развития спонтанного САП составляет 3–5% всех монохориальных диамниотических двоен [3, 4, 17–19] и может являться следствием неполной ФЛК артерио-венозных анастомозов при лечении ФФТС в 2–16% этих внутриматочных вмешательств [3, 4, 17, 18]. Показатели антенатальной смертности при САП, по сравнению с неосложненным течением монохориального многоплодия, повышаются незначительно. Частота перинатальной заболеваемости меньше по сравнению с таковой при ФФТС ввиду того, что осложнения при САП в основном развиваются в раннем неонатальном периоде, что позволяет в большинстве случаев их своевременно диагностировать и успешно корригировать [3, 17].
Синдром обратной артериальной перфузии, частота которого в популяции составляет 1 на 9500–11 000 беременностей [20–24], рядом авторов расценивается как вариант экстремально раннего и тяжелого течения ФФТС, при котором на ранних стадиях эмбриогенеза присутствует крупный анастомоз между артериями пуповин эмбрионов, который обусловливает возникновение реверсного тока крови по единственной артерии пуповины у перфузируемого плода, сердце которого развивается рудиментарно или отсутствует полностью [20–23]. Таким образом, обеспечение жизнедеятельности этого плода-акардиуса невозможно без поддержания адекватной гемодинамики в фето-плацентарной системе плода-помпы [20, 22].
К острым формам фето-фетальной трансфузии относится синдром гибели одного плода из монохориальной двойни, который может рассматриваться, как перимортальный ФФТС [3]. Подобное состояние развивается в результате острого шунтирования крови вследствие возникновения градиента давления по васкулярным анастомозам плаценты из гемоциркуляции выжившего плода в сосудистую систему антенатально погибшего близнеца. В 15% случаев острая гиповолемия и выраженная анемизация второго плода могут обусловливать его последующую гибель [3], а в 18–34% – тяжелые поражения головного мозга в виде перивентрикулярной лейкомаляции и развитие полиорганной недостаточности у плода [3, 8, 12]. Тяжесть поражения органов и систем второго плода вследствие острого шунтирования крови в сосудистую сеть погибшего плода зависит от продолжительности этого эпизода и от объема шунтированной крови, который, в свою очередь, зависит от диаметра, типа и количества сосудистых анастомозов в монохориальной плаценте [3]. Близнецы, в плаценте которых имелось небольшое количество сосудистых анастомозов малого диаметра, менее подвержены тяжелым повреждениям по сравнению с теми, у которых в плаценте имели место крупные артерио-артериальные или артерио-венозные анастомозы [25–27].
Развитие острой фето-фетальной трансфузии (ОФФТ) при неосложненном течении беременности монохориальной двойней возможно во время родов [12], которое ряд авторов определяет как острый перинатальный или интранатальный фето-фетальный синдром [28]. Однако данное осложнение монохориальной беременности описано весьма скудно на основании единичных исследований, и в настоящее время не определена частота его развития, факторы риска и неонатальные исходы при пренатальном развитии ОФФТ [12, 28].
ОФФТ – это диагноз per exclusionem [29]. Как диагностические рассматриваются следующие критерии этого осложнения.
1) Исключение предшествующих хронических форм фето-фетальной трансфузии, таких как классический ФФТС и САП (таблица).
2) Выявление разницы уровней гемоглобина между близнецами при рождении. При этом необходимо иметь в виду, что вследствие острой реакции на кровопотерю может происходить выраженная периферическая вазоконстрикция, которая позволяет временно сохранять у плода-донора уровень гемоглобина в пределах нормы, а затем, спустя несколько часов после рождения, его уровень может значительно снижаться за счет гемодилюции [29]. Среди единичных опубликованных клинических случаев этого осложнения при монохориальном многоплодии отсутствует консенсус относительно степеней выраженности различий уровней гемоглобина у плодов, которые являются объективными критериями ОФФТ, что, безусловно, затрудняет проведение метаанализа данных. Ряд авторов рассматривают критерием ОФФТ разность уровней гемоглобина в крови плодов 50 г/л и более, в то время как другие по аналогии с САП используют его значение 80 г/л и более [28]. Установлено, что при монохориальной диамниотической двойне уровень гемоглобина крови плодов, родившихся вторыми, достоверно выше, чем у родившихся первыми [31]. Этот факт, возможно, связан с развитием фето-плацентарной трансфузии после рождения и клипирования пуповины первого плода, при которой кровь из его плацентарной территории по сосудистым анастомозам также может поступать в систему кровообращения еще не рожденного второго близнеца [29, 31]. Этот феномен также следует дифференцировать с ОФФТ, при которой повышение уровня гемоглобина одного плода будет сочетаться с анемией у второго.
3) Дополнительным диагностическим критерием ОФФТ могут рассматриваться клинические проявления циркуляторной недостаточности у плода-донора в виде бледности кожных покровов, тахикардии и гипотензии [29].
Частота развития ОФФТ в родах колеблется в пределах 1,5–5,5% [28, 30]. В отличие от хронического ФФТС в основе патогенеза ОФФТ лежит трансфузия крови по крупным поверхностным артерио-артериальным и вено-венозным анастомозам с низкой резистентностью в результате декомпенсации гемодинамического баланса между плодами, имевшего место на протяжении всей беременности. Потенциально возможными причинами развития острого шунтирования крови могут являться [30, 32]:
1) увеличение диаметра васкулярных анастомозов плаценты по мере прогрессирования беременности, что приводит к повышению в них объемного кровотока;
2) острый тромбоз одного из артерио-артериальных анастомозов, что вызывает гемодинамический дисбаланс между системами циркуляций плодов;
3) острый эпизод гипотензии или брадикардии у одного из плодов, возможный в результате компрессии пуповины, что может приводить к острому шунтированию крови по артерио-артериальным анастомозам;
4) маточные сокращения в прелиминарном периоде или в родах, приводящие к нарушению плодово-плацентарной гемодинамики.
Развитие ОФФТ в родах при неосложненном течении монохориальной многоплодной беременности в настоящее время является непредсказуемым событием. Существует мнение, что единственными достоверными факторами риска ОФФТ являются монохориальность и роды через естественные родовые пути [30]. Это мнение подтверждается тем, что не было зарегистрировано случаев ОФФТ в группе пациенток с монохориальной диамниотической двойней, родоразрешенных путем операции кесарева сечения в плановом порядке на фоне отсутствия маточных сокращений [28]. Наличие поверхностных артерио-артериальных и вено-венозных анастомозов является, скорее всего, необходимым, но не единственным условием развития ОФФТ, поскольку такие анастомозы выявляются при исследовании абсолютного большинства плацент и при неосложненном течении монохориального многоплодия [28].
Критерии диагностики развития ОФФТ в родах изучены недостаточно. Теоретически анемизация одного из плодов должна отражаться на характере кривой частоты сердечных сокращений при кардиотокографии, проявляясь в появлении паттерна в виде тахикардии и синусоидального ритма. Однако только менее половины подтвержденных случаев ОФФТ сопровождались подобными кардиотокографическими признаками нарушения жизнедеятельности плода в родах [28, 30, 33]. Одним из возможных объяснений этого феномена может быть предположение, что изменения сердечного ритма при кардиотокографии коррелируют с объемом и темпом шунтирования между системами гемоциркуляции плодов [28]. Таким образом, до сих пор однозначно неизвестно, может ли непрерывный кардиотокографический мониторинг своевременно установить развитие ОФФТ в родах. Тем не менее любые изменения жизнедеятельности плодов в родах должны оцениваться с учетом возможного острого шунтирования крови между близнецами и требовать пересмотра тактики ведения родов в пользу экстренного оперативного родоразрешения в зависимости от выраженности выявленных нарушений.
Лечение новорожденных детей при выявлении ОФФТ заключается в коррекции анемии у бывшего донора и проведении операции частичной обменной гемодилюции у бывшего реципиента [29]. Новорожденным детям с показателями гемоглобина менее 120 г/л в первые сутки жизни для коррекции анемии рекомендуется проведение гемотрансфузии в объеме 10–20 мл/кг. Для коррекции тяжелой анемии у новорожденных с показателями гемоглобина менее 80 г/л в сочетании с гиповолемическим шоком до трансфузии эритроцитсодержащих компонентов крови рекомендуют проведение инфузионной терапии для поддержания нормоволемии, респираторной терапии при наличии дыхательных нарушений и кардиотонической терапии при наличии гемодинамических нарушений. Частичную обменную трансфузию выполняют при уровне гематокрита более 70% или при уровне гематокрита 65–70% в сочетании с двумя или более симптомами полицитемии со стороны органов и систем новорожденного [29, 34, 35].
Учитывая недостаточное количество опубликованных исследований, посвященных ОФФТ при монохориальном многоплодии, оценка перинатальных исходов весьма затруднительна. Некоторые эксперты предполагают оптимистичный прогноз в отношении здоровья новорожденных при своевременном начале адекватной интенсивной терапии, однако описаны случаи как интранатальных, так и ранних неонатальных потерь, причиной которых послужила ОФФТ [3]. Оценка отдаленных перинатальных исходов затруднена ввиду отсутствия многоцентровых исследований и основывается на единичных опубликованных клинических случаях, поэтому влияние перенесенной ОФФТ в родах на дальнейшее развитие новорожденного не изучено.
Потенциальная угроза развития ОФФТ в родах послужила предметом дискуссии об оптимальной тактике родоразрешения и целесообразности использования планового кесарева сечения при неосложненном течении монохориального многоплодия [36–39]. С одной стороны, провоцирующим фактором развития ОФФТ является родоразрешение через естественные родовые пути [28], с другой – частота развития ОФФТ невысока и в большинстве случаев не приводит к существенному повышению перинатальных потерь. ОФФТ является весьма редким специфическим осложнением монохориального многоплодия, коварство которого заключается в быстром и часто непредсказуемом развитии. В связи с этим при родоразрешении через естественные родовые пути неосложненных монохориальных двоен система родовспоможения должна быть готова к оказанию специализированной помощи. Любые изменения паттерна кардиотокографии при монохориальном многоплодии должны расцениваться с учетом возможного развития острого шунтирования крови между плодами [28, 33].
Заключение
Требуются дальнейшие исследования для уточнения диагностических критериев и факторов риска ОФФТ, оптимальной тактики ведения родов, а также изучения отдаленных последствий в отношении здоровья детей при этом осложнении монохориального многоплодия.
- Lewi L., Van Schoubroeck D., Gratacós E., Witters I., Timmerman D.,Deprest J. Monochorionic diamniotic twins: complications and management options. Curr. Opin. Obstet. Gynecol. 2003; 15(2): 177-94.https://dx.doi.org/10.1097/00001703-200304000-00013.
- Lewi L., Gucciardo L., Van Mieghem T. Monochorionic diamniotic twin pregnancies: natural history and risk stratification. Fetal Diagn. Ther. 2010; 27(3): 121-33. https://dx.doi.org/10.1159/000313300.
- Gratacós E., Ortiz J.U., Martinez J.M. A systematic approach to the differential diagnosis and management of the complications of monochorionic twin pregnancies. Fetal Diagn. Ther. 2012; 32(3): 145-55.https://dx.doi.org/10.1159/000342751.
- Костюков К.В., Гладкова К.А. Диагностика фето-фетального трансфузионного синдрома, синдрома анемии-полицитемии при монохориальной многоплодной беременности. Акушерство и гинекология. 2016; 1: 10-5. [Kostyukov K.V., Gladkova K.A. Diagnosis of twin-to-twin transfusion syndrome and anemia-polycythemia syndrome in monochorionic multiple pregnancy. Obstetrics and Gynecology. 2016; (1): 10-5. (in Russian)].https://dx.doi.org/10.18565/aig.2016.1.10-15.
- Костюков К.В., Сакало В.А., Гладкова К.А., Шакая М.Н., Ионов О.В., Тетруашвили Н.К. Перинатальные исходы монохориальной многоплодной беременности, осложненной фето-фетальным трансфузионным синдромом. Акушерство и гинекология. 2020; 8: 72-80. [Kostyukov K.V., Sakalo V.A., Gladkova K.A., Shakaya M.N., Ionov O.V., Tetruashvili N.K. Perinatal outcomes of monochorionic multiple pregnancies complicated by twin-to-twin transfusion syndrome. Obstetrics and Gynecology. 2020; (8): 72-80. (in Russian)]. https://dx.doi.org/10.18565/aig.2020.8.72-80.
- Михайлов А.В., Романовский А.Н., Шлыкова А.В., Кузнецов А.А., Каштанова Т.А., Новикова А.В., Потанин С.А. Применение лазерной коагуляции сосудистых анастомозов плаценты при фето-фетальном трансфузионном синдроме. Таврический медико-биологический вестник. 2016; 19(2): 167-71. [Mikhailov A.V., Romanovsky A.N., Shlykova A.V., Kuznetsov A.A., Kashtanova T.A., Novikov A.V., Potanin S.A. Laser coagulation of vascular placental anastomoses in twin-to-twin-transfusion syndrome. Taurian Medical and Biological Bulletin. 2016; 19(2): 167-71.(in Russian)].
- Bajoria R., Wigglesworth J., Fisk N.M. Angioarchitecture of monochorionic placentas in relation to the twin-twin transfusion syndrome. Am. J. Obstet. Gynecol. 1995; 172(3): 856-63. https://dx.doi.org/10.1016/0002-9378(95)90011-x.
- Кузнецов А.А., Романовский А.Н., Шлыкова А.В., Каштанова Т.А., Шман В.В., Кянксеп И.В., Мовчан В.Е., Державина Н.Е., Савельева А.А., Овсянников Ф.А., Михайлов А.В. Синдром гибели одного плода при многоплодной беременности. Трансляционная медицина. 2019; 6(5): 31-8. [Kuznetsov A.A., Romanovsky A.N., Shlykova A.V., Kashtanova T.A.,Shman V.V., Kyanksep I.V., Movchan V.E., Derzhavina N.E.,Savel’eva A.A., Ovsyannikov F.A., Mikhailov A.V. Single fetal demise in multiple pregnancy. Translational Medicine. 2019; 6(5): 31-8. (in Russian)]. https://dx.doi.org/10.18705/2311-4495-2019-6-5-.
- Hillman S.C., Morris R K., Kilby M.D. Co-twin prognosis after single fetal death: a systematic review and meta-analysis. Obstet. Gynecol. 2011; 118(4): 928-940. https://dx.doi.org/10.1097/AOG.0b013e31822f129d.
- Овсянников Ф.А., Романовский А.Н. Современные подходы к лечению фето-фетального трансфузионного синдрома. Трансляционная медицина. 2017; 4(4): 36-42. [Ovsyannikov F.A., Romanovsky A.N. Current treatment of twin-to-twin transfusion syndrome. Translational Medicine. 2017; 4(4): 36-42. (in Russian)]. https://dx.doi.org/10.18705/2311-4495-2017-4-4-36-42.
- Benoit R.M., Baschat A.A. Twin-to-twin transfusion syndrome: prenatal diagnosis and treatment. Am. J. Perinatol. 2014; 31(7): 583-94.https://dx.doi.org/10.1055/s-0034-1372428.
- Lopriore E., Middeldorp J.M., Sueters M. Twin-to-twin transfusion syndrome: from placental anastomoses to long-term neurodevelopmental outcome. Curr. Pediatr. Rev. 2005; 1(3): 191-203. https://dx.doi.org/10.2174/157339605774574999.
- Quintero R.A., Morales W.J., Allen M.H., Bornick P.W., Johnson P.K., Kruger M. Staging of twin-twin transfusion syndrome. J. Perinatol. 1999; 19(8, Pt. 1): 550-5. https://dx.doi.org/10.1038/sj.jp.7200292.
- WAPM Consensus Group on Twin-to-Twin Transfusion. Twin to-twin transfusion syndrome (TTTS). J. Perinat. Med. 2011; 39(2): 107-12.https://dx.doi.org/10.1515/jpm.2010.147.
- Acosta-Rojas R., Becker J., Munoz-Abellana B., Ruiz C., Carreras E., Gratacos E. Twin chorionicity and the risk of adverse perinatal outcome. Int. J. Gynecol. Obstet. 2007; 96(2): 98-102. https://dx.doi.org/10.1016/j.ijgo.2006.11.002.
- Faye-Petersen O.M., Crombleholme T.M. Twin-to-Twin transfusion syndrome Part 2. Infant anomalies, clinical interventions, and placental examination. Neo Reviews. 2008; 9(9): e380-92.
- Михайлов А.В., Романовский А.Н., Каштанова Т.А., Кузнецов А.А., Кянксеп И.В., Волчёнкова В.Е., Савельева А.А. Синдром анемии-полицитемии – современные подходы к диагностике и антенатальной коррекции. Вопросы гинекологии, акушерства и перинатологии. 2021; 20(2): 134-40. [Mikhailov A.V., Romanovsky A.N., Kashtanova T.A., Kuznetsov A.A., Kyanksep I.V., Volchenkova V.E., Savel’eva A.A. Twin anemia polycythemia sequence – modern approaches to diagnosis and antenatal correction. Issues of Gynecology, Obstetrics and Perinatology. 2021; 20(2): 134-40. (in Russian)]. https://dx.doi.org/10.20953/1726-1678-2021-2-134-140.
- Slaghekke F., Kist W.J., Oepkes D., Pasman S.A., Middeldorp J.M., Klumper F.J. et al. Twin anemia-polycythemia sequence: diagnostic criteria, classification, perinatal management and outcome. Fetal Diagn. Ther. 2010; 27(4): 181-90. https://dx.doi.org/10.1159/000304512.
- Российское общество акушеров-гинекологов (РОАГ), ООО «Ассоциация анестезиологов-реаниматологов (ААР)», Ассоциация акушерских анестезиологов-реаниматологов. Клинические рекомендации. Многоплодная беременность. 2020. [Russian Society of Obstetricians and Gynecologists (ROAG), Association of Anesthesiologists-Resuscitators (AAR), Association of Obstetric Anesthesiologists-Resuscitators. Clinical Guidelines. Multiple pregnancy. 2020. (in Russian)].
- Костюков К.В., Гладкова К.А. Диагностика синдрома селективной задержки роста плода, синдрома обратной артериальной перфузии при монохориальной многоплодной беременности. Акушерство и гинекология. 2016; 2: 14-8. [Kostyukov K.V., Gladkova K.A. Diagnosis of selective fetal growth restriction syndrome and reversed arterial perfusion in monochorionic multiple pregnancy. Obstetrics and Gynecology. 2016; (2): 14-8. (in Russian)].https://dx.doi.org/10.18565/aig.2016.2.14-18.
- Михайлов А.В., Романовский А.Н., Кузнецов А.А., Каштанова Т.А., Шлыкова А.В., Кянксеп И.В. Синдром обратной артериальной перфузии: патофизиологические аспекты и принципы диагностики. Таврический медико-биологический вестник. 2018; 21(2-2): 195-201. [Mikhailov A.V., Romanovsky A.N., Kuznetsov A.A., Kashtanova T.A., Shlykova A.V., Kyanksep I.V. Pathophysiological aspects and diagnostic principles of twin reversed arterial perfusion. Taurian Medical and Biological Bulletin. 2018;21(2-2): 195-201. (in Russian)].
- Костюков К.В., Павлов К.А., Дубова Е.А., Стыгар А.М., Гус А.И., Щёголев А.И. Синдром обратной артериальной перфузии (клинические наблюдения и обзор литературы). Медицинская визуализация. 2012; 6: 120-6. [Kostukov K.V., Pavlov K.A., Dubova E.A., Stygar A.M., Gus A.I., Shchegolev A.I. Twin reversed arterial perfusion syndrome (Case report and literature review). Medical Imaging. 2012; (6): 120-6. (in Russian)].
- Костюков К.В., Гладкова К.А., Тетруашвили Н.К. Тактика ведения беременности при синдроме обратной артериальной перфузии. Акушерство и гинекология. 2018; 11: 44-9 [Kostyukov K.V., Gladkova K.A., Tetruashvili N.K. Pregnancy management tactics in reversed arterial perfusion syndrome. Obstetrics and Gynecology. 2018; (11): 44-9. (in Russian)].https://dx.doi.org/10.18565/aig.2018.11.44-49.
- van Gemert M.J.C., van den Wijngaard J.P.H.M., Vandenbussche F.P.H.A. Twin reversed arterial perfusion sequence is more common than generally accepted. Birth Defects Res. A Clin. Mol. Teratol. 2015; 103(7): 641-3.https://dx.doi.org/10.1002/bdra.23405.
- Woo H.H., Sin S.Y., Tang L.C. Single foetal death in twin pregnancies: review of the maternal and neonatal outcomes and management. Hong Kong Med. J. 2000; 6(3): 293-300.
- De Villiers S.F., Slaghekke F., Middeldorp J.M., Walther F.J., Oepkes D., Lopriore E. Arterio-arterial vascular anastomoses in monochorionic placentas with and without twin–twin transfusion syndrome. Placenta. 2012; 33(8): 652-4. https://dx.doi.org/10.1016/j.placenta.2012.05.003.
- Lewi L., Deprest J., Hecher K. The vascular anastomoses in monochorionic twin pregnancies and their clinical consequences. Am. J. Obstet. Gynecol. 2013; 208(1): 19-30. https://dx.doi.org/10.1016/j.ajog.2012.09.025.
- Lopriore E., Holtkamp N., Sueters M., Middeldorp J.M., Walther F.J., Oepkes D. Acute peripartum twin–twin transfusion syndrome: Incidence, risk factors, placental characteristics and neonatal outcome. J. Obstet. Gynaecol. Res. 2014; 40(1): 18-24. https://dx.doi.org/10.1111/jog.12114.
- Lopriore E., Oepkes D. Fetal and neonatal haematological complications in monochorionic twins. Semin. Fetal Neonatal Med. 2008; 13(4): 231-8.https://dx.doi.org/10.1016/j.siny.2008.02.002.
- Skupski D.W., Sylvestre G., Di Renzo G.C., Grunebaum A. Acute twin-twin transfusion syndrome in labor: pathophysiology and associated factors. J. Matern. Fetal Neonatal Med. 2012; 25(5): 456-60. https://dx.doi.org/10.3109/14767058.2011.637146.
- Verbeek L., Zhao D.P., Middeldorp J.M., Oepkes D., Hooper S.B., Te Pas A.B., Lopriore E. Haemoglobin discordances in twins: due to differences in timing of cord clamping? Arch. Dis. Child Fetal Neonatal Ed. 2017; 102(4): 324-8. https://dx.doi.org/10.1136/archdischild-2016-311822.
- Tan T.Y.T., Denbow M.L., Cox P.M., Talbert D., Fisk N.M. Occlusion of arterio-arterial anastomosis manifesting as acute twin–twin transfusion syndrome. Placenta. 2004; 25(2-3): 238-42. https://dx.doi.org/10.1016/j.placenta.2003.08.018.
- Suzuki S., Iwasaki N., Ono S., Igarashi M., Murata T. Fetal heart rate patterns in monochorionic twins following acute twin-twin transfusion. Obstet. Gynecol. Int. 2009; 2009: 498530. https://dx.doi.org/10.1155/2009/49853.
- Общероссийская общественная организация содействия развитию неонатологии «Российское общество неонатологов» (РОН). Клинические рекомендации. Врожденная анемия вследствие кровопотери у плода. 2021. [All-Russian Public Organization for Promoting the Development of Neonatology "Russian Society of Neonatologists" (RSN). Clinical guidelines. Congenital anemia due to fetal blood loss. 2021. (in Russian)].
- Общероссийская общественная организация содействия развитию неонатологии «Российское общество неонатологов» (РОН), Общественная организация «Российская ассоциация специалистов перинатальной медицины» (РАСПМ). Клинические рекомендации. Диагностика и лечение полицитемии новорожденных. 2015. [All-Russian Public Organization for Promoting the Development of Neonatology "Russian Society of Neonatologists" (RSN), Public Organization "Russian Association of Perinatal Medicine Specialists" (RAPMS). Clinical guidelines. Diagnosis and treatment of polycythemia in newborns. 2015. (in Russian)].
- Aviram A., Lipworth H., Asztalos E.V., Mei-Dan E., Melamed N., Cao X. et al. Delivery of monochorionic twins: lessons learned from the Twin Birth Study. Am. J. Obstet. Gynecol. 2020; 223(6): 916.e1-916.e9.https://dx.doi.org/10.1016/j.ajog.2020.06.048.
- Melka S., Miller J., Fox N.S. Labor and delivery of twin pregnancies. Obstet. Gynecol. Clin. 2017; 44(4): 645-54. https://dx.doi.org/10.1016/j.ogc.2017.08.004.
- Pestana I., Loureiro T., Almeida A., Rocha I., Rodrigues R.M., Rodrigues T. Effect of mode of delivery on neonatal outcome of monochorionic diamniotic twin pregnancies: a retrospective cohort study. J. Reprod. Med. 2013; 58(1-2): 15-8.
- Weisz B., Hogen L., Yinon Y., Mazaki S., Gindes L., Schiff E. et al. Mode of delivery and neonatal outcome in uncomplicated monochorionic twin pregnancies. J. Matern. Fetal Neonatal Med. 2012; 25(12): 2721-4.https://dx.doi.org/10.3109/14767058.2012.712560.
Received 03.11.2022
Accepted 13.01.2023
Anton V. Mikhailov, Dr. Med. Sci., Director and Chief of the Maternity Hospital No. 17, 4-1 Lesnozavodskaya str., St. Petersburg, 192174, Russia;
Professor at the Department of Obstetrics, Gynecology and Reproduction, Pavlov First Saint Petersburg State Medical University, Ministry of Health of Russia,
6-8 L'va Tolstogo str., St. Petersburg, 197022, Russia; Professor at the Department of Obstetrics and Gynecology, I.I. Mechnikov North-Western State Medical University, Ministry of Health of Russia, 47, Piskarevsky Ave., St. Petersburg, 195067, Russia; Chief Researcher, D.O. Ott Institute of Obstetrics, Gynecology and Reproductology,
3 Mendeleevskaya line, St. Petersburg, 199034, Russia,
mav080960@gmail.com
Artem N. Romanovsky, PhD, obstetrician-gynecologist, ultrasound diagnostician, Maternity Hospital No. 17, 4-1 Lesnozavodskaya str., St. Petersburg, 192174, Russia;
Associate Professor at the Department of Obstetrics, Gynecology and Reproductology, St. Petersburg State University, 8а, 21-line, St. Petersburg, 199004, Russia.
Veronika E. Volchenkova, obstetrician-gynecologist, ultrasound diagnostician, Maternity Hospital No. 17, 4-1 Lesnozavodskaya str., St. Petersburg, 192174, Russia;
postgraduate of the Department of Obstetrics and Gynecology, I.I. Mechnikov North-Western State Medical University, Ministry of Health of Russia,
47, Piskarevskiy Ave., St. Petersburg, 195067, Russia.
Alexandr A. Kuznetsov, PhD, obstetrician-gynecologist, Maternity Hospital No. 17, 4-1 Lesnozavodskaya str., St. Petersburg, 192174, Russia;
assistant of the Department of Obstetrics, Gynecology and Reproduction, Pavlov First St. Petersburg State Medical University, Ministry of Health of Russia,
6-8, L'va Tolstogo str., St. Petersburg, 197022, Russia.
Alexey N. Kyanksep, Head of Neonatology, Maternity Hospital No. 17, Lesnozavodskaya str. 4-1, St. Petersburg, 192174, Russia.
Anna A. Saveleva, ultrasound diagnostician, Maternity Hospital No. 17, 4-1 Lesnozavodskaya str., St. Petersburg, 192174, Russia.
Anastasia V. Osipova, resident at the Department of Obstetrics, Gynecology and Reproductology, St. Petersburg State University, 8а, 21-line, St. Petersburg, 199004, Russia.
Maria K. Tcyganova, resident at the Department of Obstetrics, Gynecology and Reproductology, St. Petersburg State University, 8а, 21-line, St. Petersburg, 199004, Russia.
Corresponding author: Anton V. Mikhailov,
mav080960@gmail.com