Assessment of risks for bleeding during preterm labor from the causes of bleeding
Objective. To study the possibilities of predicting the risks of abnormal and massive blood loss during preterm labor on the basis of the causes of bleeding.Novikova V.A., Kamenskikh G.V., Olenev A.S., Levakov S.A., Lebedeva M.G., Apresyan S.V., Gagyaev Ch.G., Duhin A.O., Kostin I.N., Soyunov M.A., Semyatov S.M., Startseva N.M.
Material and methods. The authors carried out a prospective analysis of 1442 deliveries complicated by bleeding. Discriminant analysis was made to classify intergroup differences in the presence of abnormal and massive blood loss and in the absence of bleeding during preterm and term labor.
Resu1ts. The relative risk of abnormal or massive blood loss on the basis of the causes of bleeding in preterm labor; the signs determining intergroup differences in the presence of abnormal and massive blood loss and in the absence of bleeding during preterm and term labor; and the signs indicating the risks of hypotonic bleeding were assessed.
Conclusion. Preterm labor is threatened by abnormal and massive blood loss. The structure of the main causes of abnormal and massive blood loss is different in preterm and term labor, which leaves a resource to choose preventive and therapeutic measures.
Keywords
Obstetric hemorrhage complicates about 14 million births per year in the world [1], and despite global measures to prevent them, they remain an irresistible threat to maternal health and life [2, 3]. According to the criteria of the World Health Organization (WHO), severe postpartum hemorrhage (PPH) refers to potentially life-threatening conditions [4]. To date, an absolutely effective way of preventing PPH and severe outcomes resulting from PPH has not been found. Direct obstetric causes compose 73% of maternal deaths, the share of obstetric bleeding is 27.1% [5].
In 2015, WHO declared the Millennium Development Goals. Eight main directions were presented, one of which is improving maternal health [6].
Modern approaches to the diagnosis and treatment of obstetric hemorrhage are based not only on assessing the volume of blood loss, but also understanding its etiopathogenesis, which determines various approaches to the choice of prophylactic and therapeutic measures [7]. PPH may be severe and profuse as it is generally due to a combination of several causes.
More recent attention in literature has focused on full-term pregnancy in terms of PPH. However, the frequency of preterm labor (PL) in the world remains high, ranging from 5% to 18% of the total number of children born [8] and the relative risk (RR) of significant PPH with fetus weight <2 kg and > 4 kg can be comparable (PR = 1.55 (95% CI 1.31–1.83, p <0.0001) versus OR = 1.22 (95% CI 1.12– 1.32, p <0.0001) [9].
According to literary databases of Russian Science Citation Index, Federal Electronic Medical Library, eLibrary, EMBASE, PubMed, MEDLINE, Cochrane Library (Cochrane Review), Elsevier platform, BioMed Central, OVID interactive database for the period 2013-2018, there are no multicenter studies comparing the variety of the main causes, the possibility of predicting PPH during PL.
The objective of the research is to study the possibilities of predicting the risks of abnormal and massive blood loss during preterm labor on the basis of the causes of bleeding.
Materials and Methods
This study was carried out in the period 2013–2017 in the perinatal center of Regional Clinical Hospital No. 2 of the Department of Health, the Krasnodar Territory.
The prospective analysis of 17656 births was performed, 1442 of them were complicated by bleeding. The basic criteria for inclusion in the main and comparative groups were childbirth and obstetric bleeding. Exclusion criteria were the presence of genetically determined pathology of hemostasis, preeclampsia, diabetes mellitus, extragenital pathology in the decompensation stage, which can competitively affect the volume of blood loss.
Three clinical groups were formed, namely, main, comparison and control groups. The main group consisted of women with PL (n = 412) and massive blood loss (PL_MBL, n = 48) or abnormal blood loss (PL_ABL, n = 364); comparison group included patients with full-term labor (TL, n = 1030) and massive blood loss (TL_MBL, n = 130) or abnormal blood loss (TL_ABL, n = 900); control group included women without bleeding (n = 16214) with preterm labor (PL_Control, n = 698) and delivery on time (TL_Control, n = 15516).
The study was carried out in accordance with federal clinical guidelines (treatment protocol) “Prevention, treatment and management algorithm for obstetric hemorrhages” [7]. For statistical analysis of the results of the study we used the statistical package Statistica 12.0, Microsoft Excel 2007. Parameters of descriptive statistics were calculated. Taking into account the non-normal trait of some parameters, the median (Me), lower (Q1) and upper (Q3) quartiles were used for descriptive statistics. To assess the risk of an outcome with a particular risk factor, the relative risk (RR) was calculated with 95% confidence interval (CI). In order to interpret intergroup differences, discriminant analysis (DA) was used as a method of statistical classification. Wilk's Lambda, Partial Lambda, F-remove, Tolerance (Toler.) were calculated. Based on the calculation of the systems of linear equations, which suggest that certain indicators belong to the group under study, prognostic models of DA were obtained. Example of an equation: Group (N) = k1 * parameter 1 + k2 * parameter2 ……. + k3 * parameter3 - Constant. The most probable forecast is in the group for which the value of Group (N) will be the highest.
Results
During the period of this study, the number of births at the Perinatal Center was 42105 (8161-9140 per year), 3020 (7.17%) of which were premature. The total number of births complicated by bleeding was 3909 (9.28%); the number of PL was 1118, which was 2.66% of the total number of births and 37% of the number of PL. Massive blood loss occurred in 430 (1.02%) cases of the total number of births, in 123 (4.07%) cases of the number of PL and in 307 (0.7%) cases of the number of full-term births.
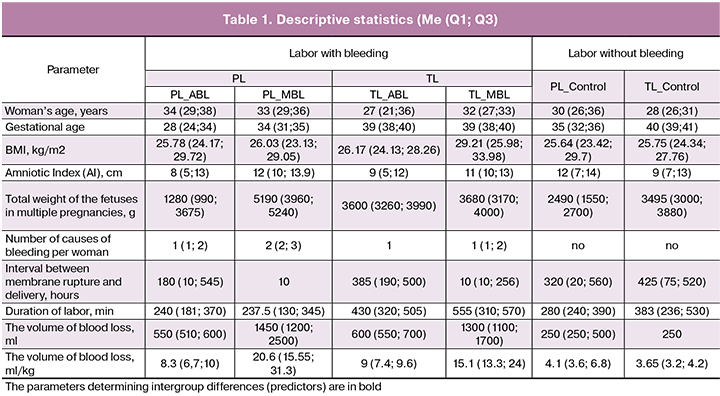
The age of the women included in the study ranged from 18 to 46 years (Me = 31; Q1 = 27; Q3 = 36), body mass index (BMI) in the preconception period was 19.33-53.07 kg/m2 (Me = 26.17; Q1 = 24.13; Q3 = 29.7). The gestation age during delivery was 22–41 weeks (Me = 36; Q1 = 32; Q3 = 39); blood loss was 200–8000 ml (Me = 725; Q1 = 500; Q3 = 1300) (Table 1).
For PL, the relative risk (RR) of abnormal or massive bleeding due to various causes in comparison with PL without bleeding (control group) was calculated (Table 2).

For preterm and full-term labor, prognostically significant signs that determine intergroup differences in case of abnormal or massive blood loss and in the absence of bleeding are established: the number of scars on the uterus, the number of causes of bleeding per woman, BMI, the total weight of the fetuses during a multiple pregnancy, interval between membrane rupture and delivery, the duration of labor (Table 1).
These predictors allowed us to classify outcomes (abnormal, massive blood loss, no bleeding) in premature and full-term labor with the help of discriminant analysis (Table 3). It is possible to calculate using the discriminant equations which group (Group (N)) the outcome will refer to. An example of the calculation of the discriminant equation: Group (N) = Coefficient * Parameter + Constant. For example, for BMI = 30, the value of the equation for the group PL_MBL = 16.03; for the group PL_ABL = 15.66; for the group TL_MBL = 15.1; TL_ABL = 15.14; for the group TL _ Control = 15.31; for the group PL_Control= 15.49. So BMI = 30 is most predictable for massive blood loss in PL_MBL.
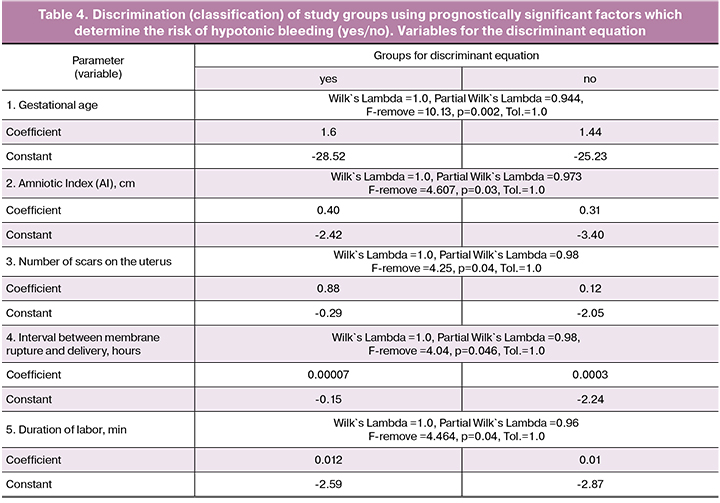
Similar results were obtained to predict hypotonic bleeding (yes/no). Table 4 presents the parameters critically separating (discriminating) labor, complicated by hypotonic bleeding (yes) or not complicated (no).
Conclusion
Preterm labor is threatened by abnormal and massive blood loss. The main causes of massive blood loss with PL are premature detachment of a normally located placenta, placenta previa, hypotonic bleeding. The signs that determine intergroup differences in abnormal, massive blood loss and in the absence of bleeding during premature and full-term labor are the number of scars on the uterus, the number of causes of bleeding per woman, BMI, the total weight of the fetuses during multiple pregnancies, the duration of interval between membrane rupture and delivery, the duration of labor. The signs that determine intergroup differences in the risk of hypotonic bleeding are the gestational age, the amniotic fluid index, the number of scars on the uterus, the duration of interval between membrane rupture and delivery, the duration of labor. The data obtained suggest that the main causes of abnormal and massive blood loss in preterm and full-term labor are different which may affect the choice of preventive and therapeutic measures.
References
- World Health Organization. Priority diseases and reasons for inclusion. Postpartum haemorrhage. Available at: http://www.who.int/medicines/areas/priority_medicines/Ch6_16PPH.pdf Accessed: October, 2018.
- Серов В.Н., Сухих Г.Т., ред. Клинические рекомендации. Акушерство и гинекология. 4-е изд. М.: ГЭОТАР-Медиа; 2015. 1024с. [Serov V.N., Sukhikh G.T. Obstetrics and gynecology. Clinical guidelines. 4th ed., Rev. and add. M.: GEOTAR-Media; 2015. 1024s. (in Russian)].
- Радзинский В.А., Фукс А.М., ред. Акушерство. Учебник. М.: ГЭОТАР-Медиа; 2016. 1040с. [Radzinskij V.A. Obstetrics: a textbook / ed. V. E. Radzinsky, A. M. Fuchs. M.: GEOTAR-Media; 2016. 1040 s. (in Russian)].
- Witteveen T., Bezstarosti H., de Koning I., Nelissen E., Bloemenkamp K.W., van Roosmalen J. et al. Validating the WHO maternal near miss tool: comparing high- and low-resource settings. BMC Pregnancy Childbirth. 2017; 17(1): 194.
- Say L., Chou D., Gemmill A., Tunçalp Ö., Moller A.B., Daniels J. et al. Global causes of maternal death: a WHO systematic analysis. Lancet Glob. Health. 2014; 2(6): e323-33.
- Millennium Development Goals (MDGs). WHO; 2015. Available at: http://www.who.int/topics/millennium_development_goals/about/en/) Accessed: October, 2018.
- Адамян Л.В., Серов В.Н., Филиппов О.С., Артымук Н.В., Баев О.Р., Башмакова Н.В., Белокриницкая Т.Е., Дробинская А.Н., Ерофеев Е.Н., Кан Е.Н., Малыгина Г.Б., Пырегов А.В., Салов И.А., Тютюнник В.Л., Шмаков Р.Г., Федорова Т.А. Профилактика, лечение и алгоритм ведения при акушерских кровотечениях. Клинические рекомендации (протокол лечения). М.; 2014. 23c. [Adamyan L.V., Serov V.N., Filippov O.S., Artymuk N.V., Baev O.R., Bashmakova N.V., Belokrinitskaya T.E., Drobinskaya A.N., Erofeev E.N., Kan E.N., Malygina G.B., Pyregov A.V., Salov I.A., Tyutyunnik V.L., Shmakov R.G., Fedorova T.A. Prevention, treatment and management algorithm for obstetric hemorrhage. Clinical recommendations (treatment protocol). Moscow. 2014. 23 p. (in Russian)]
- Информационный бюллетень ВОЗ от 19 февраля 2018 года. [WHO Newsletter. February 19, 2018]. Available at: http://www.who.int/ru/news-room/fact-sheets/detail/preterm-birth Accessed: October, 2018.
- Al Wattar B.H., Tamblyn J.A., Parry-Smith W., Prior M., Van Der Nelson H. Management of obstetric postpartum hemorrhage: a national service evaluation of current practice in the UK. Risk Manag. Healthc. Policy. 2017; 10: 1-6. doi: 10.2147/RMHP.S121737. eCollection 2017.
Received 01.11.2018
Accepted 07.12.2018
About the Authors
Novikova, Vladislava A., MD, Professor of the Department of Obstetrics and Gynecology with a course in Perinatology, Medical Institute, Federal State Autonomous Educational Institution of Higher Education «Russian University of Peoples Friendship» of the Ministry of Science and Higher Education of the Russian Federation (RUDN). 117198, Russia, Moscow, Miklukho-Maklaya str. 6. Tel.: +74991374881. E-mail: vladislavan@mail.ruKamenskikh, Gayane V., obstetrician-gynecologist of the maternity ward, Perinatal Center, state budgetary health care institution «Regional Clinical Hospital No. 2 of the Krasnodar Territory Health Department». 350012, Russia, Krasnodar, ul. Krasnyh Partizan, 6/2. Tel.: +78612220002. E-mail: pc@kkb2-kuban.ru
Olenev, Anton S., PhD, Associate Professor of the Department of Obstetrics and Gynecology with a course in Perinatology, Medical Institute, Federal State-Autonomous Educational Institution of Higher Education «Russian University of Peoples Friendship» of the Ministry of Science and Higher Education of the Russian Federation (RUDN). 117198, Russia, Moscow, Miklukho-Maklaya str. 6. Chief freelance specialist in obstetrics and gynecology in Moscow, head of the Perinatal Center branch of the City Clinical Hospital No. 24 of the DZM. Tel.: +74956134509. E-mail: olenevAS@zdrav.mos.ru
Levakov, Sergey A., MD, Professor, Head of the Department of Obstetrics and Gynecology, Federal State Autonomous Educational Institution of Higher Education «First Moscow State Medical University named after I.M. Sechenov» Ministry of Health of the Russian Federation.
119146, Russia, Moscow, Bolshaya Pirogovskaya str. 19s1. Tel: +79255063144. E-mail: levakoff@yandex.ru
Lebedeva, Marina G., PhD, Associate Professor of the Department of Obstetrics and Gynecology with a course in Perinatology, Medical Institute, Federal State-Autonomous Educational Institution of Higher Education «Russian University of Peoples’ Friendship» of the Ministry of Science and Higher Education of the Russian Federation.
117198, Russia, Moscow, Miklukho-Maklaya str. 6. Tel.: +74991374881. E-mail: kafedra-aig@mail.ru
Apresyan, Sergey V., MD, Professor of the Department of Obstetrics and Gynecology with a course in Perinatology, Medical Institute, Federal State Autonomous Educational Institution of Higher Education «Peoples’ Friendship University of Russia» of the Ministry of Science and Higher Education of the Russian Federation.
117198, Russia, Moscow, Miklukho-Maklaya str. 6. Tel.: +74991374881. E-mail: kafedra-aig@mail.ru
Gagayev, Chelebi G., MD, Associate Professor of the Department of Obstetrics and Gynecology with a course in Perinatology, Medical Institute, Federal State-Autonomous Educational Institution of Higher Education «Russian University of Peoples’ Friendship» of the Ministry of Science and Higher Education of the Russian Federation.
117198, Russia, Moscow, Miklukho-Maklaya str. 6. Tel.: 74991374881. E-mail: kafedra-aig@mail.ru
Duhin, Armen O., MD, Professor of the Department of Obstetrics and Gynecology with a course in Perinatology, Medical Institute, Federal State Autonomous Educational Institution of Higher Education «Peoples’ Friendship University of Russia» of the Ministry of Science and Higher Education of the Russian Federation.
117198, Russia, Moscow, Miklukho-Maklaya str. 6. Tel.: +74991374881. E-mail: kafedra-aig@mail.ru
Kostin, Igor N., MD, Professor of the Department of Obstetrics and Gynecology with a course in Perinatology, Medical Institute, Federal State Autonomous Educational Institution of Higher Education «Peoples’ Friendship University of Russia» of the Ministry of Science and Higher Education of the Russian Federation.
117198, Russia, Moscow, Miklukho-Maklaya str. 6. Tel.: +74991374881. E-mail: kafedra-aig@mail.ru
Soyunov, Mukhammednazar A., MD, Professor of the Department of Obstetrics and Gynecology with a course in Perinatology, Medical Institute, Federal State Autonomous Educational Institution of Higher Education «Peoples’ Friendship University of Russia» of the Ministry of Science and Higher Education of the Russian Federation.
117198, Russia, Moscow, Miklukho-Maklaya str. 6. Tel.: +74991374881. E-mail: kafedra-aig@mail.ru.
Semyatov, Said M., MD, Professor of the Department of Obstetrics and Gynecology with a course in Perinatology, Medical Institute, Federal State Autonomous Educational Institution of Higher Education «Peoples’ Friendship University of Russia» of the Ministry of Science and Higher Education of the Russian Federation.
117198, Russia, Moscow, Miklukho-Maklaya str. 6. Tel.: +74991374881. E-mail: kafedra-aig@mail.ru.
Startseva, Nadezhda M., MD, Professor of the Department of Obstetrics and Gynecology with a course in Perinatology, Medical Institute, Federal State Autonomous Educational Institution of Higher Education «Peoples’ Friendship University of Russia» of the Ministry of Science and Higher Education of the Russian Federation.
117198, Russia, Moscow, Miklukho-Maklaya str. 6. Tel.: +74991374881. E-mail: kafedra-aig@mail.ru.
For citations: Novikova V.A., Kamenskikh G.V., Olenev A.S., Levakov S.A., Lebedeva M.G., Apresyan S.V., Gagayev Ch.G., Duhin A.O., Kostin I.N., Soyunov M.A., Semyatov S.M., Startseva N.M. Assessment of risks for bleeding during preterm labor from the causes of bleeding. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2019; (2): 78-84. (in Russian)
http://dx.doi.org/10.18565/aig.2019.2.78-84