A new method for surgical treatment of uterine scar insuffisiency after a previous cesarean section using an intrauterine manipulator with a groove
Aim. The evaluation of the laparoscopic surgery for cesarean scar insufficiency after a previous cesarean section.Makiyan Z.N., Adamyan L.V., Karabach V.V., Chuprynin V.D.
Material and methods. Between 2018 and 2019, 15 patients with uterine scar dehiscence were managed at the department of operative gynecology, Federal State National Medical Research Center of Obstetrics, Gynecology and Perinatology named after. V.I. Kulakov, Russian Ministry of Helthcare.
Results. A new method was developed for laparoscopic metroplasty of uterine scar insufficiency using a new intrauterine manipulator with a groove. The use of the new method resulted in the optimization of the insufficient scar excision, which is evaluated such surgical stages, as: scar incision; conjoin to connecting margins and myometrial suturing of all layers, for repair the complete myometrial segment, that allows for effective restoration of the lower uterine segment with the formation of a mature scar.
Conclusion. The new intrauterine manipulator with a groove can be recommended for routine clinical application to optimize the management of uterine scar insufficiency after previous surgery.
Keywords
According to the estimates of the World Health Organization (WHO), cesarean section rates continue to increase worldwide and currently account for more than 23% of all deliveries. [1-3]. In Russia in 2018, this figure constituted 29.4%, and in some obstetric hospitals, it was more than 30–40%, of which about 60% of cases were first births [1–8].
About 12–20% of patients undergoing caesarean delivery develop postoperative complications; in some cases, with the formation of myometrial thinning or dehiscence of the uterine scar [3-14]. According to the International Classification of Diseases (ICD-10), code O34. 2 is assigned to the diagnosis “Maternal care due to uterine scar after previous surgery” [15].
Maternal care due to uterine scar dehiscence (myometrial thinning) after previous surgery includes surgery, that is, repair of uterine scar dehiscence (metroplasty).
According to the definition of the WHO (2015), possible symptoms of uterine scar dehiscence include [1, 3]:
- myometrial thinning of less than 2-3 mm or even its complete absence in the scar area;
- the presence of a “niche” from inside the uterine cavity or cervical canal;
- irregularly-shaped scar and the presence of cysts or inclusions;
- the presence of thickenings or impressions in the scar;
- the significant predominance of connective tissue, but underdeveloped muscle tissue, and a poor capillary network.
Repair of postoperative uterine scar dehiscence includes uterine scar excision, followed by the closure of the uterine defect and re-constitution of the uterine wall in the lower uterine segment [2–8, 11–14].
The uterine scar may be excised by laparoscopic, laparotomic, or vaginal operative approaches using various surgical energy devices including the application of a monopolar electric current (monopolar needle or hook), ultrasonic scalpel (Harmonic), and mechanical scissors [3-5, 8-14].
The combined laparoscopic and hysteroscopic technique (hysteroresectoscopy) of uterine scar dehiscence repair is the most common and considered effective by many authors. The effectiveness of laparoscopic metroplasty is about 93%; vaginal access metroplasty was effective in 90.5% [4–7, 16–19].
The uterine scar dehiscence after the metroplasty was observed in about 7-9.5% of patients; 23–35% of patients were found to have a niche from inside the cervical canal, and the thickness of the scar approaches the minimum acceptable size (about 4-6 mm) [2, 4–12, 16–19 ].
The study was aimed to optimize surgical management of uterine scar dehiscence (thinning) after a previous caesarean section.
Materials and methods
Between 2018 and 2019, 15 patients with uterine scar dehiscence (thinning) were managed at the Department of Operative Gynecology, V.I. Kulakov NMRC for OG&P of Minzdrav of Russia.
The patients underwent a complete clinical and laboratory examination, including ultrasound of the pelvic organs and urinary system; 7 patients received magnetic resonance imaging (MRI) to evaluate the scar topography.
Surgical treatment was performed in accordance with the WHO clinical guidelines [1, 3]. Metroplasty using video-assisted endoscopic technologies was approved by order of the Ministry of Health of the Russian Federation dated April 16, 2019, No. 217n (nomenclature A16.20.039.001).
Results
Fifteen patients aged 25 to 39 with a history of 1- 3 caesarean deliveries were submitted to surgical treatment.
One patient aged 38 who had 3 previous caesarean deliveries and underwent metroplasty for uterine scar dehiscence (see clinical example) postoperatively was found to have a deep niche in the scar region, and the myometrium thickness above the niche was less than 2 mm.
Metroplasty was performed laparoscopically using an intrauterine device with a groove.
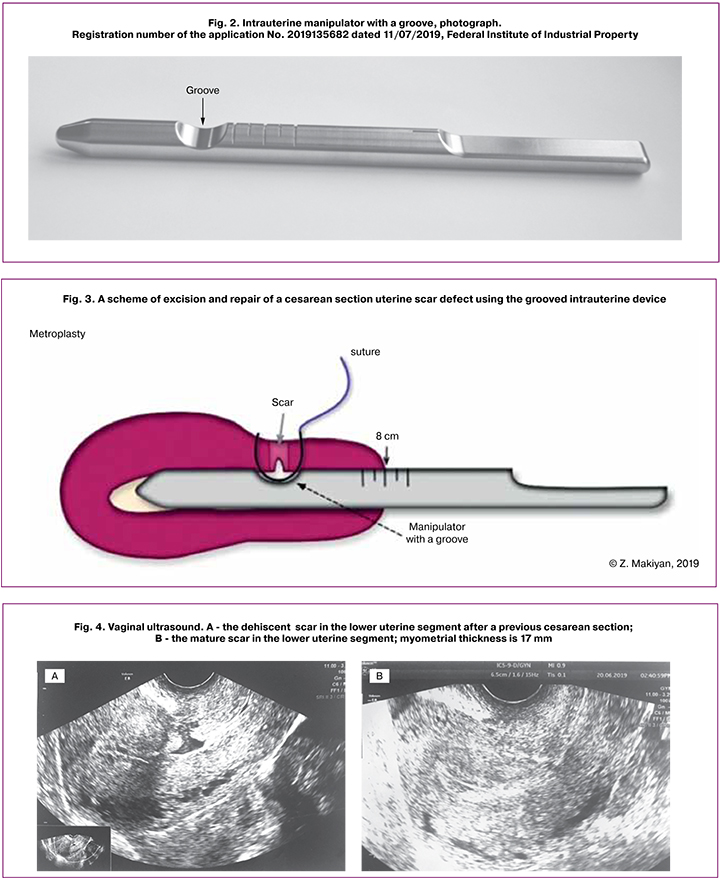
We designed a new intrauterine device with a groove1 for surgical treatment of uterine scar dehiscence (metroplasty), which (Fig. 1, 2) is a metal cylinder made of stainless steel: 190 mm long, 13 mm in diameter (there are also options with a smaller diameter - 12.0 mm and 12.5 mm), with an ogive-shaped rounded tip and a semi-cylindrical handle. At a distance of 40 mm to 58 mm (there is an option with a large distance from 50 mm to 68 mm) from the working part of the tip, there is a grooved recess 6 mm deep. The diameter of the groove is 18 mm and corresponds to the curvature of the needle used for sewing the scar (Fig. 3).
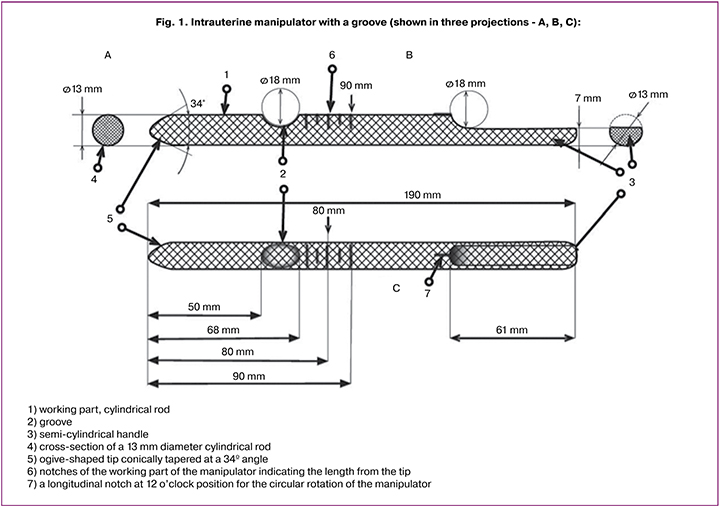
An intrauterine device is inserted into the uterine cavity through the cervical canal preliminary dilated with Geghar’s dilators.
The described above new method for surgical treatment of postoperative uterine scar dehiscence differs from existing metroplasty options in the following ways:
- an intrauterine manipulator with a groove is inserted directly under the postoperative uterine scar, which allows it to be optimally dissected and sutured through all layers;
- the postoperative scar excision is performed using mechanical scissors, immersing the scissors branch in the groove;
- the manipulator allows optimal approximation of wound edges for subsequent suturing;
- the uterine incision is closed by suturing techniques for all layers above the manipulator groove, which matches the curved sewing needle (atraumatic needle V-34 (36 mm);
- the manipulator has transverse notches indicating the length from the tip - 70, 80, 90 mm to limit the length of the manipulator insertion (corresponding to the length of the uterine cavity);
- to optimize the excision and its closure, the manipulator can be rotated around its axis to place the groove directly under the manipulation zone (if necessary, it can be located at the 10 - 12 or 2 o’clock position).
Case 1. A 38-year-old patient with a history of 3 caesarean deliveries presented with signs of uterine scar dehiscence. In 2017, she underwent laparoscopic repair of uterine scar dehiscence using a standard technique and an ultrasonic scalpel.
Ultrasonography (Fig. 4, A) showed a myometrial defect in the area of the postoperative scar with a niche sized 9mm × 3mm × 14mm and filled with menstrual detritus. The myometrial thickness over the niche was about 2 mm.
Conclusion: a myometrial defect in the area of the postoperative uterine scar, a history of uterine scar metroplasty.
Laparoscopy was performed using standard aseptic techniques and with pneumoperitoneum. A Karl Storz laparoscope and two lateral trocars were introduced into the abdominal cavity in the right iliac (Ø5mm) and left iliac (Ø12 mm) areas.
The uterus was enlarged to 5 - 6 weeks gestational size, spherical, pale pink in color, and was displaced posteriorly. On the anterior uterine wall, in the area of the vesicouterine fold, there was a post-caesarean section uterine scar. The scar was inverted and crater-shaped, up to 0.5 cm deep, up to 2 cm long, and up to 1.0 cm wide, and prolapsing at instrumental palpation. The right ovary measured 2.5×2.0×1.5 cm and had expressed follicles. The left ovary measuring 3×2.5×2.0 cm was fixed to the pelvic wall and had expressed follicles. The fallopian tubes on both sides were free throughout; fimbriae were expressed. Chromopertubation showed that both fallopian tubes were patent.
Hysteroscopy revealed a niche along the front and side walls of the upper third of the cervical canal. The niche had an irregular shape and was about 8 mm deep, about 10 mm wide, and about 20 mm long (from 10 to 2 o’clock position). The inner walls of the niche were irregular and had atrophic mucosa, pronounced vascular pattern, and cystic inclusions. Description of the procedure (Fig. 5, A – E).
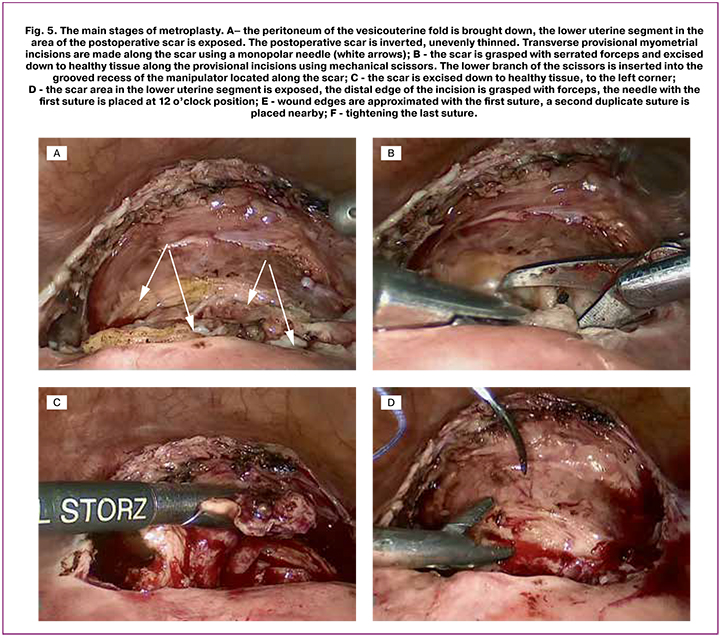
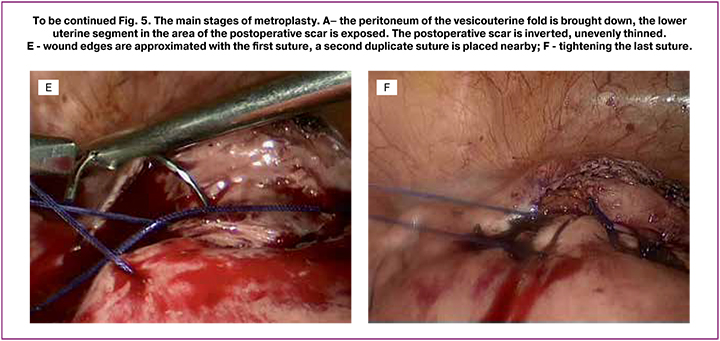
The cervical canal was dilated to Geghar’s No.12. An intrauterine grooved manipulator with a diameter of 12 mm was inserted. The peritoneum was opened in the region of the vesicouterine fold (plica vesicouterina). The urinary bladder, which was intimately fixed to the scar, was separated by blunt and sharp dissection. The lower uterine segment around the postoperative scar was exposed. Provisional myometrial incisions about 2 mm in depth were made along the proximal and distal edges of the scar using a monopolar needle. The scar was grasped by a serrated forceps and excised down to healthy tissue along the provisional incisions. The groove of the intrauterine device was exposed.
The edges of the wound were approximated above the groove and closed with three “duplicate” vicryl sutures. The second row of sutures consisted of submersible serous-muscular vicryl sutures. Peritonization was performed by a continuous suture using the peritoneum of the vesicouterine fold. Hemostasis was achieved by a bipolar coagulator. After a final check for hemostasis, the skin was closed with skin sutures and a sterile adhesive bandage.
The follow-up ultrasound (Fig. 4, B) 3 months after surgery showed that the myometrial thickness of the lower uterine segment in the scar area was 17 mm and had a homogeneous structure.
The complexity of repair of uterine scar dehiscence is mostly attributable to anatomical and topographic features including location of the lower uterine segment with the scar under the vesicouterine fold of the parietal peritoneum or urinary bladder; immediate proximity in the ascending uterine vessels; and the need to verify the area of uterine scar and determine the boundaries of scar excision within healthy tissue.
In some cases, the outcome of uterine scar defect repair depends on the probability of cervical epithelium invagination into the niche with the formation of pseudocysts or ectopic endometrial lesions (endometriosis) [19–22].
Conclusion
The newly proposed method for surgical treatment of uterine scar dehiscence after a previous caesarean section using the grooved intrauterine device allows for effective restoration of the lower uterine segment due to the optimization of metroplasty at all stages.
The results of metroplasty depend on adequate excision of the dehiscent scar down to healthy myometrium, an optimal approximation of wound edges, and myometrial suturing. The scar excision through the groove of the manipulator using mechanical scissors and closing wound edges over the groove provides the best conditions for the uterine defect repair.
The method of repair of uterine scar dehiscence using a new intrauterine manipulator with a groove can be recommended for routine clinical application and may be further optimized in the process.
References
- Vogel J.P., Betrán A.P., Vindevoghel N., Souza J.P., Torloni M.R., Zhang J., et al. WHO Multi-Country Survey on Maternal and Newborn Health Research Network. Use of the Robson classification to assess caesarean section trends in 21 countries: a secondary analysis of two WHO multicountry surveys. Lancet Global Health. 2015; 3(5): e260–70. doi: 10.1016/S2214-109X(15)70094-X.
- Еремкина В.И., Гарифуллова Ю.В. Реконструктивно-восстановительная пластика несостоятельного рубца на матке влагалищным доступом вне беременности. Практическая медицина. 2014; 4: 46–8. [Eremkina V.I., Garifullova Yu.V. The reconstructive-plastic surgery of the inconsistent scar on the uterus via vaginal access in the absence of pregnancy. Prakticheskaya meditsina. 2014; 4: 46–8. (in Russian)]. eLIBRARY ID: 21845031
- Robson M., Hartigan L., Murphy M. Methods of achieving and maintaining an appropriate caesarean section rate. Best Pract Res Clin Obstet Gynaecol. 2013; 27: 297–308. doi: 10.1016/j.bpobgyn.2012.09.004.
- Коган О.М., Войтенко Н.Б., Зосимова Е.А., Мартынова Э.Н., Нерсесян Д.М., Бубникович А.А. Алгоритм ведения пациенток с несостоятельностью послеоперационного рубца на матке после кесарева сечения. Клиническая практика. 2018; 3(9): 38–43. [Kogan O.M., Voytenko N.B., Zosimova E.A., Martynova E.N., Nersesayn D.M., Bubnikovich A.A. Algorithm for the management of patients with incompetence of postoperative uterine scar after a cesarean section. Klinicheskaya praktika. 2018; 3(9): 38–43. (in Russian)]. doi: 10.17816/clinpract09338-43
- Буянова С.Н., Пучкова Н.В. Несостоятельный рубец наматке после кесарева сечения: диагностика, тактика ведения, репродуктивный прогноз. Российский вестник акушера-гинеколога. 2011; 4: 36–8. [Buyanova S.N., Puchkova N.V. Aninconsistent uterine scar after caesarean section: diagnosis, management tactics, reproductive prognosis. Rossiiskii vestnikakushera-ginekologa. 2011; 4: 36–8. (in Russian)].
- Манухин И.Б., Мурашко А.В., Мынбаев О.А. Повторное кесарево сечение с хирургической позиции: систематический обзор. Журнал акушерства и женских болезней. 2011; 60 (Спецвыпуск): 69–70. [Manukhin I.B., Murashko A.V., Myinbaev O.A. Repeated cesarean section from surgical position: systemic review. Zhurnal akusherstva i zhenskih bolezney. 2011; 60(Special issue): 69-70. (in Russian)].
- Глухов Е.Ю., Обоскалова Т.А., Столин А.В. и др. Рубец на матке после кесарева сечения в клинике и эксперименте. Российский вестник акушера-гинеколога. 2014; 1: 10–8. [Glukhov E. Iu., Oboskalova T.A., Stolin A.V., Spirin A.V., Butunov O.V. Post-cesarean section uterine scar in clinical and experimental settings Russian Bulletin of Obstetrician-Gynecologist/Rossiyskiy vestnik akushera-ginekologa. 2014;14(1): 10–8. (in Russian)]
- Краснопольская К.В., Попов А.А., Чечнева М.А., Федоров А.А., Ершова И.Ю. Прегравидарная метропластика по поводу несостоятельного рубца на матке после кесарева сечения: влияние на естественную фертильность и результаты ЭКО. Проблемы репродукции. 2015; 21(3): 56-62. [Krasnopol’skaya K.V., Popov A.A., Chechneva M.A., Fedorov A.A.,Ershova I.Yu. Caesarian section: the influence on natural fertility and IVF outcomes. Russian Journal of Human Reproduction/Problemy reproduktsii. 2015; 21(3): 56–62. (in Russian)]. https://doi.org/10.17116/repro201521356-62
- Mathai M., Hofmeyr G.J., Mathai N.E. Abdominal surgical incisions for caesarean section. Cochrane Database Syst Rev. 2013; (5): CD004453. doi: 10.1002/14651858.CD004453.pub3.
- Bij de Vaate A.J., Brolmann H.A., van der Voet L.F., van der Slikke J.W., Veersema S., Huirne J.A. Ultrasound evaluation of the Cesarean scar: relation between a niche and postmenstrual spotting. Ultrasound Obstet Gynecol. 2011; 37(1): 93–9. doi: 10.1002/uog.8864.
- van der Voet L.F., Bij de Vaate A.M., Veersema S., Brolmann H.A., Huirne J.A. Long-term complications of caesarean section. The niche in the scar: a prospective cohort study on niche prevalence and its relation to abnormal uterine bleeding. BJOG. 2014; 121(2): 236–44. doi: 10.1111/1471-0528.12542.
- van der Voet L.F., Jordans I.P.M., Brölmann H.A.M., Veersema S., Huirne J.A.F. Changes in the Uterine Scar during the First Year after a Caesarean Section: A Prospective Longitudinal Study. Gynecol Obstet Invest. 2018; 83(2):164–70. doi: 10.1159/000478046.
- Timor-Tritsch I.E., Monteagudo A., Santos R., Tsymbal T., Pineda G., Arslan A.A. The diagnosis, treatment, and follow-up of cesarean scar pregnancy. Am J Obstet Gynecol. 2012; 207(1): 44. e41-13. doi: 10.1016/j.ajog.2012.04.018.
- Sholapurkar S.L. Surgical techniques at caesarean might modify placenta accreta risk. BJOG. 2015;122(1):143. doi: 10.1111/1471-0528.13017.
- Международная классификация болезней 10 пересмотра (МКБ-10).[International Classification of Diseases 10th Revision (ICD-10). (in Russian)] https://icd.who.int/browse10/2016/en#/O30-O48
- Nikkels C., Vervoort A., Mol B.W., Hehenkamp W.J.K., Huirne J.A.F., Brolmann H.A.M. IDEAL framework in surgical innovation applied on laparoscopic niche repair. Eur J Obstet Gynecol Reprod Biol. 2017; 215: 247–53. doi: 10.1016/j.ejogrb.2017.06.027.
- Sumigama S., Sugiyama C., Kotani T., Hayakawa H., Inoue A., Mano Y., Tsuda H., et al. Uterine sutures at prior caesarean section and placenta accreta in subsequent pregnancy: a case-control study. BJOG. 2014; 121(7): 866–74. doi: 10.1111/1471-0528.12717. discussion 875.
- Abalos E., Addo V., Brocklehurst P., El Sheikh M., Farrell B., Gray S., Hardy P., et al. Caesarean section surgical techniques (CORONIS): a fractional, factorial, unmasked, randomised controlled trial. Lancet. 2013; 382(9888): 234–48. doi: 10.1016/S0140-6736(13)60441-9.
- Marotta M.L., Donnez J., Squifflet J. et al. Laparoscopic repair of post-cesarean section uterine scar defects diagnosed in nonpregnant women. J Minimal Invasive Gynecol. 2013; 20(3): 386–91. doi: https://doi.org/10.1016/j.jmig.2012.12.006
- Makiyan Z. Endometriosis origin from primordial germ cells. Organogenesis. 2017; 13(3): 95–102. doi.org/10.1080/15476278.2017.1323162
- Makiyan Z. New theory of uterovaginal embryogenesis. Organogenesis 2016; 12(1): 33–41; doi.org/10.1080/15476278.2016.1145317
- Xu W., Wang M., Li J., Lin X., Wu W., Yang J. Laparoscopic combined hysteroscopic management of cesarean scar pregnancy with temporary occlusion of bilateral internal iliac arteries: A retrospective cohort study. Medicine (Baltimore). 2019; 98(37): e17161. doi:10.1097/MD.0000000000017161.
Received 16.10.2019
Accepted 29.11.2019
About the Authors
Makiyan Zograb Principal Investigator, Doctor of medicine. National Medical Research Center for Obstetrics, Gynecology and PerinatologyCorresponding author http://orcid.org/0000-0002-0463-1913
Adamyan Leyla V. Academician of RAS, professor, doctor of medicine. Head op operative gynecology. National Medical Research Center for Obstetrics, Gynecology and Perinatology
Karabach Valeriy V. MD, head of operation room. National Medical Research Center for Obstetrics, Gynecology and Perinatology
Chuprynin Vladimir D. MD, Head of surgical department. National Medical Research Center for Obstetrics, Gynecology and Perinatology
Zohrab N. Makiyan, MD, Leading Researcher, Department of Operational Gynecology, Federal State Budgetary Institution National Medical Research Center for Obstetrics, Gynecology and Perinatology named after V.I. Kulakova “Ministry of Health of Russia. E-mail: makiyan@mail.ru; http://orcid.org/0000-0002-0463-1913
117997, Russia, Moscow, Ac. Oparina str. 4.
Leyla V. Adamyan, MD, academician of the Russian Academy of Sciences, professor, head of the department of operative gynecology of the National Medical Research Center of Obstetrics, Gynecology and Perinatology named after V.I. Kulakova Ministry of Health of Russia. E-mail: aleyla@inbox.ru
117997, Russia, Moscow, Ac. Oparina str. 4.
Valery V. Karabach, PhD, head. operating unit of the Federal State Budgetary Institution National Medical Research Center of Obstetrics, Gynecology and Perinatology named after V.I. Kulakov, Ministry of Health of Russia.
Address: 117997, Russia, Moscow, ul. Academician Oparin, d. 4.
Vladimir D. Chuprynin, PhD, Head of the Surgery Department, National Medical Research Center of Obstetrics, Gynecology, and Perinatology named
after Academician V.I. Kulakov, Ministry of Health of Russia. Tel.: +7(495)438-3575. E-mail: v_chuprynin@oparina4.ru
117997, Russia, Moscow, Ac. Oparina str. 4.
For citation: Makiyan Z.N., Adamyan L.V., Karabach V.V., Chuprynin V.D.
A new method for surgical treatment of uterine scar insuffisiency after
a previous cesarean section using an intrauterine manipulator with a groove.
Akusherstvo i Ginekologiya/ Obstetrics and gynecology. 2020; 2: 104-110 (In Russian).
https://dx.doi.org/10.18565/aig.2020.2. 104-110