Evaluation of contamination with high-risk human papillomavirus types according to the screening results
Objective: Assessment of contamination with high-risk human papillomavirus (HR HPV) in women in Perm and Perm region according to the screening results.Bulatova I.A., Shevlyukova T.P., Nenasheva O.Yu., Shchekotova A.P., Spirina A.B.
Materials and methods: HPV DNA test of 498 women aged 46.5 (10.4) years was performed: liquid-based cytology with ScBD PrepStain (“TriPath Imaging Inc.”, USA) and HPV genotyping and quantification of 14 HR HPV types HPV types 16,18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, 68 by PCR with real-time «CFХ-96» («Bio-Rad Laboratories, Inc.», USA).
Results: Screening test results showed that HR HPV was detected in 13.6% women. Among them type 16 was found in 2.8% women, type 18 in 0.4% and type 45 in 1.4%, and the other HR HPV were found in 9% of women. At the same time, 75% of samples were HR HPV positive in women aged 30–49 лет. Distribution of HR HPV genotypes was as follows: type 16 – 21% , types 18 and 45 – 3% and 10%, respectively, other types – 66%. According to cytology results, 88% of women were NILM, 12% had inflammatory changes in smears and bacterial vaginosis.
Conclusion: According to screening test results HR HPV was detected in 13,6% of women predominantly HPV infection was not accompanied by cytological signs of viral lesions and atypia of cells.
Keywords
The issue related to early diagnosis of human papillomavirus infection is extremely urgent. According to various estimates, HPV infection is 30–80% worldwide. It has been proved, that more than 95% of cervical neoplasia is associated with high-risk HPV. The incidence of cervical cancer (CC) increases annually in Russia, and over the past ten years, it has amounted to almost 25%. At the same time, CC is diagnosed at later stages in almost a third of cases, and 30% of women are asymptomatic carriers of HPV [1–3].
Among women with high grade squamous intraepithelial lesion (HSIL) and СС, HR-HPV types 16, 31, 33, 4, 52, 58 are most common. Moreover, despite the presence or absence of clinical features of cervical morphological changes, HPV type 16 is the most frequently found type [4].
The issue of HPV testing and the choice of the most effective method for screening test remains in the focus of the global healthcare community. Today, in most economically developed countries, HPV testing for oncogenic human papillomavirus (HR-HPV) is included in the CC prevention program as a primary screening test [5, 6]. High sensibility and predictive value of HPV-negative results determine the expedience of using HPV test-based cervical cancer screening, as HPV negative test exclude development of CC in the nearest 3–5 years [7, 8].
Global screening strategies available nowadays are based on cotesting (HPV test + liquid-based cytology (LBC)) or HPV test with subsequent cytological or immunocytochemical analysis of sorted cells [9–11].
Since January 2021, a new Provision of medical care in the field of obstetrics and gynecology, approved by the Decree of the Government of the Russian Federation (RF) No. 868 of 17.06.2020, and the Order of the Ministry of Health of the RF No. 1130n of 20.10.2020 “On approval of the procedure for medical care in the field of obstetrics and gynecology” came into force in the RF. The new Procedure is supplemented with the provisions related to screening of women's health. It is carried out as a part of preventive medical examination or the periodic health examination. Liquid-based cytology (LBC) for cervical cancer screening should be performed at the age of 21–29 years once every 3 years; and cotesting, i.e. cytology/LBC with the Papanicolaou staining (Pap cytology) and HPV genotyping using HPV self-sampling should be performed at the age of 30–65 years once every 5 years. This part of preventive medical examination is considered to be completed, when 80% or more of female population is covered.
The objective of the study was assessment of contamination with high-risk human papillomavirus (HR-HPV) in women in Perm and Perm region according to the screening results.
Material and methods
498 women aged 22–72 years were examined on an outpatient basis in Perm and Perm region. Polymerase chain reaction (PCR)-based HPV DNA genotyping and quantification of 14 HR-HPV types (16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, 68 г), genotyping of HPV types 16, 18 and 45, determination of viral genome integration probability (clinical significance) in the cervical smears with a set of reagents "AmpliSense HPV-VKR screen-titer-14-FL" (Central Research Institute of Epidemiology of Rospotrebnadzor) and hybridization-fluorescence detection of amplified products with Real-Time CFX96 Touch96 system (Bio-Rad Laboratories, Inc., USA) was performed.
Clinical significance of HR-HPV allowed to assess viral genome integration probability and interprete 3 levels: low level of significance, significant and high level of significance. Liquid-based cytology (LBC) was performed with BD PrepStain system for preparation and staining of cytology samples using BD SurePath (“TriPath Imaging Inc.”, USA).
Statistical analysis
STATISTICA 7.0 and Microsoft Office Excel 2016 was used for statistical data processing. The quantitative parameters were presented as median (M) and standard deviation (SD). Spearman’s rank correlation coefficient was used to measure association between the variables. The differences between the samples were considered significant at p<0.05.
Results and discussion
The mean age of the examined women was 46.5 (10.4) years. To identify genomic DNA, it was important that at least 500 epithelial cells should be present observed in a Pap smear. In 34 samples (7 %) the number of epithelial cells was less than 500, and it was insufficient for genomic DNA identification. Due to this, re-examination was necessary at the discretion of the attending physician. In addition, HR-HPV DNA copy number in some probes was less than 1 log/100 000 cells. Clinical significance was low, but this does not exclude the presence of infection. LBC results showed no intraepithelial and malignant lesions (NILM) in all probes.
Clinical example
The Patient K., born on October 05, 1976. The results of DNA HPV test (HPV types 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, 68), total HPV DNA quantification and HPV genotyping (16, 18, 45) and detection of possible viral genome integration into genomic DNA of the patient P, born in 1981:
Number of cells – less than 71;
- HR-HPV DNA (14 types, Е1/Е2/Е7 genes) less than 1 log/100 000 cells;
- HPV DNA type 16 (Е6 gene) less than 1 log/100 000 cells;
- Total HPV DNA levelS (log scale) less than 1 lg /105 CC cells.
Clinical significance was interpreted as low level of significance.
Notes: The number of genomic DNA (small number of epithelial cells) was insufficient. Decision of re-examination should be taken by the attending physician.
Liquid-based cytology results showed NILM. The cytogram did not show specific clinical features.
According to statistics, about 10% of smears are not adequate due to wrong material collection and sample preparation [12, 13].
Screening test results showed that HR-HPV was in 68/498 (13.6%) women, among them type 16 was found in 14/498 (2.8%), type 18 – in 2/498 (0.4%), type 45 – in 7/498 (1.4%) women. Other types of HR-HPV were found in 45/498 (9%) women.
The obtained results correlated with average data in Russia, although the data on HR-HPV infection are variable in some regions. This may be due to different age and territorial allocation of the examined patients. For example, in Tyumen region, HPV infection was found in 14.9% of women. Among them, type 16 was detected in 8.1%, type 18 – in 6.8% of patients with HPV positive test results [14].
According to the data in Lipetsk region, HR-HPV was detected in 7.7% of women [15], in Krasnodar region the prevalence of HPV was 21.4%, in Kaluga region – 13.1%. According to the data in Chelyabinsk region, high risk HR-HPV was identified in 58.2% of women [16]. In Ingushetia, the rate was considerably lower – in 10.7% of patients [17]. Considering the findings in previous studies in Perm, quantitative PCR assay for HPV detection (types 16, 18) showed that 6.5% of women had HPV positive results [18]. Among the citizens of Moscow and Moscow region, the rates of HR-HPV vary in different studies from 14% to 24.7%. In 36 % of PHV-positive women, types 16 и 18 were identified [19, 20].
Further, we analyzed the incidence of high risk HPV among different age groups of women. The analysis showed that 75% of women aged 30–49 years had HR-HPV-positive test results (Table 1).
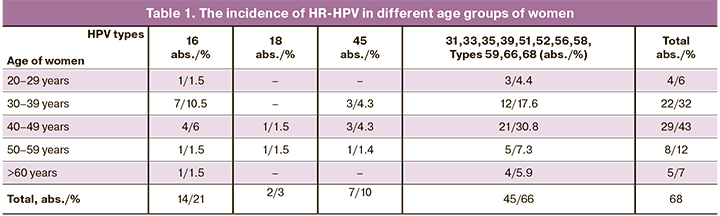
HPV type 16 was found in all age groups, but most common among women aged 30–39 years. Type 18 was detected in groups aged 40–49 and 50–59 years. Type 45 was identified almost in half of cases among women aged 40–49 years; Approximately the same rate of other HR-HPV genotypes was in all age groups of women.
Young women of reproductive age are more likely to be at high risk of HPV infection. According to a number of authors, the infection rate is 15–35% among women aged 18–30 years [19, 21].
However, in our study 75 % of HR-HPV DNA positive probes was found among women at a more mature age – from 30 to 49 years. Probably, this was related to the contingent of examined women.
The distribution of genotypes in the structure of HP HPV was the following: type 16 was 21%, types 18 and 45 – 3 and 10%, respectively, other types 66%. According to other studies, the most common types of HPV were 16, 31, 33, 44, 52, 58 and 68 [4, 22].
Among HR-HPV-positive test results, 47% were of low clinical significance, 28% were significant and 25% had a high level of significance. Thus, the level of clinical significance of more than half cases of HR-HPV (53%) was significant and of high level of significance. This should be taken in account, when treatment is prescribed.
Additionally, it should be noted, that correlation of the viral load with the level of clinical significance of HR-HPV was positive: r=0.56 (0.31–0.73); р=0.003.
Distribution of HR-HPV type 16 depending on clinical significance was almost similar, and type 18 had a high level of clinical significance (Table 2).
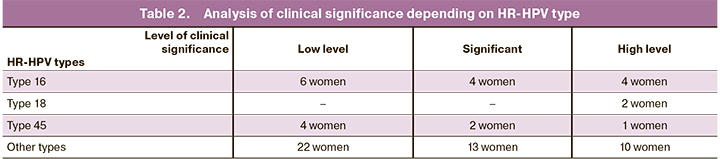
In the group of women with HPV type 45 the level of clinical significance was low in most cases; among other HR-HPV types, this level of significance was almost in half of the cases.
PCR-based HR HPV test using LBC samples showed no signs of atypia and viral lesions in women with HR-HPV positive test results. According to the results of cervical LBC, NILM was in 88% of women, inflammatory type of smear was in 7%, candidal colpitis was in 2% and bacterial vaginosis in 1% of women.
The data in publications vary. For example, during medical examination of female students in Perm, cytology results showed the signs of viral lesions in 2.4% of samples [18]. According to our previous studies, cytology results in Perm region showed, that HR-HPV detection rate was 0.03% [23].
In Ingushetia, cytology results showed cervical intraepithelial neoplasia (CIN) grades II, III in 1.5% of HR-HPV positive women [24]. In Lipetsk region, 68.5% of women with HR-HPV infection had atypical squamous cells of undetermined significance (ASC-US) [13].
Conclusion
Thus, according to screening test results HR-HPV was detected in 68/498 (13.6%) women predominantly at the age of 30–49 years, who were examined on an outpatient basis. In the structure of HPV, the prevalence of types 16, 18 and 45 was 34%. Cervical HR-HPV infection was not not accompanied by cytological signs of viral lesions and atypia of cells.
The obtained results demonstrate the feasibility of using large-scale combined testing for detection, prevention and early diagnosis of HR-HPV.
References
- Каприн А.Д., Старинский В.В., Петрова Г.В., ред. Злокачественные новообразования в России в 2018 году (заболеваемость и смертность). М.: МНИОИ им. П.А. Герцена – филиал ФГБУ «НМИЦ радиологии» Минздрава России; 2019. 250c. [Kaprin A.D., Starinskiy V.V., Petrova G.V., ed. Malignant neoplasms in Russia in 2018 (morbidity and mortality). M.: P.A. Herzen Moscow State Medical Research Institute – branch of the NMRC of Radiology of the Ministry of Health of the Russian Federation; 2019. 250 p. (in Russian)].
- Каприн А.Д., Старинский В.В., Петрова Г.В., ред. Состояние онкологической помощи населению России в 2018 году. М.: МНИОИ им. П.А. Герцена – филиал ФГБУ «НМИЦ радиологии» Минздрава России; 2019. 236с. [Kaprin A.D., Starinskiy V.V., Petrova G.V., ed. The state of cancer care for the population of Russia in 2018. M.: P.A. Herzen Moscow State Medical Research Institute – branch of the NMRC of Radiology of the Ministry of Health of the Russian Federation; 2019. 236 p. (in Russian)].
- Сметанина О.В., Кузьминых Д.А., Сметанина С.В., Гамаюнов С.В., Ускова Е.Ю. Скрининг рака шейки матки: к вопросу об организации. Акушерство и гинекология. 2021; 4: 143-9. [Smetanina O.V., Kuz'minykh D.A., Smetanina S.V., Gamayunov S.V., Uskova E.Yu. Cervical Cancer Screening: An Organization Question. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2021; 4: 143-9 (in Russian)]. https://dx.doi.org/10.18565/aig.2021.4.143-149.
- Мзарелуа Г.М., Назарова Н.М., Некрасова М.Е., Сычева Е.Г., Бурменская О.В., Стародубцева Н.Л., Асатурова А.В., Хабас Г.Н., Павлович С.В. Распространенность типов вируса папилломы человека у пациенток с цервикальными интраэпителиальными неоплазиями различной степени тяжести. Акушерство и гинекология. 2018; 4: 94-100. [Mzarelua G.M., Nazarova N.M., Nekrasova M.E., Sycheva E.G., Burmenskaya O.V., Starodubtseva N.L. et аl. Prevalence of human papillomavirus types in patients with cervical intraepithelial neoplasias of varying severity. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2018; 4: 94-100. (in Russian)]. https://dx.doi.org/10.18565/aig.2018.4.94-100.
- WHO. WHO report on cancer: setting priorities, investing wisely and providing care for all. Switzerland: Geneva; 2020. 160с. Аvailable under the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo).
- Crossley B., Crossley J. A review of the use of human papilloma virus (HPV) in cervical screening. Br. J. Biomed. Sci. 2017; 74(3):105-9. https://dx.doi.org/10.1080/09674845.2017.1332555.
- Гатагажева З.М., Никитина В.П., Неродо Г.А., Леонов М.Г., Узденова З.Х., Шелякина Т.В., Льянова З.А., Сапралиева Д.О. Оптимизация выявления и лечения заболеваний шейки матки, выявленных на «Открытом приеме» в Республике Ингушетия. Современные проблемы науки и образования. 2016; 4: 8. [Gatagazheva Z.M., Nikitina V.P., Nerodo G.A. Optimization of detection and treatment of cervical diseases identified at the "Open Reception" in the Republic of Ingushetia. Sovremennye problemy nauki i obrazovaniya/ Modern problems of science and education. 2016; 4: 8. (in Russian)]. http://www.science-education.ru/ru/article/view
- Bosch F.X., Lorincz A., Muñoz N., Meijer C.J., Shah K.V. The causal relation between human papillomavirus and cervical cancer. J. Clin. Pathol. 2002; 55(4): 244-65. https://dx.doi.org/10.1136/jcp.55.4.244.
- Министерство здравоохранения Российской Федерации. Российское общество акушеров-гинекологов (РОАГ). Общероссийская общественная организация «Российское общество специалистов по профилактике и лечению опухолей репродуктивной системы (РОСОРС). Клинические рекомендации. Цервикальная интраэпителиальная неоплазия, эрозия и эктропион шейки матки. М.; 2020. 59c. [Russian Society of Obstetricians and Gynecologists. Clinical recommendations. Cervical intraepithelial neoplasia, erosion and ectropion of the cervix. M.; 2020. 59 p. (in Russian)].
- Li Y.C., Zhao Y.Q., Li T.Y., Chen W., Liao G.D., Wang H.R. et al. The performance of immunocytochemistry staining as triaging tests for high-risk HPV-positive women: a 24-month prospective study. J. Oncol. 2020; 2020: 6878761. https://dx.doi.org/10.1155/2020/6878761.
- Benevolo M., Mancuso P., Allia E., Gustinucci D., Bulletti S., Cesarini E. et al. New Technologies for Cervical Cancer 2 (NTCC2) Working Group. Determinants of p16/Ki-67 adequacy and positivity in HPV-positive women from a screening population. Cancer Cytopathol. 2021; 129(5): 383-93. https://dx.doi.org/10.1002/cncy.22385.
- Савельева Г.М., Сухих Г.Т., Серов В.Н., Радзинский В.Е., Манухин И.Б., ред. Национальное руководство по гинекологии. М.: ГЭОТАР-Медиа; 2017. 1008с. [Savel'eva G.M., Sukhikh G.T., Serov V.N., Radzinskiy V.E., Manukhin I.B., ed. National Guide to Gynecology. M.: GEOTAR-Media; 2017. 989 p. (in Russian)].
- Каприн А.Д., Новикова Е.Г., Трушина О.И., Грецова О.П. Скрининг рака шейки матки – нерешенные проблемы. Исследования и практика в медицине. 2015; 1(2): 36-41. [Kaprin A.D., Novikova E.G., Trushina O.I., Gretsova O.P. Screening for cervical cancer is an unresolved issue. Issledovaniya i praktika v meditsine/ Research and practice in medicine. 2015; 1 (2): 36-41. (in Russian)].
- Фролова О.В., Васильева А.Ю. Изучение распространения высококанцерогенных типов вируса папилломы человека среди жителей г. Тюмени и Тюменской области. Фундаментальные исследования. 2007; 7: 35-6. [Frolova O.V., Vasil'eva A.Yu. Study of the spread of highly carcinogenic types of human papillomavirus among residents of Tyumen and the Tyumen region. Fundamental'nye issledovaniya/ Basic research. 2007; 7: 35-6 (in Russian)].
- Аполихина И.А., Баширова Л.К., Летникова Л.И., Худякова О.В., Иванов С.В., Горбунова Е.А., Долгушина Н.В. Оценка инфицированности вирусом папилломы человека женщин Липецкой области с использованием диагностического теста самозабора материала. Акушерство и гинекология. 2018; 11: 98-104. [Apolikhina I.A., Bashirova L.K., Letnikova L.I., Khudyakova O.V., Ivanov S.V., Gorbunova E.A. et al. Evaluation of human papillomavirus infection in women in Lipetsk region using a self-sampling diagnostic test. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2018; 11: 98-104. (in Russian)]. https://dx.doi.org/10.18565/aig.2018.11.98-104.
- Долгушина В.Ф., Абрамовских О.С. Распространенность различных генотипов вируса папилломы человека при патологии шейки матки. Акушерство и гинекология. 2011; 4: 69-74. [Dolgushina V.F., Abramovskikh O.S. Prevalence of different genotypes of human papillomavirus in cervical pathology. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2011; 4: 69-74. (in Russian)].
- Гатагашева З.М., Узденова З.Х., Зеленова О.В. Оценка информативности региональной скрининговой программы по выявлению патологии шейки матки. Акушерство и гинекология. 2019; 7: 98-102. [Evaluation of the information content of the regional screening program to identify the pathology of the cervix. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2019; 7: 98-102. (in Russian)]. https://dx.doi.org/10.18565/aig.2019.7.98-102.
- Олина А.А., Ширинкина Е.В., Метелева Т.А., Шевлюкова Т.П. Остроконечные кондиломы. Официальная статистика, клинические проявления и эффективность терапии. Медицинский совет. 2019; 13: 86-92. [Olina A.A., Shirinkina E.V., Meteleva T.A., Shevlyukova T.P. Genital warts. Official statistics, clinical manifestations and effectiveness of therapy. Meditsinskiy sovet/Medical Council. 2019; 13: 86-92. (in Russian)]. https://dx.doi.org/10.21518/2079-701X-2019-13-86-92.
- Роговская С.И., Михеева И.В., Шипулина О.Ю., Минкина Г.Н., Подзолкова Н.М., Радзинский В.Е., Шипулин Г.А. Распространенность папилломавирусной инфекции в России. Эпидемиология и вакцинопрофилактика. 2012; 1: 25-33. [Rogovskaya S.I., Mikheeva I.V., Shipulina O.Yu., Minkina G.N., Podzolkova N.M., Radzinskiy V.E. i dr. The prevalence of human papillomavirus infection in Russia. Epidemiologiya i vaktsinoprofilaktika/ Epidemiology and Vaccine Prevention. 2012; 1(62): 25-33. (in Russian)].
- Бдайциева Э.Т., Михеева И.В. Оценка распространенности папилломавирусной инфекции. В кн.: Сборник научных статей МПФ ППО ММА им. И.М. Сеченова «Профилактическая медицина – практическому здравоохранению». 2010; 4: 193-8. [Bdaytsieva E.T., Mikheeva I.V. Assessment of the prevalence of human papillomavirus infection. Collection of scientific articles of the IPF PPO I.M. Sechenov MMA "Preventive medicine – practical health care". 2010; 4: 193-8. (in Russian)].
- Маянский А.Н. Вирус папилломы человека – онкогенный вирус. Педиатрическая фармакология. 2010; 7(4): 48-55. [Mayanskiy A.N. Human papillomavirus is an oncogenic virus. Pediatricheskaya farmakologiya/ Pediatric Pharmacology. 2010; 7(4): 48-55. (in Russian)].
- Назарова Н.М., Бурменская О.В., Суламанидзе Л.А., Прилепская В.Н., Павлович С.В., Трофимов Д.Ю. Распространенность типов вируса папилломы человека аногенитальной области у пациенток с ВПЧ-ассоциированными заболеваниями шейки матки. Акушерство и гинекология. 2015; 12: 89-96. [Nazarova N.M., Burmenskaya O.V., Sulamanidze L.A., Prilepskaya V.N., Pavlovich S.V., Trofimov D.Yu. Prevalence of types of human papillomavirus in the anogenital region in patients with HPV-associated diseases of the cervix. Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2015; 12: 89-96. (in Russian)].
- Щекотова А.П., Булатова И.А., Падучева С.В., Шабиева О.Р., Погребнова Л.С., Безматерных С.П., Сапрыкина И.А. Анализ результатов цитологического скрининга шейки матки у лиц, проживающих в Пермском крае. Пермский медицинский журнал. 2020; 37(3): 66-74. [Shchekotova A.P., Bulatova I.A., Paducheva S.V., Shabieva O.R., Pogrebnova L.S., Bezmaternykh S.P. et al. Analysis of the results of cytological screening of the cervix in persons living in the Perm region. Permskiy meditsinskiy zhurnal/ Perm Medical Journal. 2020; 3(37): 66-75. (in Russian)].
Received 09.06.2021
Accepted 12.07.2021
About the Authors
Irina A. Bulatova, Dr. Med. Sci., Head of the Department of Normal Physiology, Professor of the Department of Faculty Therapy No. 2, Occupational Pathologyand Clinical Laboratory Diagnostics, Academician E.A. Wagner Perm State Medical University, Ministry of Health of Russia, +7(922)315-92-88, bula.1977@mail.ru,
http://orcid.org/0000-0002-7802-4796, 614990, Russia, Perm, Petropavlovskaya str., 26.
Tatyana P. Shevlyukova, Dr. Med. Sci., Professor of the Department of Obstetrics and Gynecology, Tyumen State Medical University, Ministry of Health of Russia,
+7(922)394-28-08, tata21.01@mail.ru, https://orcid.org/0000-0002-7019-6630, 625023, Russia, Tyumen, Odesskaya str., 54.
Olga Yu. Nenasheva, PhD, Head of the Medical Laboratory "MedLabExpress", +7(342)240-40-40, +7(963 8701118, svsh@medlabexpress.perm.ru,
614077, Russia, Perm, Ushinskogo str., 4.
Alevtina P. Shchekotova, Dr. Med. Sci., Professor of the Department of Faculty Therapy No. 2, Occupational Pathology and Clinical Laboratory Diagnostics,
Academician E.A. Wagner Perm State Medical University, Ministry of Health of Russia, +7(342)217-10-31, al_shchekotova@mail.ru,
http://orcid.org/0000-0003-0298-2928, 614990, Perm, Petropavlovskaya str., 26,
Anna B. Spirina, Head of the Clinical Diagnostic Laboratory, Perm Regional Oncological Dispensary, +7(908)240-61-81, permcancer@yandex.ru,
614066, Russia, Perm, Bauman str., 15.
Corresponding author: Irina A. Bulatova, bula.1977@mail.ru
Authors’ contributions: Bulatova I.A., Shevlyukova T.P. – the concept and design of the study; Spirina A.B., Nenasheva O.Yu. – material collection and processing; Bulatova I.A., Shchekotova A.P. – statistical data processing; Bulatova I.A.,
Shevlyukova T.P. – writing the text of the article; Bulatova I.A. – editing the text of the article.
Conflicts of interest: The authors declare that they have no conflict of interests.
Funding: The study was conducted without any sponsorship.
Patient Consent for Publication: All patients provided informed consent for the publication of their data.
Authors' Data Sharing Statement: The data supporting the findings of this study are available on request from the corresponding author after approval from the principal investigator.
For citation: Bulatova I.A., Shevlyukova T.P., Nenasheva O.Yu., Shchekotova A.P., Spirina A.B. Evaluation of contamination with high-risk human papillomavirus types
according to the screening results.
Akusherstvo i Ginekologiya/Obstetrics and Gynecology. 2021; 10: 112-117 (in Russian)
https://dx.doi.org/10.18565/aig.2021.10.112-117