The role of immunological markers in predicting the course and outcome of pregnancy in patients with isthmic cervical insufficiency
Objective: To investigate the clinical value of cervical canal IL-6, IL-8, and MMP-8 in predicting gestational age at delivery in pregnant women with isthmic cervical insufficiency (ICI). Materials and methods: A prospective cohort study enrolled 60 pregnant women with ICI. Women were divided into 2 groups categorized by gestational age at delivery. Pregnant women in Group 1 (n=23, 38.3%) and Group 2 (n=37, 61.7%) gave birth before and after 32 weeks of gestation, respectively. During vaginal speculum examination, all patients underwent cervical mucus sampling from the cervical canal to determine IL-6, IL-8, and MMP-8 concentrations. Results: In Group 1, the concentration of IL-6, IL-8, and MMP-8 was 12.2 pg/ml, 283.2 pg/ml, and 28.1 ng/ml. In Group 2, the concentration IL-6, IL-8, and MMP-8 was 7.2 pg/ml, 142.4 pg/ml, and 14.6 ng/ml. Correlation analysis between cervical marker levels and gestational age at delivery revealed a strong negative statistically significant correlation for all markers (p<0.001). Linear regression showed association between gestational age at delivery and the concentrations of immunological markers at the time of initial diagnosis of ICI: the higher the level of cervical markers, the higher the risk of spontaneous preterm birth (PB). ROC curve analysis determined the optimal threshold values for each of the markers including IL-6 concentration of 9.6 pg/ml, IL-8 of 195.6 pg/ml, and MMP-8 -of 21.5 ng/ml. Conclusion: Threshold values for IL-6≥9.6 pg/mL, IL-8≥195.6 pg/mL, and MMP-8≥21.5 ng/mL concentrations in the cervical canal can be recommended as predictive of very early and early PB, and are highly likely to be predictors of intraamniotic inflammation/infection regardless of the results of the cervical content culture.Timokhina E.V., Strizhakov A.N., S.V. Pesegova S.V.
Keywords
Early pregnancy loss remains of the most important issues encountered by obstetricians [1, 2]. The worldwide incidence of preterm birth is 11.1% [6], which varies between countries within a range of 5–13% and results in approximately 15 million children born preterm each year [1–5].
One of the main causes of pregnancy loss in the second trimester and early PB is isthmic cervical insufficiency (ICI), which complicates up to 1% of all pregnancies [4, 7, 8].
Despite the high clinical significance of ICI in obstetrics, the methods to assess the real risk of PB with different ICI correction remain poorly understood.
One of the pathogenetic mechanisms of ICI development is impaired barrier function of the cervix and cervical canal and the transmission of intra-amniotic infection/inflammation [2]. Previous studies show that women with ICI experience premature cervical maturation and cervical dilation due to substances involved in inflammatory and immune reactions [8]. Pro-inflammatory cytokines, such as interleukins (IL)-6 and -8, induce the synthesis of prostaglandins that stimulate uterine contractions, cervical softening, and membrane weakening, while anti-inflammatory cytokines, in contrast, prevent these changes [2, 5, 9]. Therefore, immune regulation during pregnancy is important to maintain an optimal balance between proinflammatory and anti-inflammatory cytokines for prolongation and successful completion of pregnancy.
Matrix metalloproteinase (MMP)-8 is found in the granules of mature neutrophils, which are the first to enter the focus of inflammation. One of the effects of MMP-8 is the destruction of the cervical extracellular matrix; thereby further shortening and dilation of the cervical canal, ultimately leading to spontaneous PB [10].
The markers involved in premature cervical maturation and proven to predict PB include IL-6 and IL-8, MMP, tissue inhibitor of metalloproteinases (TIMP) -1, and macrophage colony-stimulating factor (M-CSF) [2, 8].
However, to date, the role of these markers in predicting PB in women with ICI has not been adequately studied, particularly those found locally in cervical mucus.
Therefore, the present study aimed to investigate the clinical value of cervical canal IL-6, IL-8, and MMP-8 in predicting gestational age at delivery in pregnant women with isthmic cervical insufficiency (ICI).
Materials and methods
Sixty-three pregnant women with ICI were enrolled in a prospective cohort study conducted from 2020 to 2022 at the Yudin Perinatal Center.
The diagnosis of ICI was made by ultrasound examination (cervical shortening less than 25 mm and/or dilation of the cervical canal by 10 mm or more) and gynecological examination.
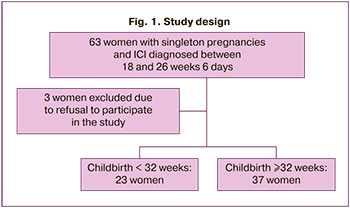
During the study, 3 pregnant women were excluded due to refusal of further participation in the study.
It is known that children born before 32 weeks of gestation (very early and early PB) have significantly higher morbidity and mortality than those born at a later gestational age [8]. For this reason, women were divided into 2 groups depending on the gestational age at delivery. Group 1 consisted of 23 pregnant women with labor occurring before 32 weeks of gestation, and Group 2 consisted of 37 women with labor occurring after 32 weeks of gestation. The study design is shown in Figure 1.
The sample size was calculated by K.A. Odelnova's method: with a study power of 90%, a significance level of α=0.05, and a minimum clinically significant difference of 10%, the required number of patients was 44 and more.
Analysis of the course and outcomes of pregnancy was performed from the time of ICI diagnosis in pregnant women without signs of initial stage and/or active PB on admission to the maternity hospital at 18–26 weeks and 6 days.
The study analyzed the charachteristics of somatic and obstetric and gynecological history, the course of pregnancy, labor and delivery, and the postpartum period, as well as the condition of newborns. Women who met the inclusion criteria were included in the study.
The inclusion criteria were: 1. Women aged 18 years or older; 2. A singleton pregnancy; 3. Signs of ICI by ultrasound measurement of cervical length; 4. Gestational age at diagnosis of ICI of 18–26 weeks 6 days (based on the last menstrual date and / or the first trimester ultrasound examination); 5. Written informed consent of the patient to participate in the study.
Exclusion criteria were: 1. Multiple pregnancy; 2. History of cervical surgery (conization, plasty, cervical tears in previous births, cervical amputation); 3. Fetal bladder prolapse; 4. Starting/active PB; 5. Acute phase or exacerbation of chronic infectious diseases; 6. Pregnant women refusing to participate in the study.
ICI patients were treated and managed according to the approved clinical guidelines "Preterm Birth" and " Isthmic-cervical Insufficiency ".
In addition to basic diagnostic methods, during cervical speculum examination, all patients underwent cervical mucus from the cervical canal using a universal sterile soft universal probe. Cervical mucus was sampled for immunological testing at the time of initial diagnosis of ICI in patients admitted to the maternity hospital at 18–26 weeks, 6 days at the time of diagnosis of ICI. The probe was inserted into the cervical canal and rotated 2 times clockwise, then 2 times counterclockwise. The tip of the probe was then placed in an Eppendorf-type tube containing 1 ml of buffer solution. The biomaterial was centrifuged, the supernatant was taken and stored at -40°C until examination. No complications were observed when taking the biomaterial from the cervical canal, the procedure was safe and low-traumatic.
IL-6, IL-8 concentrations in cervical mucus were determined by enzyme immunoassay using the Human ELISA Kit (Thermo Fisher Scientific, USA) and the MMP-8 - DuoSet Kit (R&D Systems, USA).
The study was approved by the Research Ethics Committee of the I.M. Sechenov First Moscow State Medical University (Ref. No: № 31 of 11.11.2020).
Statistical analysis
Statistical analysis was performed using StatTech v. 2.8.3 (Stattech LLC, Russia). The distribution of continuous variables was tested for normality using the Shapiro-Wilk test (when the number of subjects was less than 50) or the Kolmogorov-Smirnov test (when the number of subjects was greater than 50). Quantitative variables that show normal distribution were expressed as means (M) and standard deviation (SD) and presented as M (SD); otherwise, the median (Me) with the interquartile range (Q1; Q3) was reported. Frequencies and percentages were reported for categorical variables. Normally distributed continuous variables were compared between two groups with a Welch-t test. Differences between two groups with nonnormally distributed data were analyzed using the Mann–Whitney U-test. The percentages were compared using Pearson's chi-square test (χ2) (for expected frequencies greater than 10) and Fisher's exact test (for expected frequencies less than 10) for 2×2 contingency tables. Percentages were compared using Pearson's chi-square test for 2×k contingency tables. Correlation analysis was conducted by calculating Spearman's rank correlation coefficients (for non-normally distributed data). A predictive model characterizing the association of a quantitative variable with factors was developed using linear regression. To assess the predictive significance of quantitative variables when predicting a particular outcome, ROC-curve analysis was used. The threshold value of a quantitative variable at the cut-off point was determined by the highest value of the Juden index. Differences were considered statistically significant at p<0.05.
Results
The mean age of the pregnant women was 30.3 (5.4) years. ICI was first diagnosed at 23.0 (22.0–24.0) weeks of pregnancy. At the same time, cervical canal material was sampled. The median cervical length was 20.9 (19.0–22.5) mm.
The results of the study of the clinical and anamnestic data of pregnant women with ICI, presented in Table 1, showed that the patients in both groups were comparable in terms of age, body mass index, cervical length, obstetric history, and gynecological pathology. However, the incidence of cervical ectopia was statistically significantly higher in Group 1 compared to Group 2 patients (p=0.005).
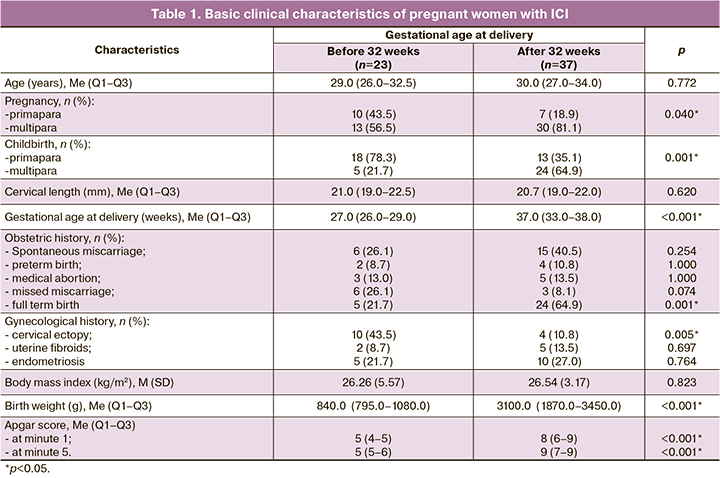
In Group 1, 13/23 (56.5%) women were multipara; only 5 pregnant women (21.7%) were expected to give birth again. And in Group 2, 24 (64.9%) of the 30/37 (81.1%) women were multipara. It should be noted that 64.9% of the patients in Group 2 had previously had full-term births, while in Group 1 only 21.7% of the women had full-term births.
ICI correction was performed according to clinical guidelines. Twenty (33.3%) pregnant women underwent cervical sutures during progesterone therapy, 22 (36.7%) had an obstetric pessary, and 18 (30.0%) pregnant women received ICI correction with progesterone alone.
This pregnancy ended in late spontaneous miscarriage in 2 women (3.3%) and PB in 34 women (43.3%). Full-term delivery occurred in 24 patients (40%). The distribution of gestational ages at delivery is shown in Figure 2.
A cesarean section was performed in 6 patients (10%): in Group 1, in 1 (4.3%) patient; in Group 2, in 5 (13.5%) pregnant women. The indication for surgical delivery in all patients was 2 or more uterine scars after previous cesarean sections.
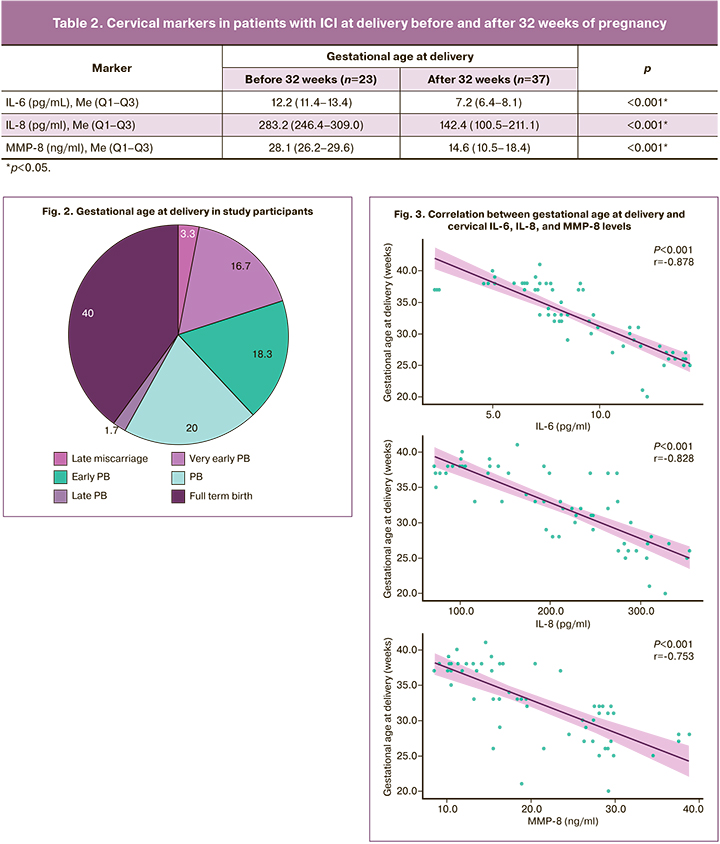
A comparative assessment of the IL-6, IL-8, and MMP-8 levels in the cervical mucus of the patients revealed their statistically significantly higher concentrations in the group of the patients who had been delivered before 32 weeks of pregnancy (p<0.001). The findings are presented in Table 2.
Given the difference in marker concentrations at different gestational ages at delivery, we performed a correlation analysis of the relationship between cervical marker levels at the time of ICI diagnosis and biomaterial sampling and gestational age at delivery. A statistically significant strong inverse correlation (Chaddok scale) was found for all markers (p<0.001).
Figure 3 presents graphs showing the correlations between gestational age at delivery and cervical marker levels at the time of ICI diagnosis. When cervical marker concentrations increase, an earlier gestational age at delivery should be expected.
The association between spontaneous PB and immunological markers in the cervical canal at the time of the initial diagnosis of ICI was described by the following equations:
- For IL-6: Y(gestational age)=-1.412×X(IL-6)+45.357. A 1 pg/ml increase in IL-6 concentration should be expected to decrease gestational age by 1.412 weeks (73.7% of the observed variance);
- for IL-8: Y(gestational age) =-0.052×X(IL-8)+43.551. A 1 pg/mL increase in IL-8 concentration should be expected to decrease gestational age by 0.052 weeks (64.2% of the observed variance);
- for MMP-8: Y(gestational age)=-0.515×X(MMP-8)+42.892. An increase of 1 ng/ml in cervical MMP-8 levels should be expected to decrease gestational age by 0.515 (56.3% of the observed variance).
That is, the higher the level of cervical markers, the more likely is the risk of spontaneous PB in this patient.
Taking into account the association between gestational age at delivery and IL-6, IL-8, and MMP-8 in cervical mucus in ICI patients, we performed ROC analysis and determined threshold values for each of the markers and their predictive value. The main findings are presented in Table 3.
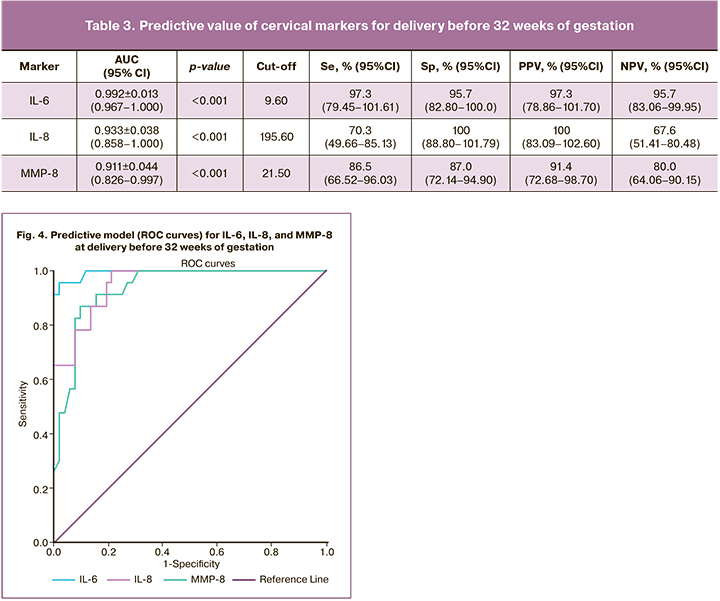
The cutoff concentration of IL-6 was 9.6 pg/ml, IL-8 was 195.6 pg/ml, and MMP-8 was 21.5 ng/ml. Very early and early PB (before 32 weeks) were predicted with high sensitivity at levels of these markers in the cervical mucus above these values. Figure 4 shows the ROC curves for cervical markers in patients with ICI.
Our findings allow effective differentiation between patients with ICI and very early and early PB and those with later gestational age at delivery (after 32 weeks).
Discussion
Studies investigating immunological markers in PB have been conducted for quite some time. Initially, amniotic fluid studies were intended to identify the association between inflammatory cytokine levels with chorioamnionitis and PB. For example, in 2018, Chaemsaithong P. et al. [11] reported a study of amniotic fluid obtained by amniocentesis in patients with symptoms of PB. The authors performed amniotic fluid culture to detect aerobic and anaerobic microorganisms and mycoplasmas and determine leukocyte count, IL-6 and MMP-8. The results showed that MMP-8 was more specific in the detection of intra-amniotic infection. The patients whose leukocyte counts in amniotic fluid were within normal limits and no infectious agent was detected by standard culture techniques, but who had a positive test for MMP-8, gave birth prematurely.
However, amniocentesis is an invasive procedure, which carries certain risks for the mother and the fetus. Therefore, researches have attempted to study the same markers using less invasive methods, such as venous blood, urine and cervical mucus.
Cervical mucus is a medium that reflects the local biochemical status of gestational tissues. Various marker proteins in this medium can be used to predict PB, such as cytokines including IL-1β, -6, -7, -8, -17α, -18; fetal fibronectin, lactoferrin, tumor necrosis factor and many others [12].
The findings of our study suggest that concentrations of IL-6, IL-8, and MMP-8 concentrations in cervical mucus in patients with ICI were significantly higher at delivery before 32 weeks of gestation, which is probably related to the development of endocervical and intraamniotic infections and inflammation (both aseptic and microbial-associated).
IL-6 levels have long been proven to be closely related to microbial-associated intraamniotic inflammation, so its determination in cervical mucus can be used as a simple non-invasive diagnostic method. A study by Kacerovsky et al. proved that the levels of IL-6 and IL-8 in cervical mucus are indicators of intra-amniotic inflammation and consequently PB [13].
As in our study, in 2004, Sakai M et al. determined the level of IL-8 in cervical mucus and obtained similar results. In women with a short cervix, there was a significant relationship between high levels of IL-8 and PB [14]. In contrast, in 2017, Yoo H.N. et al. found no statistically significant association between IL-8 concentration in cervical mucus and the development of PB [8].
In another study in 2020, Park S. et al. showed that elevated levels of several cytokines (macrophage inflammatory proteins 1α and 1β, IL-6, IL-7 and IL-17α) were associated with PB before 34 weeks' gestation, while IL-8 levels did not correlate with gestational age at subsequent delivery. Furthermore, IL-6 and IL-17α showed the highest sensitivity, 80 and 75%, respectively [12]. The authors concluded that these markers can be used as predictors of PB.
MMP-8 in cervical mucus also plays an important role in the formation of ICI, and its high levels, regardless of the presence of intracervical infections, are associated with premature cervical remodeling. Several studies have identified cut-off values for MMP-8 in amniotic fluid indicating a high risk of PB (23 ng/mL) [15] and the development of chorioamnionitis (188.3 ng/mL) [16].
Our study also showed that elevated levels of IL-6, IL-8, and MMP-8 in cervical mucus in patients with ICI may be predictors of very early and early PB.
Given the high incidence of cervical and vaginal infections and, consequently, ascending infection and intra-amniotic inflammation in pregnant women with ICI, our data were compared with the results of the placenta histological examination in women with PB. Pathomorphological examination of the placenta showed signs of histological chorioamnionitis in 69.6% of patients in Group 1 and 27.0% of Group 2 patients (p=0.001; 95% CI: 1.960–19.430). However, opportunistic and pathogenic microbial groups were detected in microbiologically significant titers only in 34.7% and 8.1% of pregnant women, respectively; hence, the remaining women had aseptic inflammation without an infectious agent.
Conclusion
In women with ICI, non-invasive markers, including IL-6, IL-8, and MMP-8, in cervical mucus could be used to predict the course of pregnancy and gestational age at delivery.
Threshold values for IL-6≥9.6 pg/mL, IL-8≥195.6 pg/mL, and MMP-8≥21.5 ng/mL concentrations in the cervical canal can be recommended as predictive of very early and early PB, and are highly likely to be predictors of intraamniotic inflammation/infection regardless of the results of the cervical content culture.
More prospective studies are needed to determine whether these cervical mucus markers can be used to guide the choice of the optimal management strategy for patients with ICI.
References
- Белоусова В.С., Стрижаков А.Н., Тимохина Е.В., Свитич О.А., Богомазова И.М., Пицхелаури Е.Г. Преждевременные роды: от понимания патогенеза к тактике ведения. Акушерство, гинекология и репродукция. 2018; 12(4): 47-51. https://dx.doi.org/10.17749/2313-7347.2018.12.4.047-051. [Belousova V.S., Strizhakov A.N., Timokhina E.V., Svitich O.A.,Bogomazova I.M., Pitskhelauri E.G. Preterm birth: from understanding of pathogenesis to pregnancy management. Akusherstvo, ginekologiya i repriductsiya/Obstetrics, Gynecology and Reproduction. 2018; 12(4): 47-51.(in Russian)]. https://dx.doi.org/10.17749/2313-7347.2018.12.4.047-051.
- Агруц К.Р., Пасман Н.М., Степанова А.А., Каткова Н.С., Дударева А.В.,Кустов С.М., Проничева С.В., Воронова Н.В. Оценка эффективности современных методов коррекции истмико-цервикальной недостаточности. Научное обозрение. Медицинские науки. 2020; 2: 16-20.https://dx.doi.org/10.17513/srms.1091. [Agruts K.R., Pasman N.M., Stepanova A.A., Katkova N.S., Dudareva A.V., Kustov S.M., Pronicheva S.V., Voronova N.V. Evaluation of the effectiveness of modern methods of correction of isthmic-cervical insufficiency. Scientific review. Medical sciences. 2020; 2: 16-20. (in Russian)]. https://dx.doi.org/10.17513/srms.1091.
- Chawanpaiboon S., Vogel J.P., Moller A.B., Lumbiganon P., Petzold M., Hogan D. et al. Global, regional, and national estimates of levels of preterm birth in 2014: a systematic review and modelling analysis. Lancet Glob. Health. 2019; 7(1): e37-e46. https://dx.doi.org/10.1016/S2214-109X(18)30451-0.
- Тимохина Е.В., Стрижаков А.Н., Песегова С.В., Белоусова В.С., Самойлова Ю.А. Выбор метода коррекции истмико-цервикальной недостаточности: результаты ретроспективного исследования. Акушерство и гинекология. 2021; 8: 86-92. https://dx.doi.org/10.18565/aig.2021.8.86-92. [Timokhina E.V., Strizhakov A.N., Pesegova S.V., Belousova V.S., Samoilova Yu.A. The choice of techniques for correction of isthmic-cervical insufficience: the results of the retrospective study. Obstetrics and Gynecology. 2021; 8: 86-92. (in Russian)]. https://dx.doi.org/10.18565/aig.2021.8.86-92.
- Koullali B., Westervelt A.R., Myers K.M., House M.D. Prevention of preterm birth: Novel interventions for the cervix. Semin. Perinatol. 2017; 41(8): 505-10. https://dx.doi.org/10.1053/j.semperi.2017.08.009.
- Kim S., Park H.S., Kwon H., Seol H.J., Bae J.G., Ahn K.H. et al.; Korean Society of Ultrasound in Obstetrics and Gynecology Research Group. Effect of cervical cerclage on the risk of recurrent preterm birth after a twin spontaneous preterm birth. J. Korean Med. Sci. 2020; 35(11): e66. https://dx.doi.org/10.3346/jkms.2020.35.e66.
- Курцер М.А., Азиев О.В., Панин А.В., Егикян Н.М., Болдина Е.Б., Грабовская А.А. Лапароскопический серкляж при истмико-цервикальной недостаточности, вызванной ранее перенесенными операциями на шейке матки. Акушерство и гинекология. 2017; 5: 58-62.https://dx.doi.org/10.18565/aig.2017.5.58-62. [Kurtser M.A., Aziev O.V., Panin A.V., Egikyan N.M., Boldina E.B., Grabovskaya A.A. Laparoscopic cerclage for isthmico-cervical insufficiency caused by previous surgery on the cervix. Obstetrics and Gynecology. 2017; 5: 58-62. (in Russian)].https://dx.doi.org/10.18565/aig.2017.5.58-62.
- Yoo H.N., Park K.H., Jung E.Y., Kim Y.M., Kook S.Y., Jeon S.J. Non-invasive prediction of preterm birth in women with cervical insufficiency or an asymptomatic short cervix (≤25 mm) by measurement of biomarkers in the cervicovaginal fluid. PLoS One. 2017; 12(7): e0180878.https://dx.doi.org/10.1371/journal.pone.0180878.
- Tarca A.L., Fitzgerald W., Chaemsaithong P., Xu Z., Hassan S.S., Grivel J.C. et al. The cytokine network in women with an asymptomatic short cervix and the risk of preterm delivery. Am. J. Reprod. Immunol. 2017; 78(3): e12686.https://dx.doi.org/10.1111/aji.12686.
- Van Lint P., Libert C. Matrix metalloproteinase-8: cleavage can be decisive. Cytokine Growth Factor Rev. 2006; 17(4): 217-23. https://dx.doi.org/10.1016/j.cytogfr.2006.04.001.
- Chaemsaithong P., Romero R., Docheva N., Chaiyasit N., Bhatti G., Pacora P. et al. Comparison of rapid MMP-8 and interleukin-6 point-of-care tests to identify intra-amniotic inflammation/infection and impending preterm delivery in patients with preterm labor and intact membranes. J. Matern. Fetal Neonatal Med. 2018; 31(2): 228-44. https://dx.doi.org/10.1080/14767058.2017.1281904.
- Park S., You Y.A., Yun H., Choi S.J., Hwang H.S., Choi S.K. et al. Cervicovaginal fluid cytokines as predictive markers of preterm birth in symptomatic women. Obstet. Gynecol. Sci. 2020; 63(4): 455-63. https://dx.doi.org/10.5468/ogs.19131.
- Kacerovsky M., Musilova I., Jacobsson B., Drahosova M., Hornychova H.,Janku P. et al. Cervical fluid IL-6 and IL-8 levels in pregnancies complicated by preterm prelabor rupture of membranes. J. Matern. Fetal Neonatal Med. 2015; 28(2): 134-40. https://dx.doi.org/10.3109/14767058.2014.908179.
- Sakai M., Sasaki Y., Yoneda S., Kasahara T., Arai T., Okada M. et al. . Elevated interleukin-8 in cervical mucus as an indicator for treatment to prevent premature birth and preterm, pre-labor rupture of membranes: a prospective study. Am. J. Reprod. Immunol. 2004; 51(3): 220-5. https://dx.doi.org/10.1111/j.1600-0897.2004.00145.x.
- Keeler S.M., Kiefer D.G., Rust O.A., Vintzileos A., Atlas R.O., Bornstein E., Hanna N. Comprehensive amniotic fluid cytokine profile evaluation in women with a short cervix: which cytokine(s) correlates best with outcome? Am. J. Obstet. Gynecol. 2009; 201(3): 276.e1-6. https://dx.doi.org/10.1016/j.ajog.2009.05.045.
- Kim S.M., Romero R., Park J.W., Oh K.J., Jun J.K., Yoon B.H. The relationship between the intensity of intra-amniotic inflammation and the presence and severity of acute histologic chorioamnionitis in preterm gestation. J. Matern. Fetal Neonatal Med. 2015; 28(13): 1500-9. https://dx.doi.org/10.3109/14767058.2014.961009.
Received 19.06.2022
Accepted 29.09.2022
About the Authors
Elena V. Timokhina, Dr. Med. Sci., Professor, Department of Obstetrics, Gynecology and Perinatology, I.M. Sechenov First Moscow State Medical University, Ministry of Health of Russia (Sechenov University), +7(916)607-45-34, +7(499)782-30-45, elena.timokhina@mail.ru, https://orcid.org/0000-0001-6628-0023, 119991, Russia, Moscow,B. Pirogovskaya str., 2-4.
Alexander N. Strizhakov, Academician of RAS, Professor, Head of the Department of Obstetrics, Gynecology and Perinatology, I.M. Sechenov First Moscow State Medical University, Ministry of Health of Russia (Sechenov University), +7(499)782-30-45, kafedra-agp@mail.ru, 119991, Russia, Moscow, B. Pirogovskaya str., 2-4.
Svetlana V. Pesegova, Post-Graduate Student, Department of Obstetrics, Gynecology and Perinatology, I.M. Sechenov First Moscow State Medical University, Ministry of Health of Russia (Sechenov University), +7(499)782-30-45, svpesegova@gmail.com, https://orcid.org/0000-0002-1339-5422, 119991, Russia, Moscow, B. Pirogovskaya str., 2-4.
Corresponding author: Elena V. Timokhina, elena.timokhina@mail.ru
Authors' contributions: Strizhakov A.N., Timokhina E.V., Pesegova S.V. – conception and design of the study; Timokhina E.V., Pesegova S.V. – data collection, manuscript drafting; Strizhakov A.N., Timokhina E.V. – manuscript reviewing and editing; Pesegova S.V. – statistical analysis and visualization.
Conflicts of interest: The authors have no conflicts of interest to declare.
Funding: There was no funding for this study.
Ethical Approval: The study was approved by the Research Ethics Committee of the I.M. Sechenov First Moscow State Medical University (Ref. No: № 31 of 11.11.2020 г.).
Patient Consent for Publication: All patients provided informed consent for the publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available on request from the corresponding author after approval from the principal investigator.
For citation: Timokhina E.V., Strizhakov A.N., Pesegova S.V. The role of immunological markers in predicting the course and outcome of pregnancy in patients with isthmic cervical insufficiency.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2022; 10: 50-57 (in Russian)
https://dx.doi.org/10.18565/aig.2022.10.50-57



