Sucking reflex and the effectiveness of enteral nutrition in neonates during the first months of life
Aim. To investigate the effectiveness of sucking in preterm newborns during the transition from tube to oral feeding (breast or bottle) and to substantiate the principles of creating computer software for an objective assessment of the sucking reflex.Ryumina I.I., Borovikov P.I., Narogan M.V., Kukhartseva M.V., Lagutin V.V., Orlovskaya I.V., Zubkov V.V., Degtyarev D.N.
Materials and methods. The development of sucking activity was examined in 105 infants born at 25–31 weeks, divided into three groups categorized by the severity of respiratory disorders. The study included the development of computer software for non-invasive visual analysis of sucking effectiveness in newborns.
Results. The analysis involved examining the association between timing of the onset of sucking, discontinuation of tube feeding, and severity of respiratory disorders. The presence of moderate and severe bronchopulmonary dysplasia significantly prolonged the transition from tube to oral feeding. An objective method using sucking pattern recognition software was developed to assess sucking effectiveness.
Conclusion. The developed software allows for a quantitative objectified assessment of the movements of various parts of the newborn’s face during sucking. Once verified and validated, the method can objectively assess sucking in neonates of different gestational ages.
Keywords
Breastfeeding plays a crucial role in the growth and development of babies and determines their future health. Besides the unique properties of breast milk, the process of sucking at the breast is one of the factors responsible for the correct development of the maxillofacial structures and the speech apparatus. The breastfed newborn cries less and sleeps better, has higher motor activity and is less likely to have intestinal colic. Breastfeeding promotes the emotional relationship between mother and infant and is associated with better intellectual and motor development.
Sucking behavior in preterm infants reflects the baby's neurobehavioral and whole body maturation [1, 2]. The ability to maintain vital functions such as heart and respiration rate, oxygen saturation is of great importance for preventing hypoxia, bradycardia, and respiratory distress during feeding [3, 4].
Effective suck-swallow-breathe coordination is an essential skill that in term infants is seen as a sign of maturation and neurodevelopmental stability. Poor sucking reflexes due to morphofunctional immaturity or poor general condition make it difficult to initiate breastfeeding or bottle-feeding for preterm infants. They are fed through a tube, which allows the infant to get milk without having to suck and swallow.
The ability to suck effectively also depends on the rate at which the full volume of oral feeding is achieved, which, in turn, is determined by many factors, such as the duration of mechanical ventilation or other types of respiratory support, oral feeding tolerance, and the time of the feeding intervals [5]. However, the effectiveness of sucking in clinical practice is assessed, as a rule, subjectively. It depends not only on the child's ability to suck independently but also on the experience of the mother or health care team caring for the child. The existing methods for assessing sucking activity are either too subjective or rather complicated, requiring special equipment and training [6, 7].
This study aimed to investigate the effectiveness of sucking in preterm newborns during the transition from tube to oral feeding (breast or bottle) and to substantiate the principles of creating computer software for an objective assessment of the sucking reflex.
Materials and methods
The study analyzed sucking patterns in extremely preterm infants in the natural physiological nursing setting without oral stimulation and nootropic agents. The study included 105 extremely low gestational age (GA) infants born at 25–31 weeks’ gestation with very and extremely low birth weight. Children with hereditary metabolic disorders, endocrine diseases, severe hemolytic disease, and congenital malformations requiring surgical intervention were not included in the study.
One of the main factors affecting the attainment of full oral feeding, development of sucking reflex, and effective sucking was the presence and severity of respiratory disorders, the duration of invasive mechanical ventilation, and long-term dependence on high supplementary oxygen concentrations.
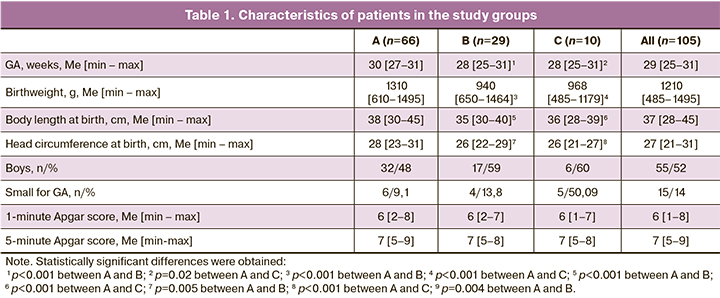
All patients included in the study had respiratory disorders due to lung immaturity (respiratory distress syndrome) and congenital pneumonia, which required respiratory support using various techniques, including high-frequency mechanical ventilation. All patients were divided into three groups categorized by the severity of respiratory disorders. Group A (n=66) included infants with respiratory disorders but without bronchopulmonary dysplasia (BPD). Babies in group B (n=29) had mild and in group С (n=10) moderate to severe BPD, respectively (Table 1).
As part of the study, we developed a new non-invasive method for visually analyzing newborns' sucking effectiveness. It uses a specially designed computer algorithm for recognizing the movements of a newborn's cheekbones, cheeks, and lips on a mobile phone. The software allows real-time assessment of newborns' sucking and including changes in its effectiveness. The research protocol involved the mother's informed consent on the recording, which was done, as a rule, in her presence. For simplicity of designation, this approach was called "Computer vision."
Algorithms for processing mobile phone recordings were developed for capturing, modifying. Primary processing of video data, methods for tracking an object on the video were adapted as applied to arbitrary movements of a child in a frame, algorithms for recognizing a child's face based on open annotated data were developed, encoded primary facial models for determining reference points on the child's face (cheekbones, cheeks, lips, chin). The current accuracy of recognizing a child's face in the videos was 0.7 in the lateral view, 0.95 in the anterior view (the number of frames in which the system was able to recognize a face). Based on the video data analysis of pattern recognition and computer vision, the main methods of face recognition used in the field of computer vision were identified. On some of the data, the existing libraries of annotated images of the adult face in the lateral and anterior view were tested, which showed satisfactory results on newborns' videos. Of the initial 100 video recordings from mobile phone cameras, 61 (61 video files) were used; the length of recordings ranged from 15 seconds to 1 minute.
Statistical analysis
Statistical analysis was performed using Microsoft Excel spreadsheets and IBM SPSS Statistics version 23 (USA) statistical software. The groups were compared using nonparametric tests. Quantitative variables were reported as the median and minimum, and maximum values (Me [min – max]). Pairwise comparison of the study groups was carried out. The Fisher's test and the Mann-Whitney test were used to assess the differences between the two groups of patients. Correlation between two quantitative variables was analyzed using Kendall's correlation coefficient. Differences were considered statistically significant at p <0.05.
Results and discussion
Table 1 shows the characteristics of children included in the study and divided into three groups categorized by the duration and severity of respiratory disorders. Groups B and C differed from group A in terms of GA and the main anthropometric parameters at birth (birth weight, body length, head circumference): the less GA and body weight/length were, the more prolonged respiratory disorders were observed, complicated by BPD, the degree of which was also depended on the child maturity.
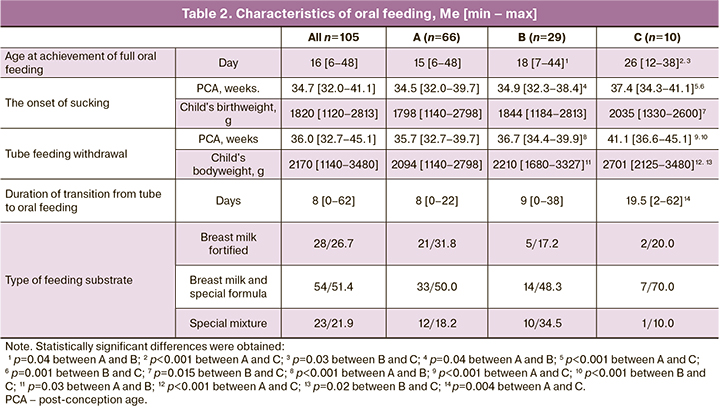
Table 2 presents an analysis of the age at the achievement of full oral feeding, the type of feeding substrate, the time of the onset of sucking and the tube feeding withdrawal, the duration of the transition from tube to feeding on a bottle with a nipple, categorized by the severity of BPD (groups A, B, C). The timing of the onset of sucking and tube feeding withdrawal was significantly associated with oxygen therapy duration. The more prolonged oxygen therapy was required, the later the baby began to suck from the nipple, and the later the tube feeding was discontinued.
All very preterm infants who did not require oxygen therapy after 28 days of life achieved oral feeding before PCA of 40 weeks, with an average of 34.7 weeks. Babies with mild BPD began to suckle a few days later, and on average, tube feeding was discontinued a week later. The age at which tube feeding was started and tube feeding was canceled in children with moderate and severe BPD were significantly greater than in groups A and B. Thus, in children with BPD, the age at tube feeding withdrawal depended on the disease's severity. They began to suck from the nipple later due to insufficient suck-swallow-breathe coordination against the background of respiratory failure, oxygen desaturation, apnea, and bradycardia. The transition from tube to oral feeding was also longer in group B than in the other groups. This is explained by the persisting decrease in oxygen saturation and increased respiratory failure during sucking in children with BPD.
Given the later onset of oral feeding, babies with BPD were already getting larger when it was possible to stop tube feeding. The withdrawal of tube feeding, on average, occurred when the body weight of the children was 2094, 2210, and 2701 g in groups A, B, and C, respectively.
There were no significant statistical differences in the type of feeding; basically, the children were on mixed feeding, and 31.8% of them received only fortified breast milk without the use of infant formula (Table 2).
Tube feeding was discontinued between weeks 36 and 45 of PCA. The duration of the transition from tube to oral feeding was characterized by pronounced individual variability and was not associated significantly with body weight. There was a weak negative correlation between body weight and PCA (r = -0.19, p <0.05). In group A and group B, a statistically significant positive correlation was obtained between the age at full oral feeding and tube feeding withdrawal.
Our results suggest that the effectiveness of sucking in extremely preterm infants depends on the respiratory function and maturity, which is determined by GA, PCA, and individual developmental characteristics, such as suck-swallow-breathe coordination, sucking force, the formation of sleep-wake cycles. Moreover, the sucking efficiency did not directly depend on the child's body weight. It is known that suck-swallow-breathe coordination begins to appear at 32 weeks and improves by 40 weeks. In our study, children who had a relatively rapid increase in the amount of food started feeding on the nipple earlier. However, tube feeding withdrawal and the transition to full oral feeding occurred at the same time as in children with a slower increase in oral feeding volume. This observation suggests a more significant influence of the rate of central nervous system maturation on the ability to suck in preterm infants [8].
All breastfeeding mothers were encouraged to bring the preterm baby to the breast from the moment of effective sucking. However, only two children in group A switched to full breastfeeding at the hospital stage. At the time of hospital discharge, the rest of the children still needed full or supplemental bottle feeding, and this was determined not only by the need to fortify breast milk. It should be noted that the assessment of bottle and breastfeeding effectiveness is mostly subjective and depends on the experience of the nurse or mother, as well as the time of feeding session, time of day, and other factors.
The existing methods for assessing the quality of sucking have both advantages and disadvantages. Most of the techniques have been used for a long time and are subjective. Several objective assessment methods are either expensive, such as a sensorized pacifier, or require the assessment of a specially trained healthcare professional [7, 9, 10]. One of the most convenient and accessible methods for diagnosing impaired sucking function in infants, including premature babies, is the Neonatal Oral-Motor Assessment Scale (NOMAS) for assessment of the coordination of the sucking, swallowing, and breathing sequence, as well as movements of the mandible and tongue [11, 12]. This scale is a non-invasive convenient to use tool, making it possible to track the development of sucking skills, both during breastfeeding and when feeding on a bottle with a nipple. At the same time, some parts of the NOMAS scale are subjective, and the results depend on the individual interpretation, which was proven by the Dutch working group, which identified seven different interpretations of the NOMAS parameters [13]. This group of experts introduced new assessment guidelines, and this revision improved the inter-rater reliability of the NOMAS in the diagnosis of sucking dysfunction [14].
 The proposed image recognition method (computer vision) is non-invasive, objective, and effective in obtaining data, does not require expensive equipment, and allows for storing the received information. It was designed based on computer vision and the Lucas Kanade motion analysis algorithm, enabling detecting the stream of an arbitrary number of points of interest in the video. An archive of 61 nutritional and non-nutritional sucking videos was used with various lighting conditions, baby positions, and shooting angles. Applying this approach to videos with newborns during non-nutritive and nutritive sucking, the proposed system calculates each point of interest's absolute motion vectors, thereby tracking the intensity of movement of the baby's cheekbones, lips, larynx, and cheeks. The system receives a stabilized image of the baby during sucking with points of interest marked on the baby's face. The points were selected using the NOMAS method, according to which the intensity/frequency of cheekbone and tongue movements, swallowing, and sucking rhythm are the qualitative indicators of sucking activity. All these parameters relate to quantitative factors characterizing the sucking reflex and are analyzed by visual observation of specific parts of the newborn's face. To determine these parameters, the points are selected in such a way as to involve the zones of the jaws, lips, and cheekbones of the newborn. An example of marking is shown in Figure 1. The system collects data on the intensity of indirect signs of sucking in an infant, observing muscles' movement involved in sucking. By normalizing and removing unnecessary "noise" from the collected data, the system produces graphs of the desired points' frequency and amplitude of motion.
The proposed image recognition method (computer vision) is non-invasive, objective, and effective in obtaining data, does not require expensive equipment, and allows for storing the received information. It was designed based on computer vision and the Lucas Kanade motion analysis algorithm, enabling detecting the stream of an arbitrary number of points of interest in the video. An archive of 61 nutritional and non-nutritional sucking videos was used with various lighting conditions, baby positions, and shooting angles. Applying this approach to videos with newborns during non-nutritive and nutritive sucking, the proposed system calculates each point of interest's absolute motion vectors, thereby tracking the intensity of movement of the baby's cheekbones, lips, larynx, and cheeks. The system receives a stabilized image of the baby during sucking with points of interest marked on the baby's face. The points were selected using the NOMAS method, according to which the intensity/frequency of cheekbone and tongue movements, swallowing, and sucking rhythm are the qualitative indicators of sucking activity. All these parameters relate to quantitative factors characterizing the sucking reflex and are analyzed by visual observation of specific parts of the newborn's face. To determine these parameters, the points are selected in such a way as to involve the zones of the jaws, lips, and cheekbones of the newborn. An example of marking is shown in Figure 1. The system collects data on the intensity of indirect signs of sucking in an infant, observing muscles' movement involved in sucking. By normalizing and removing unnecessary "noise" from the collected data, the system produces graphs of the desired points' frequency and amplitude of motion.
The development of the analysis technique logically consists of marking the original image, choosing points of interest on the newborn's face, stabilizing the video, tracking each point's movements by frame during sucking, recognizing the trend and seasonality in the received signal, and identifying signal characteristics. Since the collected data contains images of newborns in various poses with a partially covered face and data with different picture quality, automated systems for recognizing and marking faces turned out to be poorly applicable in this task. It was therefore decided to mark up the presented videos for more accurate analysis manually. The image markup interface was made using computer vision methods using the Python programming language. This marking is performed on the first frame of the video, which imposes restrictions on shooting quality. The marking takes place in accordance with the developed recommendations, points of interest are highlighted on the child's chin, on the cheekbones, and cheeks, and one reference point is mandatory, from which the movement of the rest is calculated. The marked image is automatically stabilized for a more accurate determination of the distance between points.
Video motion analysis takes place in two stages:
I. Two adjacent video frames are compared by the Lucas Kanade algorithm to detect the optical flow between frames, thereby tracking the movement of selected points in the video [15–17].
II. For each point, the distance from the fixed reference point is calculated on each frame, and the distance vector is recorded in the resulting table.
The result of the algorithm is an array of distances for each point of interest, reflecting the relative movement of each point and the corresponding part of the newborn's face. The data are entered into a table, which is a discrete motion estimate for each channel. Specific characteristics of the sucking activity of each newborn were identified by statistical analysis, which consisted of the following steps:
1. The distance vector was normalized to the mean.
2. The time series analysis was performed to identify its structure and components of seasonality and trend.
3. Assuming that the movements of the points of interest are periodic and occur with their amplitude and frequency parameters, we analyze the seasonality component in the decomposition of the original signal to identify the specifics of the movements.
As a result, we have an array of values for each point, including the distances from the fixed benchmark, which is an absolute indicator of the movement of the corresponding points on the face of the newborn. For a numerical comparison of the received data for each channel-point, the received signal is analyzed; an example of such a signal is shown in Figure 2. The motion data were decomposed into three critical components for further analysis: trend vector, seasonality vector (periodic function), error vector.
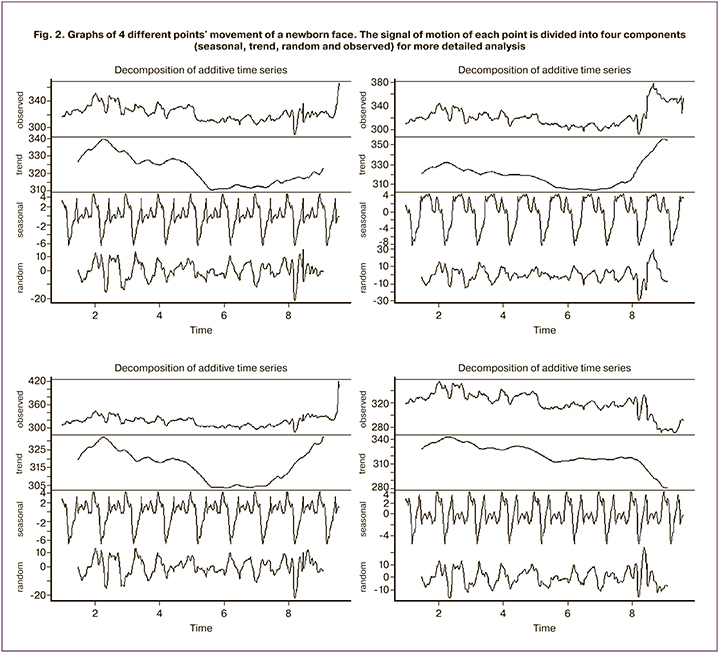
The phase of a newborn sucking activity was determined by searching for local maximum and minimum according to the initial signal (the first graph in the figure) for each time interval. The relative amplitude and frequency of sucking movements were calculated at a high density of the found "peaks," indicating an active reciprocating motion. The length of the constant frequency segments indicates the rhythm of the sucking movements. These indicators were used for comparable quantitative analysis of sucking movements. After processing 30 records of sufficient quality, for each of which the points of interest were marked, and the movement of these points was analyzed, the motion track of the selected points was recorded. The values of the amplitude and frequency of the seasonal component were calculated.
The relationship between sucking pattern in the neonatal period and further neurological development, the importance of detailed assessment in the diagnosis of sucking disorders for each individual parameter, has been confirmed in many studies [18–21]. The question remains open at what age does the inconsistency of sucking movements and the inability to maintain the sucking process reflect the normal development of the central nervous system and the child's body as a whole, and at what age it signals severe neurological disorders. Besides, further research is needed to understand the mechanisms of coordination of the sucking, swallowing, and breathing sequence during the maturation of a preterm baby's body.
Disorders of the sucking reflex and dyscoordination of the sucking, swallowing, and breathing sequence can be caused by respiratory diseases in BPD. Preterm babies with mild BPD, or small for GA, as a rule, have more difficulties associated with the formation of neurobehavioral functions than children with normal anthropometric parameters for GA and without BPD [22]. Wolthuis-Stigte et al. (2014) found that deviations in the periodicity and parameters of sucking skills according to NOMAS can be associated with disorders of psychomotor development [19].
Conclusion
The developed software allows for a quantitative objectified assessment of the movements of various parts of the newborn's face during non-nutritive and nutritive sucking. The findings correlate with the subjective visual assessment of sucking. Once verified and validated, the method can be used to evaluate suckling in neonates of different gestational ages and comparative analysis of various feeding methods.
References
- Lau C., Smith E.O., Schanler R.J. Coordination of suck-swallow and swallow respiration in preterm infants. Acta Paediatr. 2003; 92(6): 721-7.
- Pickler R.H., Best A., Crosson D. The effect of feeding experience on clinical outcomes in preterm infants. J. Perinatol. 2009; 29(2): 124-9. https://doi.org/10.1038/jp.2008.140.
- Hasenstab K.A., Nawaz S., Lang I.M., Shaker R., Jadcherla S.R. Pharyngoesophageal and cardiorespiratory interactions: Potential implications for premature infants at risk of clinically significant cardiorespiratory events. Am. J. Physiol. Gastrointest. Liver Physiol. 2019; 316(2): G304-12. https://doi.org/10.1152/ajpgi.00303.2018.
- Pineda R., Prince D., Reynolds J., Grabill M., Smith J. Preterm infant feeding performance at term equivalent age differs from that of full-term infants. J. Perinatol. 2020; 40(4): 646-54. https://doi.org/10.1038/s41372-020-0616-2.
- Chu E., Freck S., Zhang L., Bhakta K.Y., Mikhael M. Three-hourly feeding intervals are associated with faster advancement in very preterm infants. Early Hum. Dev. 2020; 131: 1-5. https://doi.org/10.1016/j.earlhumdev.2019.01.021.
- Mizuno K., Aizawa M., Saito S., Kani K., Tanaka S., Kawamura H., Hartmann P.E., Doherty D. Analysis of feeding behavior with direct linear transformation. Early Hum. Dev. 2006; 82(3): 199-204. https://doi.org/10.1016/j.earlhumdev.2005.08.002.
- Miller J.L., Kang S.M. Preliminary ultrasound observation of lingual movement patterns during nutritive versus non-nutritive sucking in a premature infant. Dysphagia. 2007; 22(2): 150-60. https://doi.org/ 10.1007/s00455-006-9058-z.
- Нароган М.В., Рюмина И.И., Кухарцева М.В., Грошева Е.В., Ионов О.В., Тальвирская В.М., Лазарева В.В., Зубков В.В., Дегтярев Д.Н. Практический опыт применения клинических рекомендаций «Энтеральное вскармливание недоношенных детей». Акушерство и гинекология. 2018; 9: 106-14. [Narogan M.V., Ryumina I.I., Kukhartseva M.V., Grosheva E.V., Ionov O.V., Talvirskaya V.M., Lazareva V.V., Zubkov V.V., Degtyarev D.N. Practical experience in the application of clinical guidelines "Enteral feeding of premature babies". Akusherstvo i ginekologiya/Obstetrics and gynecology. 2018; 9: 106-14. (in Russian)]. https://doi.org/https://dx.doi.org/10.18565/aig.2018.9.106-114.
- AWHONN. Breastfeeding. J. Obstet. Gynecol. Neonatal Nurs. 2015; 44(1): 145-50. https://doi.org/10.1111/1552-6909.12530.
- AWHONN. Systematic assessment of the infant at the breast (SAIB). Washington DC; 1989.
- Palmer M., Crawley K., Blanco I. Neonatal oral-motor assessment scale: a reliability study. J. Perinatol. 1993; 13(1): 28-35.
- Palmer M. Identification and management of the transitional suck pattern in premature infants. J. Perinat. Neonatal Nurs. 1993; 7(1): 66-75. https://doi.org/10.1097/00005237-199306000-00009.
- da Costa S.P., van den Engel-Hoek L., Bos A.F. Sucking and swallowing in infants and diagnostic tools. J. Perinatol. 2008; 28(4): 247-57. https://doi.org/10.1038/sj.jp.7211924.
- da Costa S.P., Hübl N., Kaufman N., Bos A.F. New scoring system improves inter-rater reliability of the Neonatal Oral-Motor Assessment Scale. Acta Paediatr. 2016; 105(8): e339-44. https://doi.org/10.1111/apa.13461.
- Ahmine Y., Caron G., Mouaddib El. M., Chouireb F. Adaptive Lucas-Kanade tracking. Image Vis. Comput. 2019; 88: 1-9. Available at: https://hal.archives-ouvertes.fr/hal-02193928
- Yilmaz A., Javed O., Shah M. Object tracking: A survey. ACM Comput. Surv. 2006; 38(4):1-45.
- Mohiuddin K., Alam M.M., Das A.K., Munna T.A., Allayear S.M., Ali H. Haar cascade classifier and Lucas–Kanade optical flow based realtime object tracker with custom masking technique. In: Arai K., Kapoor S., Bhatia R., eds. Advances in information and communication networks. Springer; 2019:398-410.
- Nieuwenhuis T., da Costa S.P., Bilderbeek E., Geven W.B., van der Schans C.P., Bos A.F. Uncoordinated sucking patterns in preterm infants are associated with abnormal general movements. J. Pediatr. 2012; 161(5): 792-8. https://doi.org/10.1016/j.jpeds.2012.04.032.
- Wolthuis-Stigter M.I., Luinge M.R., da Costa S.P., Krijnen W.P., van der Schans C.P., Bos A.F. The association between sucking behavior in preterm infants and neurodevelopmental outcomes at 2 years of age. J. Pediatr. 2015; 166 (1): 26-30. https://doi.org/10.1016/j.jpeds.2014.09.007.
- Medoff-Cooper B., Shults J., Kaplan J. Sucking behavior of preterm neonates as a predictor of developmental outcomes. J. Dev. Behav. Pediatr. 2009; 30(1): 16-22. https://doi.org/10.1097/DBP.0b013e318196b0a8.
- Tsai S.W., Chen C.H., Lin M.C. Prediction for developmental delay on Neonatal Oral Motor Assessment Scale in preterm infants without brain lesion. Pediatr. Int. 2010; 52(1): 65-8. https://doi.org/10.1111/j.1442-200X.2009.02882.x.
- Da Costa S.P., van der Schans C.P., Zweens M.J., Boelema S.R., van der Meij E., Boerman M.A., Bos A.F. The development of sucking patterns in preterm, small-for-gestational age infants. J. Pediatr. 2010; 157(4): 603-9. https://doi.org/10.1016/j.jpeds.2010.04.037.
Received 16.09.2020
Accepted 02.11.2020
About the Authors
Irina I. Ryumina, Dr. Med. Sci., Head of the Department of Pathology of Newborns and Preterm Infants, V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia.Tel.: +7(903)770-80-48. E-mail: i_ryumina@oparina4.ru, i.ryumina@mail.ru. ORCID: 0000-0003-1831-887X. 117997, Russia, Moscow, Ac. Oparina str., 4.
Pavel I. Borovikov, PhD (Math. Sci.), Head of the Bioinformatics Laboratory, V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia.
Tel.: +7(919)109-12-64. E-mail: p_borovikov@oparina4.ru. ORCID: 0000-0003-4880-7500. 117997, Russia, Moscow, Ac. Oparina str., 4.
Marina V. Narogan, Dr. Med. Sci., Leading Researcher at the Department of Pathology of Newborns and Preterm Infants, V.I. Kulakov NMRC for OG&P,
Ministry of Health of Russia; Professor at the Department of Neonatology, I.M. Sechenov First MSMU, Ministry of Health of Russia (Sechenov University). Tel.: +7(905)550-16-21.
E-mail: m_narogan@oparina4.ru. ORCID: 0000-0002-3160-905X. 117997, Russia, Moscow, Ac. Oparina str., 4; 119991, Russia, Moscow, Trubetskaya str., 8-2.
Marina V. Kukhartseva, Neonatologist, Researcher at the Department of Pathology of Newborns and Preterm Infants of the Institute of Neonatology and Pediatrics,
V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia. Tel.: +7(903)551-95-55. E-mail: m_kukhartseva@oparina4.ru; kolibry90@list.ru. ORCID: 0000-0002-4916-9531.
117997, Russia, Moscow, Ac. Oparina str., 4.
Vadim V. Lagutin, Researcher of Laboratory of Bioinformatics, V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia.
Tel.: +7(916)622-57-57. E-mail: laggi@mail.ru. ORCID: 0000-0001-7536-0631. 117997, Russia, Moscow, Ac. Oparina str., 4.
Irina V. Orlovskaya, Ph.D., Senior Researcher, Clinical Care Supervisor at the Department of Pathology of Newborns and Preterm Infants of the Institute of Neonatology and Pediatrics, V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia. Tel.: +7(916) 696-20-56. E-mail: i_orlovskaya@oparina4.ru. ORCID: 0000-0001-9565-5760.
117997, Russia, Moscow, Ac. Oparina str., 4.
Viktor V. Zubkov, MD, Director of the Institute of Neonatology and Pediatrics, V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia; Professor of the Department
of Neonatology, I.M. Sechenov First MSMU, Ministry of Health of Russia (Sechenov University). Tel.: +7(963)750-48-77. E-mail: v_zubkov@oparina4.ru,
victor.zubkov@mail.ru. ORCID: 0000-0001-8366-5208. 117997, Russia, Moscow, Ac. Oparina str., 4; 119991, Russia, Moscow, Trubetskaya str., 8-2.
Dmitriy N. Degtyarev, Dr. Med. Sci., Professor, Deputy Director for Research, V.I. Kulakov NMRC for OG&P, Ministry of Health of Russia; Head of the Department
of Neonatology, I.M. Sechenov First MSMU, Ministry of Health of Russia (Sechenov University); Chairman of the Ethics Committee of the Russian Society of Neonatologists, Moscow, Russia. Tel.: +7(926)007-26-30. E-mail: d_degtiarev@oparina4.ru. ORCID: 0000-0001-8975-2425.
117997, Russia, Moscow, Ac. Oparina str., 4; 119991, Russia, Moscow, Trubetskaya str., 8-2.
For citation: Ryumina I.I., Borovikov P.I., Narogan M.V., Kukhartseva M.V., Lagutin V.V., Orlovskaya I.V., Zubkov V.V., Degtyarev D.N. Sucking reflex and the effectiveness of enteral nutrition in neonates during the first months of life.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2021; 2: 105-112 (in Russian)
https://dx.doi.org/10.18565/aig.2021.2.105-112