An operational study of the effectiveness of early diagnosis in female reproductive disorders associated with genital tuberculosis
Objective. Based on the amended list of risk factors for genital tuberculosis, to conduct an operational study of active identification of women at risk of reproductive disorders associated with genital tuberculosis.Leshchenko O.Ya., Malanova A.B., Atalyan A.V.
Material and methods. The study was conducted at the Research Center for Problems of Family Health and Human Reproduction (Irkutsk), G.D. Dugarova Republican Tuberculosis Clinical Hospital (Ulan-Ude), and Republican Clinical Gynecological Hospital (Ulan-Ude) in 2011–2017. The study analyzed the incidence of female genital tuberculosis in 2011 among patients of maternity clinics of City Polyclinic No. 6 and City Polyclinic No. 4. Obstetrician-gynecologists providing outpatient care at the City Polyclinic No. received a course of six once-monthly lectures. The developed algorithm for genital tuberculosis risk stratification was introduced with subsequent referrals of patients to G.D. Dugarova Republican Tuberculosis Clinical Hospital, Ulan-Ude since the beginning of February 2012. After the intervention, the incidence of genital tuberculosis was assessed in the control and experimental health care facilities (2015).
Results. An extended list of risk factors for genital tuberculosis in women with reproductive disorders has been proposed and introduced into clinical practice. The list included new and updated criteria: chronic pelvic pain, a history of failed IVF attempts, specific types of menstrual disorders, temporary criteria for treatment failure of menstrual dysfunction and pelvic inflammatory diseases. The operational study estimated the implementation of an algorithm for active identification of risk factors of female reproductive disorders associated with genital tuberculosis, which resulted in 3.6-fold improvement of diagnosis of genital tuberculosis in outpatient settings.
Conclusion. The operational study of the active introduction of the extended list of risk factors in outpatient settings increased the effectiveness of early diagnosis of female reproductive disorders associated with genital tuberculosis: 14 out of 390 (3.6%), which corresponds to 0.5 per 100 000 population versus zero incidence without intervention.
Keywords
In recent years, the problem of genital tuberculosis in Russia has been extremely relevant due to the projected growth in extrapulmonary tuberculosis incidence rate, its inconsistency with official indicators and a high proportion of tuboperitoneal infertility [1, 2]. Female genital tuberculosis is rare and difficult-to-diagnose with an incidence ranging from 0.5 to 2.0 cases per 100 000 population [3–5]. In the Republic of Buryatia, the incidence rate of female genital tuberculosis in 2010 – 2012 was 1.2 per 100 000 population, which is 2.2-fold higher than in the Russian Federation (0.5 per 100 000) [6]. According to Russian authors, in 25–36% of patients, genital tuberculosis is diagnosed 10–15 years after the onset of the disease as incidental findings during surgery (10–25%), which negatively affects reproductive function [4, 7]. From 60% to 97% of women with genital tuberculosis are infertile [3, 8].
Early diagnosis and timely therapy of female genital tuberculosis remain highly relevant problems which, if solved, would significantly improve patients’ fertility and quality of life. The absence of specific clinical symptoms, latent course, low detection rates of the pathogen in pathological material results in a low detection rate of genital tuberculosis in women with reproductive disorders (Kolesnikova, 2014). The formation of a risk group for genital tuberculosis among women can provide several times better detection of tuberculosis [4, 5].
Aim: Based on the amended list of risk factors for genital tuberculosis, to conduct an operational study of active identification of women at risk of reproductive disorders associated with genital tuberculosis.
Material and methods
The study was conducted at the Research Center for Problems of Family Health and Human Reproduction (Irkutsk), G.D. Dugarova Republican Tuberculosis Clinical Hospital (Ulan-Ude), and Republican Clinical Gynecological Hospital (Ulan-Ude) in 2011–2017.
Analysis of medical records. The analysis was based on annual statistical reports provided by outpatient maternity clinics of City Polyclinic No. 6 and City Polyclinic No. 4 and outpatient medical records (form No. 025/у- 87 of the Ministry of Health of the Russian Federation) for the period from 2011 to 2015.
Questionnaire survey. The survey was conducted using a questionnaire based on the WHO questionnaire card (WHO project No. 88093). The questionnaire includes questions about age, marital status, contraceptive methods, reproductive plans, and reproductive and somatic history. The questionnaire was supplemented with several questions and grouped into sections: personal data (age, nationality, education, social status, place of residence), complaints at presentation, concomitant gynecological diseases, a history of somatic diseases and tuberculosis. The patients’ history of disease was examined based on the principles of examination and interviewing of TB patients. The analysis included the refinement of the first manifestation of the disease, the presence of subfebrile fever, its duration, and variability; increasing symptoms of intoxication (weakness, sweating, a decreased ability to work, lack of appetite, loss of body weight). The analysis included a history of tuberculin test conversion in childhood and adolescence, previous history of tuberculosis of any other site, contacts with tuberculosis patients in private life or at work. The questionnaire for estimating the socio-biological, family and domestic status of women of reproductive age included questions of the socio-biological, family and domestic status, obstetric and gynecological history, complaints and objective status.
Gynecological history taking involved the following information: age of menarche, features of the formation of menstrual function: regularity, the presence of pain, the blood loss. We studied the nature and rhythm of menstruation and menstrual cramps. Analysis of the reproductive function included the age of sexual debut, the outcome of the first pregnancy, the number of births, abortions, miscarriages, missed abortions, ectopic pregnancies, complications of postpartum and post-abortion periods. Women, who failed to achieve a clinical pregnancy after 12 months of regular unprotected sexual intercourse, were considered infertile. We analyzed the duration of infertility, the fertility of the sexual partner, the results of previous examinations and treatment of sexual partners.
The factual materials obtained in the form of quantitative and qualitative clinical or para-clinical parameters were recorded in the questionnaires and computer database “Register of women of reproductive age with risk factors for genital tuberculosis” No. 2017620351 of 03/27/2017.
General clinical examination. An objective examination included an assessment of physical development using a body mass index proposed by G. Brey as a weight-to-height ratio (BMI = kg/m2); measurement of blood pressure (BP), and body temperature. If the patients had a subfebrile fever, temperature curves were plotted on a temperature chart. The patients were evaluated for the presence of trophic skin changes and hirsutism. The standard gynecological examination included breast examination with palpation, assessment of the presence and degree of galactorrhea, and degree and distribution of hair growth.
Statistical analysis was performed using Statistica 6.1, StatSoft, Inc., USA (license holder – Research Center for Family Health Problems and Human Reproduction). Statistical significance was assumed for p < 0.05.
From 2011 to 2015, an operational study was conducted at Ulan-Ude city polyclinics No. 6 and No. 4. According to WHO experts’ recommendations, the study included several steps: choosing a strategy or program, conducting a pretest to assess the initial state of the problem, intervention posttest to assess the effectiveness of implementation.
Operational Study Design
Pretest. The analysis of the incidence of female genital tuberculosis for 2011 was conducted in maternity clinics of City Polyclinic № 6 and City Polyclinic № 4. As reported by Ulan-Ude Republican Tuberculosis Clinical Hospital, in 2011, no cases genital tuberculosis were diagnosed among women attending maternity clinics of City Polyclinics No. 4 and No. 6.
Intervention. Obstetrician-gynecologists providing outpatient care at the City Polyclinic No. 6 received a course of six once-monthly lectures. The developed algorithm for genital tuberculosis risk stratification was introduced with subsequent referrals of patients to G.D. Dugarova Republican Tuberculosis Clinical Hospital in Ulan-Ude since the beginning of February 2012. In 2012, outpatient medical cards of all women of reproductive age visiting the experimental maternity clinic for any reason were marked indicating that the patients belong to the genital tuberculosis risk group.
Posttest. An assessment of the incidence of genital tuberculosis after intervention in the control and experimental health care facilities (2015)
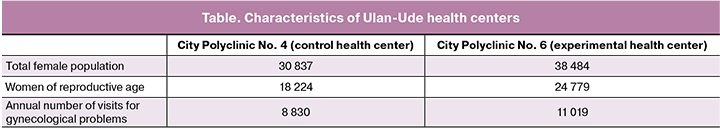
The method of unit selection. Two health care facilities were chosen at the City Polyclinic No. 4 (control) and the City Polyclinic No. 6 (experimental), geographically located in Zheleznodorozhny district and Vostochny settlement of Ulan-Ude, respectively. The introduction was carried out in February 2012. Both health care facilities were comparable in the number of the population served in 2011: 38484 and 30837 women were registered at the City Polyclinic № 6 and City Polyclinic № 4, respectively. Of them, 20779 and 18224 women were of reproductive age, respectively (table). In 2011, at the City Polyclinic No. 6, 489, 497, 121, 71, and 11 patients were under follow-up observation for chronic pelvic inflammatory diseases, menstrual dysfunction, endometriosis, female infertility, and pregnancy loss, respectively. At the City Polyclinic No. 4, 490, 323, 121, 39, and 30 patients were under follow-up observation for chronic pelvic inflammatory diseases, menstrual dysfunction, endometriosis, female infertility, and pregnancy loss, respectively.
The intervention consisted of the methodological work with obstetricians and gynecologists, the active introduction of the extended list of risk factors and the formation of a genital tuberculosis risk group among women with reproductive disorders and the immediate referral of the patients to the G.D. Dugarova Republican Tuberculosis Clinical Hospital (Ulan-Ude) to rule out or confirm the diagnosis of genital tuberculosis.
Results and discussion
Based on the analysis of literature including methodological recommendations “Organization of the identification of patients with tuberculosis in outpatient clinics and hospitals”, approved by the Ministry of Health of the Russian Federation on July 20, 2007 No. 5589-RC, we developed a new expanded list of risk factors for the formation of a genital tuberculosis risk group among women of reproductive age:
- Primary infertility;
- Secondary infertility;
- Chronic uterine and adnexal inflammatory diseases with frequent exacerbations (more than four episodes per year) that are not amenable to medical treatment (ineffectiveness of antibacterial, anti-inflammatory therapy for 14–21 days);
- A history of surgery for uterine and adnexal inflammatory diseases and currently ongoing pain syndrome and/or subfebrile fever;
- Chronic pelvic pain (ineffectiveness of non-specific, antibacterial, anti-inflammatory therapy);
- Patients with adnexal masses (especially fixed adnexal masses);
- Women with sexual infantilism;
- Menstrual disorders including oligomenorrhea, hypomenorrhea, secondary amenorrhea, abnormal uterine bleeding with failed medical therapy (including hormonal therapy) within 3–6 months;
- A history of missed abortion, spontaneous miscarriage, and pregnancy loss;
- A history of ectopic pregnancy;
- A history of failed IVF attempts;
- Subfebrile fever of unknown origin (with the exclusion of other somatic pathology);
- Female adolescents with a history of the conversion of tuberculin tests from negative to positive, who have functional genital disorders or non-localized abdominal pain;
- Women of reproductive age with a history of tuberculosis of any site;
- Women whose husbands suffer from urogenital tuberculosis.
As compared with the previously discussed 2007 recommendations, our proposed extended list of risk groups for verifying female genital tuberculosis includes additional criteria: chronic pelvic pain and a history of failed IVF attempts. Also, in the updated list, we specify the timing of treatment failure in pelvic inflammatory diseases, types of menstrual disorders, and the timing of treatment failure in these disorders.
From 2012 to 2015, women with risk factors were selected at the City Polyclinic No. 6 (experimental) as a result of the implementation of the algorithm to form a genital tuberculosis risk group. Of 390 patients, who were referred to G.D. Dugarova Republican Tuberculosis Clinical Hospital for in-depth examination between 2012 and 2014, fourteen (3.6%) were diagnosed with genital tuberculosis and reproductive disorders. In 2014, the incidence rate of female genital tuberculosis was 0.5 per 100,000 population. In the City Polyclinic No.4, which did not use the algorithm for identifying risk factors for genital tuberculosis, the incidence rate of genital tuberculosis remained at the same zero level.
Conclusion
One of the priorities in the active detection of genital tuberculosis is a thorough analysis and identification of risk factors for this disease. Formation of a risk group among women has been proven to result in several-fold better tuberculous detection. As compared with the previously discussed 2007 methodological recommendations, our proposed extended list of risk groups for verifying female genital tuberculosis includes additional criteria: chronic pelvic pain and a history of failed IVF attempts. Also, in the updated list, we specify the timing of treatment failure in pelvic inflammatory diseases, types of menstrual disorders, and the timing of treatment failure in these disorders. The introduction of a new algorithm for the active detection of patients with risk factors in outpatient settings resulted in the detection of genital tuberculosis in 3.6% of women with reproductive disorders against zero detected cases without intervention.
Thus, the introduction of an extended list of risk factors for genital tuberculosis and active selection of the genital tuberculosis risk group will allow outpatient physicians to refer patients with reproductive disorders to the TB health service promptly. That, in turn, will allow the early diagnosis of genital tuberculosis with a full course of specific anti-tuberculosis therapy, which may help preserve fertility in this patients’ category.
The active introduction of the expanded list of risk factors for genital tuberculosis, which included new and updated criteria, increased the effectiveness of early diagnosis of female reproductive disorders associated with genital tuberculosis in outpatient settings: 14 out of 390 (3.6%), which corresponds to 0.5 per 100,000 population versus zero incidence without intervention.
References
- Лещенко О.Я., Маланова А.Б., Аталян А.В. Диагностика и прогноз репродуктивных нарушений, ассоциированных с туберкулезом половых органов у женщин. В кн.: Сухих Г.Т., Адамян Л.В., ред. XI Международный конгресс по репродуктивной медицине. Москва, 17-20 января. М.: МЕДИ Экспо; 2017: 77-9. [ Leshhenko O. Ja., Malanova A. B.,Ataljan A. V. Diagnosis and prognosis of reproductive disorders associated with genital tuberculosis in women. In the book: Sukhikh G.T., Adamyan L.V., ed. XI International Congress on Reproductive Medicine. Moscow, January 17-20. M .: MEDI Expo; 2017: 77-9. (in Russian)]
- Мушкин А.Ю., Белиловский Е.М., Першин А.А. Внелегочной туберкулез в Российской Федерации: сопоставление некоторых официальных данных и результатов анкетного скрининга. Медицинский альянс. 2013; 1: 80-5.[ Mushkin A. Ju., Belilovskij E. M., Pershin A. A.Extrapulmonary tuberculosis in the Russian Federation: a comparison of some official data and the results of questionnaire screening. Medical Alliance. 2013; 1: 80-5. (in Russian)]
- Мордык А.В., Яковлева А.А., Николаева И.Н., Леонтьев В.В. Актуальность проблемы внелегочного туберкулеза в современных эпидемиологических условиях. Тихоокеанский медицинский журнал. 2015; 3: 19-21. [ Mordyk A.V., Jakovleva A.A., Nikolaeva I.N., Leont’ev V.V. The urgency of the problem of extrapulmonary tuberculosis in modern epidemiological conditions. Pacific Medical Journal. 2015; (3): 19-21. (in Russian)]
- Кульчавеня Е.В., Краснов В.А., Щербань М.Н. Избранные вопросы фтизиоурологии. Новосибирск: Наука; 2010. 142c. [ Kul’chavenja E.V., Krasnov V.A., Shherban’ M.N. Selected questions of phthisiology. Novosibirsk: Science; 2010. 142p. (in Russian)]
- Колесникова Л.И., Лещенко О.Я., Маланова А.Б. Современный взгляд на проблему туберкулеза женских половых органов. Акушерство и гинекология. 2014; 9: 24-9. [Kolesnikova L. I., Leshhenko O. Ja., Malanova A. B. A modern view on the problem of female genital tuberculosis. Obstetrics and gynecology. 2014; (9): 24-9. (in Russian)]
- Маланова А.Б., Цыбикова Л.Б., Лещенко О.Я., Сутурина Л.В. Эпидемиологическая ситуация по туберкулезу женских половых органов в республике Бурятия за период 2003–2011 гг. Acta Biomedica Scientifica. 2012; 3-1: 101-3. [ Malanova A. B., Cybikova L. B., Leshhenko O. Ja., Suturina L.V. Epidemiological situation of female genital tuberculosis in the Republic of Buryatia for the period 2003-2011. Acta Biomedica Scientifica. 2012; (3-1): 101-3. (in Russian)]
- Leshchenko O.Y., Malanova A.B., Atalyan A.V. The hierarchy of complaints of infertile women from group of risk of genital tuberculosis and endometriosis. J. Endometr. Pelvic Pain Disord. 2015; 7(Suppl. 1): 74-5.
- Arora R., Sharma J.B. Female genital tuberculosis--a diagnostic and therapeutic challenge. Indian J. Tuberc. 2014; 61(2): 98-102.
Received 06.02.2018
Accepted 02.03.2018
About the Authors
Leshchenko, Olga Y., MD, leading Researcher, head of the Laboratory of Socially Related Infections in Reproductology, Research Center for Problems of Family Health and Human Reproduction.. 664003, Russia, Irkutsk, Timirjazeva str. 16. Tel.: +79643521588. E-mail: loyairk@mail.ruMalanova, Auna B., phthisio-gynecologist at the G.D. Dugarova Republican Tuberculosis Clinical Hospital.
670004, Russia, Ulan-Ude, Batozhabaya str. 10. Tel.: +79140534848. E-mail: malanova@list.ru
Atalyan, Alina V., PhD, senior researcher at Laboratory of Socially Related Infections in Reproductology, Research Center for Problems of Family Health and Human Reproduction. 664003, Russia, Irkutsk, Timirjazeva str. 16. Tel.: +73952209440. E-mail: atalyan@sbamsr.irk.ru
For citation: Leshchenko O.Ya., Malanova A.B., Atalyan A.V. An operational study of the effectiveness of early diagnosis in female reproductive disorders associated with genital tuberculosis. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2019; (1): 98-102. (in Russian)
http: // dx.doi.org/10.18565/aig.2019.1.98-102